Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.6 Madrid jun. 2017
https://dx.doi.org/10.17235/reed.2017.4748/2016
ORIGINAL PAPERS
Knowledge of disease and access to a specialist reported by Spanish patients with ulcerative colitis. UC-LIFE survey
Conocimiento de la enfermedad y acceso al especialista descrito por pacientes españoles con colitis ulcerosa. Encuesta UC-LIFE
Federico Argüelles-Arias1, Daniel Carpio2, Xavier Calvet3, Cristina Romero4, Luis Cea-Calvo4, Berta Juliá4 and Antonio López-Sanromán5
1Joint Unit of Clinical Management - Digestive Diseases. Hospitales Virgen Macarena-Rocío. Sevilla, Spain.
2Department of Gastroenterology. Complexo Hospitalario Universitario de Pontevedra. Instituto de Investigación Biomedica (IBI). SERGAS. Pontevedra, Spain.
3Departament of Medicine. Universitat Autònoma de Barcelona. Unitat de Malalties Digestives. Corporació Sanitaria Universitària Parc Taulí. Sabadell, Spain; Centro de Investigación Biomédica en Red de enfermedades hepáticas y digestivas (CIBERehd). Madrid, Spain.
4Medical Department. Merck Sharp & Dohme. Madrid, Spain.
5Gastroenterology Unit. Department of Gastroenterology and Hepatology. Hospital Universitario Ramón y Cajal. Madrid, Spain
This study was funded by Merck Sharp & Dohme de España, a subsidiary of Merck & Co., Whitehouse Station, New Jersey, USA, and was endorsed by the Confederation of Associations for Patients with Crohn's and Ulcerative Colitis of Spain (ACCU; www.accuesp.com.es).
Conflicts of interest: F. Argüelles-Arias has provided services as a speaker, consultant or advisor, or has received research funding from Merck Sharp & Dohme, AbbVie, Takeda, Tillotts, Kern-Pharma, Faes Farma, Shire Pharmaceuticals, Gebro Pharma, and Vifor Pharma. D. Carpio has provided services as a consultant for Merck Sharp & Dohme, AbbVie, Pfizer and UCB Pharma, has received speaker fees from Merck Sharp & Dohme, AbbVie, Pfizer, Takeda, Shire, Gebro Pharma, Tillotts, Dr Falk Pharma, and Almirall, and has been involved in clinical research for Merck Sharp & Dohme, AbbVie and Tygenix. X. Calvet has provided services as a speaker, consultant and advisor, or has received research funding from Merck Sharp & Dohme, AbbVie, Hospira, Pfizer, Faes Farma, Shire Pharmaceuticals, Gebro Pharma, Otsuka Pharmaceutical, and Vifor Pharma. C. Romero, B. Julia and L. Cea-Calvo are full-time employees of the Medical Department of Merck Sharp & Dohme Spain. A. López-Sanromán has provided services as a speaker, consultant or advisor for Merck Sharp & Dohme, AbbVie, Hospira, Gebro Pharma, Faes Farma, Shire Pharmaceuticals, Takeda, and Tillotts.
ABSTRACT
Background and aim: Education of patients with ulcerative colitis (UC) about their disease and access to a specialist are important to improve health outcomes. Our objective was to determine, by collecting information directly from the patients, their information sources and knowledge of the disease, and the options for access to the gastroenterologist.
Methods: The information was collected using a printed survey handed out by 39 gastroenterologists to 15 consecutive adult patients with UC. Patients answered anonymously from their home. The responses were stratified by hospital size (> 900; 500-900; < 500 beds).
Results: A total of 585 patients received the survey and 436 responded (74.5%; mean age of 46 years [13.5], 53% men). The main information source was the specialist physician (89.2%). Between 32% and 80% of patients had areas of improvement regarding knowledge of their disease. Knowledge of the disease was better in patients from small hospitals (< 500 beds). The frequency of routine visits was also higher in small hospitals. In case of a flare-up, 60% stated they were able to contact their doctor by phone and 37%, that they could get an appointment on the same day. The percentage stating that they had to ask for an appointment and wait until their physician was available was lower in small hospitals.
