Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.12 Madrid dic. 2016
https://dx.doi.org/10.17235/reed.2016.3897/2015
Spontaneous retroperitoneal hematoma in a patient under anticoagulant agents presenting as upper gastrointestinal bleeding
Hemorragia digestiva alta como forma de presentación de hematoma retroperitoneal espontáneo gigante secundario a anticoagulación en una mujer con reordenación del gen JAK2
Gabriel Carrilero-Zaragoza1, Juan Egea-Valenzuela1, María Moya-Arnao2, María Muñoz-Tornero1, Roxanna Jijón-Crespín1, Paula Tomás-Pujante1, Elena Iglesias-Jorquera1, Josefa Parra-García3, Eduardo Sánchez-Velasco1, Ana Pereñíguez-López1, Manuel Miras-López1, Matilde Fuster-Quiñonero4 and Fernando Carballo-Álvarez1
Departments of 1Digestive Diseases, 2Hematology, 3Pathology, and 4Radiodiagnosis. Hospital Universitario Virgen de la Arrixaca. El Palmar, Murcia. Spain
ABSTRACT
We present the case of a 44-year-old woman with past history of repeated miscarriage and Budd-Chiari syndrome secondary to primary myelofibrosis. Because of this she was under treatment with oral anticoagulant agents. The patient was admitted in hospital as she presented with gastrointestinal bleeding (melena), asthenia and progressive anemia. In an initial upper endoscopy an extrinsic duodenal compression associated with an ulcer on the posterior face of the first portion of duodenum and upper duodenal knee was observed. In the following days a huge spontaneous retroperitoneal hematoma due to anticoagulation was diagnosed by computed tomography. This was treated with a percutaneous drainage and withdrawal of the antithrombotic drugs. The evolution of the patient was initially satisfactory but she suffered subclavian and jugular vein thrombosis, and reintroduction of anticoagulant agents at the lowest therapeutic doses was required.
Key words: JAK-2. Duodenal ulcer. Retroperitoneal hematoma. Gastrointestinal bleeding.
RESUMEN
Presentamos el caso de una mujer de 44 años de edad con antecedentes de abortos de repetición y síndrome de Budd-Chiari secundario a una mielofibrosis primaria en tratamiento anticoagulante. Consulta por melenas y astenia, presentando anemización progresiva. En una gastroscopia inicial se aprecia una compresión extrínseca a nivel supraampular de segunda porción duodenal, con una úlcera asociada en cara posterior de bulbo y primera rodilla. Posteriormente se diagnostica mediante una tomografía computarizada de un hematoma retroperitoneal espontáneo secundario a anticoagulación. Se trata con drenaje percutáneo y retirada de anticoagulación con buena respuesta inicial. No obstante, presenta complicaciones trombóticas (trombosis subclavia y yugular) y se reintroducen los anticoagulantes con dosis en el límite bajo del rango terapéutico.
Palabras clave: JAK-2. Úlcera duodenal. Hematoma retroperitoneal. Hemorragia digestiva alta.
Introducción
The manifestations of duodenal ulcer can be variable, from a simple dyspeptic syndrome or abdominal pain, up to upper gastrointestinal bleeding manifesting as hematemesis or melena. In a high number of cases, duodenal ulcer can be secondary to Helicobacter pylori infection or nonsteroidal anti-inflammatory drugs (NSAIDs) intake, but other not so frequent causes have been also described in literature, such as tumors and ischemia or mechanic ulcers due to extrinsic compression of the duodenum (1).
Case report
We present the case of a 44-year-old woman who was admitted to our hospital because of severe epigastric pain and melena. The patient was under follow-up in the Departments of Digestive Diseases and Hematology. In the past, she presented with repeated miscarriage and Budd-Chiari syndrome, and different morphological and genetic studies, as well as bone marrow biopsy, were carried out with a final diagnosis of prefibrotic stage of primary myelofibrosis (Fig. 1) and heterozygous JAK-2 (V617F) mutation.
The patient was under oral anticoagulant agents (acenocoumarol) and had been included in waiting list for liver transplantation due to chronic liver failure.
During her admission, significative anemia (Hb: 9.2 g/dl) and INR: 1 were observed. As the patient presented with melena an upper endoscopy was performed, finding an ulcer on the posterior face of the first portion of duodenum and superior duodenal flexure, with mild active bleeding. This lesion was treated endoscopically with submucosal adrenaline injection and placement of hemostatic clips. Thickened folds were also observed on the supra-ampullary area of the second duodenal portion (Fig. 2).
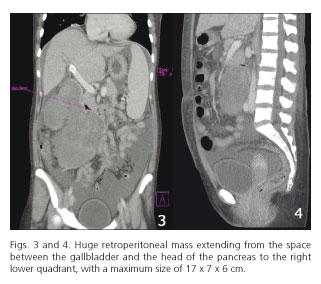
After 48 hours, the patient presented worsening of her situation and drop of hemoglobin levels, so a new upper endoscopy was carried out. Great gastric retention was observed, but no gastric lesions, and pylorus was patent. On the second portion of the duodenum, a big bulge on the wall caused a complete stenosis. After this, an abdominal computed tomography was done, finding a huge, heterogeneous and multilobulated mass in the retroperitoneal space and the root of the mesentery, suggesting a hematoma. The upper part of the hematoma was located between the gallbladder and the head of the pancreas, under the duodenum, which was completely compressed by the mass. A big lobulation of the hematoma (12 x 9 x 11 cm) grew from this upper part downstream and ahead of the aorta, cava and right psoas getting to the abdominal right lower quadrant, with a maximum size of 17 x 7 x 6 cm (Figs. 3 and 4).
With all these findings, anticoagulant agents were withdrawn. An arteriography did not find a point of bleeding but a radiologic drainage was placed. The patient remained stable, with no new drops in hemoglobin or external signs of gastrointestinal bleeding. However, after withdrawal of anticoagulants she suffered subclavian and jugular vein thrombosis and the specialists from the Departments of Digestive Diseases and Hematology agreed to restart anticoagulation at the lower limits of therapeutic range.
Nowadays, some months after the episode, the patient remains in a good clinical situation and in the waiting list for liver transplantation.
Discussion
Melena is the typical clinical presentation of upper gastrointestinal bleeding secondary to duodenal ulcer. In most of the cases this is related to Helicobacter pylori infection of NSAIDs intake, and ischemia or extrinsic compression of the duodenal wall are rare etiological factors. Association between oral anticoagulant agents and spontaneous retroperitoneal hematoma, as it occurred in our patient, has been previously described (2). This retroperitoneal hematoma caused compression and ulceration of the duodenal wall in our patient, and this ulcer and the consequent gastrointestinal bleeding were the first clinical manifestations of the retroperitoneal hematoma.
References
1. Naylor RG, Juler GL. Congenital causes of duodenal ulcers in adults. Arc Surg 1976;111:658-62. DOI: 10.1001/archsurg.1976.01360240038006. [ Links ]
2. Sunga KL, Bellolio MF, Gilmore RM, et al. Spontaneous retroperitoneal hematoma: Etiology, characteristics, management, and outcome. J Emerg Med 2012;43:e157-61. DOI: 10.1016/j.jemermed.2011.06.006. [ Links ]
![]() Correspondence:
Correspondence:
Gabriel Carrilero Zaragoza.
Department of Digestive Diseases.
Hospital Universitario Virgen de la Arrixaca.
Ctra. Madrid-Cartagena, s/n.
30120 El Palmar, Murcia. Spain
e-mail: gcarrileroz88@gmail.com
Received: 30-07-2015
Accepted: 14-09-2015











 texto en
texto en