Conclusions: There are areas of improvement with regard to knowledge of their disease in patients with UC followed in hospital clinics. Patients followed in small hospitals seem to know their disease better, are followed more frequently in the clinic, and have better access in case of a flare-up.
Key words: Ulcerative colitis. Self-management. Information sources. Knowledge of disease. Access to physician.
RESUMEN
Antecedentes y propósito: la educación de los pacientes con colitis ulcerosa (CU) sobre su enfermedad y el acceso al especialista es importante para mejorar los resultados en salud. Nuestro objetivo fue conocer, recogiendo información directamente de los pacientes, sus fuentes de información y su conocimiento de la enfermedad, y las posibilidades de acceso al especialista en gastroenterología.
Métodos: la información fue recogida mediante encuesta impresa, entregada por 39 gastroenterólogos a 15 pacientes adultos consecutivos con CU. Los pacientes contestaron de forma anónima desde su domicilio. Las respuestas se estratificaron según el tamaño del hospital (> 900; 500-900; < 500 camas).
Resultados: quinientos ochenta y cinco pacientes recibieron la encuesta y 436 contestaron (74,5%; edad media 46 años (13,5), 53% hombres). La principal fuente de información fue su médico especialista (89,2%). Entre un 32% y un 80% presentaron áreas de mejora en el conocimiento de su enfermedad. El conocimiento de la enfermedad fue mejor en pacientes de hospitales pequeños (< 500 camas). La frecuencia de revisiones rutinarias fue mayor también en hospitales pequeños. Ante empeoramiento, el 60% declaró poder contactar por teléfono con su médico y el 37%, conseguir cita el mismo día. El porcentaje que declaró tener que pedir cita y esperar disponibilidad fue menor en hospitales pequeños.
Conclusiones: en pacientes con CU seguidos en consultas hospitalarias, existen áreas de mejora en el conocimiento de su enfermedad. Los pacientes seguidos en hospitales pequeños parecen conocer mejor su enfermedad, son seguidos con más frecuencia en la consulta y tienen mejor acceso en caso de empeoramiento.
Palabras clave: Colitis ulcerosa. Automanejo. Fuentes de información. Conocimiento de la enfermedad. Acceso al médico.
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease of unknown cause in which both genetic and environmental factors are involved. The rectal mucosa is always affected, and extension, which is always continuous from the rectum and in the proximal direction, varies from patients with rectal involvement only (proctitis) to patients with disease in the entire colon (1,2).
The chronic relapsing nature of UC, its socially stigmatizing symptoms, and its most common onset in the second decade of life trigger profound changes in the life of patients from the time of diagnosis (3,4). Added to the physical impact of the symptoms are the effects on the patient psyche from the impact of the disease on social, work and emotional relationships, which eventually leads to impaired quality of life of these patients (5-9).
All the above justifies why patient-physician communication is a vital element in the care process of these patients, where the construction of collaborative relationships between both becomes a key element to achieve optimal management of the disease (10,11). Efficient physician-patient communication contributes to the achievement of better health outcomes and has been significantly associated with better treatment adherence (12-14).
An adequate knowledge of the disease by UC patients will enable them to better face their disease and the possibilities for self-management. Two especially sensitive periods for the patient when the need for information and/or education is greatest are after diagnosis and at the time of relapse (15). The most relevant areas of information for patients after diagnosis are related to symptoms, possible complications, etiology, long-term course, risk of cancer, and the impact of the disease and treatments on fertility (11).
The UC-LIFE survey was conducted in a large sample of UC patients followed in hospital throughout Spain in order to determine their perceptions, points of view and opinions on the experience of living with UC. The description of the survey and the results on the perception of the symptom burden and emotional impact of the disease have been previously published (16,17). The objective of this study was to determine, by collecting information directly from UC patients, their information sources and knowledge of the disease and the ease with which they can access the gastroenterologist (frequency of visits to a specialist and options for contacting the specialist in case of a flare-up).
Methods
UC-LIFE was a cross-sectional survey of UC patients that was conducted between June and September 2014. Patients followed in gastroenterology clinics of 38 Spanish hospitals participated in the survey. Regarding the size of the participating hospitals, the different types that were representative of the network of public hospitals in Spain was taken into account (> 900 beds [37%], n = 14; 500-900 beds [34%], n = 13; < 500 beds [29%], n = 11).
Participants and procedures
Thirty-nine gastroenterologists handed out the survey to 585 adult patients with UC. To prevent selection bias, each physician handed out the survey consecutively to the first 15 UC patients who routinely attended the clinics, irrespective of the severity of the disease or any other criterion. Patients received instructions to read and answer the questionnaire anonymously and voluntarily from their home, returning the completed questionnaire by mail in a prepaid envelope with the address of the agency in charge of tabulation and analysis of the data. No reminder was made to complete the survey and the physicians did not collect any data from the patients' medical history.
Instrument used for the survey
The UC-LIFE survey was created with the participation of three expert physicians in the treatment of inflammatory bowel disease (IBD), and was reviewed by three patients belonging to the Confederation of Associations for Patients with Crohn's and Ulcerative Colitis of Spain (ACCU) to ensure that the questions and language used were appropriate and understandable. The questionnaire consisted of 44 closed and multiple-choice questions that requested information about the following aspects: demographic characteristics, perception of symptom burden and severity of the disease during the previous year, social and emotional impact due to UC in everyday life, the most important treatment attributes for patients and satisfaction with current treatment and physician behaviors' during the medical interview. In addition, questions were included about the main information sources for patients, knowledge of the disease (through a series of statements which the patients had to respond to by agreeing or not with them), frequency of visits to the physician in the last year, frequency of routine visits and options for access to the specialists in case of a flare-up. The complete survey is available as an appendix to the main publication (16).
Statistical considerations
UC-LIFE was a survey of an exploratory nature and no formal hypotheses or sample sizes were established. Quantitative variables are expressed as mean and standard deviation (SD) or median and interquartile range (IQR) if the data did not follow a normal distribution. Qualitative variables are described as frequencies or percentages. Comparisons were made according to the symptom burden and interference with everyday life during the previous year, and hospitals were stratified by size based on the number of beds: A (> 900 beds), B (500-900 beds) and C (< 500 beds). Student's t-test was used for simple bivariate comparisons or between independent groups. The Chi-squared or Fisher's exact test were used to compare proportions. Multiple comparisons between subgroups were performed using the minimum significant difference test. Missing values were not imputed. Given the basically descriptive nature of the results, no adjustments for multiplicity were made. A p-value ≤ 0.05 was considered to be statistically significant. Statistical analysis was performed using SPSS software version 18.0.0.
Ethical considerations
The survey was reviewed and approved by the Ethics Committee of the Hospital Parc Taulí, Barcelona (Spain), and by the Confederation of Associations for Patients with Crohn's and Ulcerative Colitis of Spain (ACCU).
The documentation accompanying the survey provided the patient with information about the anonymous nature of the survey and the pooled processing of the data, thus ensuring that patient identification was not possible. Sending of the completed survey by the patient was considered as consent to participate.
Results
Demographic characteristics
The survey was handed out to 585 patients and 436 returned it completed (response rate: 74.5%). By hospital size, 35.8% of patients were from large hospitals (> 900 beds), and 34.8% and 29.4% were from medium (900-500 beds) and small hospitals (< 500 beds), respectively. The mean age of respondents was 46.2 (SD 13.6) years, and 52.8% of them were men. The median duration of the disease was eight (IQR: 4-15) years. Demographic characteristics are described in table I. Overall, 47.1% of patients indicated that their symptoms had been controlled during the previous year, and 28.0% and 24.9%, respectively, reported having had "symptoms with no impact on everyday life" and "symptoms with impact on everyday life".
Patients' information sources and knowledge of disease
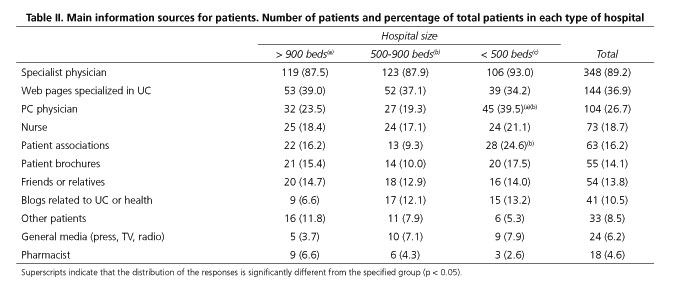
The most frequently cited information sources by patients were the specialist physician (89.2%), web pages specialized in UC (36.9%) and the Primary Care (PC) physician (26.7%) (Table II). The vast majority of patients indicated the specialist physician as the most important source (93.0%). When information sources were analyzed by hospital size, patients treated in smaller hospitals mentioned more frequently the PC physician and patient associations than those treated in larger hospitals (Table II).
Nearly three quarters of patients stated that their physician always or nearly always provided them information about the causes, the possible course of the disease and the different treatment options (70.8%, 69.1% and 72.5%, respectively). The frequency with which patients agreed with each of the above statements was significantly higher in smaller hospitals compared to medium or large hospitals (Fig. 1).
Based on the correct responses given by patients on specific statements about UC, the large majority seem to have an adequate knowledge of the relapsing and noncontagious nature of the disease or the need for lifelong treatment, with percentages of 88.2%, 93.2% and 88.2%, respectively. However, between 32% and 40% of patients showed an erroneous belief or no knowledge about aspects related to the incurable nature of the disease (32.4%), the role of diet (30.5%) or the possibility of involvement of other organs in addition to the intestine (40.0%). The areas of knowledge of the disease in which a larger percentage marked erroneous responses or indicated no knowledge were related to the hereditary nature of UC and the role of stress in the origin of the disease, at 61.6% and 80.4%, respectively.
In the subgroup analysis by hospital size, the percentage of patients with correct responses about UC in smaller hospitals was generally higher than in medium and large hospitals. Specifically, in questions on the incurable nature of the disease and the role of diet and stress in the development of UC, a significantly higher percentage of patients responded correctly in small hospitals compared to large hospitals (Fig. 2).
Follow-up in a hospital clinic and access in case of flare-up
With regard to the frequency in which patients attended their specialist clinic during the previous year, 40.6%, 44.9% and 14.4% attended 0-2 times, 3-5 times and > 5 times, respectively (n = 394). Almost half of patients (47.2%) stated that they agreed with their physician to have routine visits every 2-3 months, 36.1% and 14.1% every six months or every year, respectively, and only 2.3% did not agree on routine visits.
Patients from smaller hospitals reported a significantly higher frequency of routine visits compared to those from medium and large hospitals (Table III). According to the symptom control reported by patients during the previous year, the frequency of follow-up in patients whose symptoms had been controlled was significantly higher in smaller hospitals (Table III.2), whereas patients with symptoms in the previous year reported similar frequencies of follow-up in large, medium and small hospitals (Table III. 3 and 4).
In case of a clinical flare-up, the following options were stated by patients: telephone contact (59.6%), possibility of getting an appointment in the hospital on the same day (36.9%), and having to go to the Emergency Department (29.6%). Nearly a quarter of patients (21.0%) stated that they had to ask for an appointment and wait until their physician was available, and 15.1% said they could get in contact by e-mail. Patients from small hospitals reported more availability when contacting by phone or e-mail and a lower need to ask for an appointment and wait for their physician to be available (p < 0.05) (Fig. 3).
Discussion
The present study, based on the results of the UC-LIFE survey, complements other two studies which discussed different aspects dealt with in the survey about the perception of symptom burden of the disease, preferences and satisfaction with treatment (16) and the psychosocial impact perceived by the patient (17). This analysis provides relevant information on the knowledge that patients have about important aspects of their disease and about their follow-up and access to the gastroenterologist, and reveals significant differences in favor of patients who are followed in small hospitals.
Ulcerative colitis is a disease that affects all aspects of the individual's life and therefore patient education and a collaborative relationship with the physician are key aspects in achieving optimum results in terms of control of the disease and quality of life of the patient (12,13,18). In the UC-LIFE survey, patients highlighted the gastroenterologist as their main information source. Other studies have found similar results: the survey carried out by Rubin et al. in 451 UC indicated that, for 89% of patients, the gastroenterologist was their main information source (6). Likewise, Bernstein et al. found similar results in 74 IBD patients. In this last study, and in agreement with our results, the second most important information source for patients was the internet (11). In this regard, the physician's advice on adequate and reliable web pages which can help patients to improve their knowledge of the disease may be particularly useful for them.
In the present survey, only 19% of patients mentioned nursing staff as an information source. The reason is probably that not all clinics have nursing staff specialized in IBD, a valuable resource that has shown to be effective to inform patients about general aspects of their disease and enhance adherence to medication. Based on all this, nurses are now a cornerstone in the diagnosis and follow-up of these patients (19).
Sixteen percent of respondents considered patient associations as an important information source, and this percentage was significantly higher in patients treated at smaller hospitals (24%). Associations usually offer information and emotional support, which are important aspects for the patient, so referral of patients to these associations may be beneficial for them.
A significant number of participants seem to have erroneous beliefs about some aspects related to UC such as its chronic and incurable nature, transmission to offspring, the role of diet or stress on the development of the disease, or the possible occurrence of extraintestinal manifestations. An interesting finding is that patients treated in smaller hospitals seem in general to have a better knowledge of many of these aspects.
On the other hand, seven out of ten patients think that their physicians always or almost always inform them about their disease causes, course and possible treatment options, and once again patients most frequently report that their physicians deal with these issues in smaller hospitals. The extension and difficulty of the aspects to be discussed with the patient, especially at the time of the initial diagnosis, requires time, which is not always available within a routine visit. Therefore, in many cases it may be more efficient to schedule additional visits where, in addition to the explanations of the medical team, patients' concerns, information needs and opinions can be addressed. In this regard, drawing an educational plan that allows patients to answer their questions and acquire an adequate knowledge of their disease could be beneficial for most patients (10,11).
A patient-centered communication model which considers their opinions, understands their concerns and information needs, and takes into account pyschosocial aspects related to UC will help patients resolve their symptoms and feel more satisfied with the care they receive (10,18). In this regard, various studies have shown that educating patients to be more autonomous in the management of their disease can have a positive impact on the number of visits to the physician. Robinson et al. carried out a study in 203 UC patients in which the intervention group was trained in self-management of their UC and only went to the physician clinic when they thought it was necessary, while the control group received no training and followed the normal schedule of routine visits. Both groups were followed for a median of 14 months (IQR 11-18). In patients from the intervention group, treatment of a flare-up of their disease was much more rapid and they made significantly fewer visits to the hospital and PC physician (20). Kennedy et al. obtained similar results, with a reduction in the number of visits and an increase in patients' confidence after receiving a disease self-management training program (21). In line with the results of these studies, the IBD Unit of Hospital del Vall d'Hebron carried out a study with 393 patients who completed a questionnaire on the visits scheduling, the need for emergency treatment and the quality of the care they received, and were also asked for suggestions on how to improve the control of their disease. Ninety-eight percent of participants thought that information and knowledge of their disease could be useful to control it and 70% indicated that adequate information could help them to start treatment before visiting the physician (22). In fact, the reasons for visiting the physician were more often related to the patient's emotional health than to the disease itself, and therefore a more patient-centered model, where patients are appropriately educated about their disease and participate more actively in their care, may be also beneficial to the healthcare system (23-25).
In this patient sample, nearly half of them had visited their specialist physician 3-5 times during the previous year, agreeing with him/her on routine visits every 2-3 months. This frequency was significantly higher in smaller hospitals, and it is striking that this higher frequency seems to occur in patients who state that their UC is controlled, without symptoms. The reasons for this discrepancy cannot be deduced from the survey data, but they may be related at least in part to a different care load, which in turn determines the frequency of patient appointments. One consideration in this respect is that certain patients, particularly those who reported having been controlled in the last year, could be followed more efficiently with fewer visits to the hospital. Regarding this, in the CRONICA-UC study, the SCCAI questionnaire for UC patients was recently validated for its remote use from the patient's home via a web page, with a good correlation to the questionnaire evaluated by the physician in the hospital clinic (26). The negative predictive value for active disease was very high (95%), suggesting that patients in a stable status of the disease could benefit from a more flexible follow-up, with remote evaluations and fewer visits to the hospital clinic.
Nearly 60% of patients mentioned their possibility to contact their physician by phone in case of flare-up, and 37% could get an appointment in the hospital on the same day. These figures suggest a high availability of the specialist, consistent with the importance of being able to contact the physician rapidly at the time of a relapse in order to optimize treatment as soon as possible. It should be noted that in smaller hospitals patients can contact their physicians by phone or e-mail more frequently than in medium or large hospitals, and that they have to ask for an appointment and wait until their physician is available less frequently, though there are no differences between hospitals regarding their size in terms of the possibility of getting a hospital appointment on the same day.
Our study has a number of limitations. First, information is collected from the patient's self-assessment, and the findings commented upon should be understood as the patients' perceptions, which are valuable as they reflect how patients live their disease. Second, the participants reported on an extended time period of one year, and therefore their responses may be affected by recall bias. The survey was handed out to patients followed in hospital clinics, therefore, participants in the survey are not necessarily representative of the whole population of UC patients. Handing out the survey to consecutive patients may increase the likelihood of including patients with more severe disease, who tend to attend the clinics more frequently; however, this also reduces patient selection bias by the physicians. This fact may partly explain the high frequency of visits reported by these patients in the survey (nearly half stated being seen every 2-4 months). The survey was distributed in three types of hospitals according to their size, but no information was collected on whether the patients came from hospitals with IBD units or specialized nurses, which could influence the way in which patients are treated or followed, and therefore their responses. Finally, the anonymous nature of the survey does not allow us to know the profile of the patients who did not return the completed questionnaire, and also we do not know what effect the fact that the survey period overlapped with the summer period has on the selection of the sample.
In summary, the patients participating in the UC-LIFE survey considered the specialist physician as their main information source, and their responses suggest that knowledge of certain aspects of their disease could be improved. The frequency with which patients go to their specialist physician, even in a situation of clinical stability, and the frequency with which, in case of a flare-up, they can be attended by the specialist, either on the same day in the hospital or by phone, suggests a notable availability of the physicians to their patients. The differences found between hospitals of different sizes, where patients from small hospitals seem to know their disease better but are also seen more frequently and have a better access, should be taken into account for the purpose of a more efficient planning of the care provided to these patients.
Acknowledgements
The UC-LIFE survey was sponsored and funded by Merck Sharp & Dohme de España, a subsidiary of Merck & Co., Inc., Whitehouse Station, New Jersey, USA, and endorsed by the Confederation of Associations for Patients with Crohn's and Ulcerative Colitis of Spain (ACCU). Statistical analysis was performed by Alejandro Pedromingo (Bio-estadistica.com). The authors would like to thank the patients for their invaluable contribution to this study by completing the surveys.
The following healthcare professionals contributed to this study by handing out the survey to their patients (in alphabetical order):
Dr. María M. Alcalde, Hospital Universitario Infanta Cristina, Badajoz.
Dr. Xavier Aldeguer, Hospital Universitario Doctor Josep Trueta, Gerona.
Dr. Federico Argüelles-Arias, Hospital Universitario Virgen Macarena, Sevilla.
Dr. Maite Arroyo, Hospital Universitario Lozano Blesa, Zaragoza.
Dr. Nelly Balza, Hospital Son Llàtzer, Mallorca.
Dr. Jesús Barrio, Hospital Universitario Río Hortega, Valladolid.
Dr. Olga Benítez, Hospital Universitario Mútua de Terrassa, Barcelona.
Dr. Fernando Bermejo, Hospital Universitario de Fuenlabrada, Madrid.
Dr. Xavier Calvet, Corporación Sanitaria Universitaria Parc Taulí, Barcelona.
Dr. Raquel Camargo, Hospital Universitario Virgen de la Victoria, Málaga.
Dr. Daniel Carpio, Complejo Hospitalario Universitario de Pontevedra, Pontevedra.
Dr. María L. Castro, Hospital Universitario Virgen Macarena, Sevilla.
Dr. Daniel Ceballos, Hospital Universitario Doctor Negrín, Gran Canaria.
Dr. Cristóbal de la Coba, Hospital de Cabueñes, Asturias.
Dr. Xavier Cortés, Hospital de Sagunto, Valencia.
Dr. Eugeni Domènech, Hospital Universitario Germans Trias i Pujol, Barcelona.
Dr. Carmen Dueñas, Hospital San Pedro de Alcántara, Cáceres.
Dr. María Fe García, Hospital Universitario de Elche, Alicante.
Dr. Santiago García, Hospital Universitario Miguel Servet, Zaragoza.
Dr. Valle García, Hospital Universitario Reina Sofía, Córdoba.
Dr. Rosario Gómez, Hospital Universitario Virgen de las Nieves, Granada.
Dr. Pedro González, Complejo Hospitalario La Mancha Centro, Ciudad Real.
Dr. Jordi Guardiola, Hospital Universitario de Bellvitge, Barcelona.
Dr. Álvaro Hernández, Hospital de Torrecárdenas, Almería.
Dr. Esteban Hernández, Hospital Universitario del Henares, Madrid.
Dr. José M. Huguet, Consorcio Hospital General Universitario de Valencia, Valencia.
Dr. Antonio López-Sanromán, Hospital Universitario Ramón y Cajal, Madrid.
Dr. Pilar Martínez, Hospital Universitario 12 de Octubre, Madrid.
Dr. Teresa Martínez, Hospital Rafael Méndez, Murcia.
Dr. Ana Muñagorri, Hospital Universitario de Donostia, San Sebastián.
Dr. Concepción Muñoz, Hospital Virgen de la Salud, Toledo.
Dr. José F. Muñoz, Hospital Clínico Universitario de Salamanca, Salamanca.
Dr. Héctor Pallarés, Hospital Juan Ramón Jiménez, Huelva.
Dr. Laura Ramos, Hospital Universitario La Laguna, Tenerife.
Dr. Montserrat Rivero, Hospital Universitario Marqués de Valdecilla, Cantabria.
Dr. Antonio Rodríguez, Hospital Clínico Universitario de Salamanca, Salamanca.
Dr. Cristina Rodríguez, Complejo Hospitalario de Navarra, Navarra.
Dr. Ainhoa Rodríguez-Pescador, Hospital de Galdakao, Vizcaya.
Dr. Patricia Romero, Hospital General Universitario Santa Lucía, Murcia.
References
1. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis Part 1: Definitions and diagnosis. J Crohns Colitis 2012;6:965-90. DOI: 10.1016/j.crohns.2012.09.003. [ Links ]
2. Ghosh S, Shand A, Ferguson A. Ulcerative colitis. Br Med J 2000;320:1119-23. DOI: 10.1136/bmj.320.7242.1119. [ Links ]
3. Johnston RD, Logan RFA. What is the peak age for onset of IBD? Inflamm Bowel Dis 2008;14(Supl 2):S4-5. DOI: 10.1002/ibd.20545. [ Links ]
4. Husain A, Triadafilopoulos G. Communicating with patients with inflammatory bowel disease. Inflamm Bowel Dis 2004;10:444-50. [ Links ]
5. Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: Results of the European Federation of Crohn's and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis 2007;1:10-20. DOI: 10.1016/j.crohns.2007.06.005. [ Links ]
6. Rubin DT, Siegel CA, Kane SV, et al. Impact of ulcerative colitis from patients' and physicians' perspectives: Results from the UC: NORMAL survey. Inflamm Bowel Dis. 2009;15:581-8. DOI: 10.1002/ibd.20793. [ Links ]
7. Casellas F, Arenas JI, Baudet JS, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: A Spanish multicenter study. Inflamm Bowel Dis 2005;11:488-96. DOI: 10.1097/01.MIB.0000159661.55028.56. [ Links ]
8. Iglesias-Rey M, Barreiro-de-Acosta M, Caamaño-Isorna F, et al. Psychological factors are associated with changes in the health-related quality of life in inflammatory bowel disease. Inflamm Bowel Dis 2014;20:92-102. [ Links ]
9. Guthrie E, Jackson J, Shaffer J, et al. Psychological disorder and severity of inflammatory bowel disease predict health-related quality of life in ulcerative colitis and Crohn's disease. Am J Gastroenterol 2002;97:1994-9. DOI: 10.1111/j.1572-0241.2002.05842.x. [ Links ]
10. Suárez-Almazor ME. Patient-physician communication. Curr Opin Rheumatol 2004;16:91-5. DOI: 10.1097/00002281-200403000-00003. [ Links ]
11. Bernstein KI, Promislow S, Carr R, et al. Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis 2011;17:590-8. DOI: 10.1002/ibd.21363. [ Links ]
12. Stewart MA. Effective physician-patient communication and health outcomes: A review. Can Med Assoc J 1995;152(9). [ Links ]
13. Haskard Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: A meta-analysis. Med Care 2009;47(8):826-34. DOI: 10.1097/MLR.0b013e31819a5acc. [ Links ]
14. Bermejo F, López-Sanromán A, Algaba A. Adhesión al tratamiento en la enfermedad inflamatoria intestinal: estrategias para mejorarla. Gastroenterol Hepatol 2009;32(Supl 2):31-6. DOI: 10.1016/j.gastrohep.2009.01.098. [ Links ]
15. Lesnovska KP, Börjeson S, Hjortswang H, et al. What do patients need to know? Living with inflammatory bowel disease. J Clin Nurs 2013;23:1718-25. DOI: 10.1111/jocn.12321. [ Links ]
16. Carpio D, López-Sanromán A, Calvet X, et al. Perception of disease burden and treatment satisfaction in patients with ulcerative colitis from outpatient clinics in Spain: UC-LIFE survey. Eur J Gastroenterol Hepatol 2016;28(9):1056-64. DOI: 10.1097/MEG.0000000000000658. [ Links ]
17. López-Sanromán A, Carpio D, Calvet X, et al. Perceived emotional and psychological impact of ulcerative colitis in outpatients in Spain: UC-LIFE survey. Dig Dis Sci 2016;62(1):207-16. DOI: 10.1007/s10620-016-4363-3. [ Links ]
18. Camacho L. Apoyo y tratamiento psicológico en la enfermedad inflamatoria intestinal: relación médico-paciente. Gastroenterol Hepatol 2009;32(Supl 2):13-8. [ Links ]
19. Dibley L, Bager P, Czuber-Dochan W, et al. Identification of research priorities for inflammatory bowel disease nurses in Europe: a Nurses-European Crohn's and Colitis Organization Delphi Survey. J Crohn's Colitis 2016;11(3):353-9. DOI: 10.1093/ecco-jcc/jjw164. [ Links ]
20. Robinson A, Thompson D.G, Wilkin D, et al. Guided self-management and patient-directed follow-up of ulcerative colitis: A randomized trial. Lancet 2001;358:976-81. DOI: 10.1016/S0140-6736(01)06105-0. [ Links ]
21. Kennedy AP, Nelson E, Reeves D, et al. A randomized controlled trial to assess the effectiveness and cost of a patient orientated self-management approach to chronic inflammatory bowel disease. Gut 2004;53:1639-45. DOI: 10.1136/gut.2003.034256. [ Links ]
22. Casellas F, Fontanet G, Borruel N, et al. The opinion of patients with inflammatory bowel disease on healthcare received. Rev Esp Enferm Dig 2004;96:174-84. DOI: 10.4321/S1130-01082004000300003. [ Links ]
23. Han SW, McColl E, Steen N, et al. The predictors of hospital clinic visits in patients with ulcerative colitis: an examination of disease variables, quality of life and illness perception. Gastroenterol 2000;118(Issue 4)1:A123. DOI: 10.1016/S0016-5085(00)82572-X. [ Links ]
24. Drossman DA, Leserman J, Mitchell CM, et al. Health status and health care use in persons with inflammatory bowel disease. A national sample. Dig Dis Sci 1991;36(12):1746-55. [ Links ]
25. De Boer A, Sprangers M, Bartelsman J, et al. Predictors of health care utilization in patients with inflammatory bowel disease: A longitudinal study. Eur J Gastroenterol Hepatol 1998;10:783-9. DOI: 10.1097/00042737-199809000-00010. [ Links ]
26. Marín-Jiménez I, Nos P, Domenèch E, et al. Diagnostic performance of the simple clinical colitis activity index self-administered online at home by patients with ulcerative colitis: CRONICA-UC study. Am J Gastroenterol 2016;111:261-8. DOI: 10.1038/ajg.2015.403. [ Links ]
![]() Correspondence:
Correspondence:
Cristina Romero de Santos.
Medical Department.
Merck Sharp & Dohme de España.
C/ Josefa Valcarcel, 38.
28027 Madrid, Spain
e-mail: cristina.rdesantos@merck.com
Received: 21-12-2016
Accepted: 25-01-2017











 texto en
texto en