Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.9 Madrid sep. 2017
https://dx.doi.org/10.17235/reed.2017.4660/2016
New psychological therapies for irritable bowel syndrome: mindfulness, acceptance and commitment therapy (ACT)
Beatriz Sebastián Sánchez1, Jesús Gil Roales-Nieto2, Nuno B. Ferreira3, Bárbara Gil Luciano4 and Juan José Sebastián Domingo5
1Department of Psycology. Universidad de Almería. Almería, Spain.
2Department of Health Psychology. Universidad de Almería. Almería, Spain.
3Department of Clinical and Health Psychology. University of Edinburgh. Edinburgh, United Kingdom.
4Department of sycology. Universidad de Almería. Almería, Spain; Madrid Institute of Contextual Psychology. Madrid, Spain.
5Functional Gastrointestinal Disorders Consultation. Gastroenterology Unit. Hospital General Royo Villanova. Zaragoza, Spain
ABSTRACT
The current goal of treatment in irritable bowel syndrome (IBS) focuses primarily on symptom management and attempts to improve quality of life. Several treatments are at the disposal of physicians; lifestyle and dietary management, pharmacological treatments and psychological interventions are the most used and recommended. Psychological treatments have been proposed as viable alternatives or compliments to existing care models. Most forms of psychological therapies studied have been shown to be helpful in reducing symptoms and in improving the psychological component of anxiety/depression and health-related quality of life. According to current NICE/NHS guidelines, physicians should consider referral for psychological treatment in patients who do not respond to pharmacotherapy for a period of 12 months and develop a continuing symptom profile (described as refractory irritable bowel syndrome). Cognitive behavioral therapy (CBT) is the best studied treatment and seems to be the most promising therapeutic approach. However, some studies have challenged the effectiveness of this therapy for irritable bowel syndrome. One study concluded that cognitive behavioral therapy is no more effective than attention placebo control condition and another study showed that the beneficial effects wane after six months of follow-up. A review of mind/body approaches to irritable bowel syndrome has therefore suggested that alternate strategies targeting mechanisms other than thought content change might be helpful, specifically mindfulness and acceptance-based approaches. In this article we review these new psychological treatment approaches in an attempt to raise awareness of alternative treatments to gastroenterologists that treat this clinical syndrome.
Key words: Irritable bowel syndrome. Mental disorders. Psychotherapy. Cognitive therapy. Mindfulness. Acceptance and commitment therapy.
Introduction
A recent systematic review and meta-analysis has demonstrated a global prevalence of IBS of 11%, a percentage that varies considerably in some instances according to the geographic region and diagnostic criteria used to define the syndrome (1). On the other hand, the percentage of patients seeking health care related to IBS reaches 12% in Primary Care practices and is by far the largest subgroup seen in gastroenterology clinics (2).
IBS has been defined according to the new Rome IV criteria (3) as recurrent abdominal pain associated with two or more of the following conditions: related to defecation, associated with a change in the frequency of stool and associated with a change in the consistency of stool. Symptom onset should occur at least six months before the diagnosis and symptoms should be present on average at least one day a week in the last three months.
The etiology and pathophysiology of IBS is unknown. Several pathogenic factors responsible for IBS have been proposed, such as genetic and environmental factors (4), abnormal gut motility (5), visceral hypersensitivity (6), post-infectious inflammatory mechanisms (7), psychological morbidity, physical, emotional and sexual abuse (8), bacterial overgrowth (9) and changes in intestinal microbiota (10), among others. However, none of them seem to clearly explain the mechanisms that trigger the syndrome.
Nowadays, a model taking into account the numerous physiological symptoms (e.g., altered motility, gut hypersensitivity) but also psychosocial factors and interactions between the brain and gut seems to be shifting the understanding of IBS (11).
This biopsychosocial interpretation of IBS (11), heavily influenced by discoveries in the fields of psychosomatics and psychoneuroimmunology (12,13), is now recognized as one of the most complete and best fitting models for this illness.
In the model we can see how changes in early life/premorbid genetic and environmental (parenting, infection) factors might play a role in the development of both psychosocial (susceptibility to stress, psychological illness, psychological traits) and physiological (abnormal motility, visceral hypersensitivity) factors leading to the expression of IBS symptoms and coping behaviors. Also, the interplay between psychosocial and physiological factors via the interactions between the central nervous system (CNS) and the enteric nervous system (ENS) is thought to influence IBS expression (11). These biopsychosocial interactions are therefore thought to have an impact on patient quality of life and their approach to health care.
Historically, the absence of a structural or organic explanation for IBS and anecdotal observations of patient behavior has always seemed to support the possible presence of psychological morbidity.
Early research concluded that the etiology of IBS was linked to hypochondriasis or psychogenic traits (14), with some authors even considering IBS to be part of a psychiatric illness (15). This is not surprising as most studies show that between 54% and 94% of IBS patients meet criteria for at least one (axis I) psychiatric disorder (16). IBS patients usually have associated mental disorders with the most frequent being anxiety (69%) followed by affective disorders (38%) (17); other common symptoms include nervousness, rumination, panic attacks, posttraumatic stress, social phobia, somatization and eating disorders. Less common symptoms include sleep disorders, loss of appetite and exhaustion (18-20).
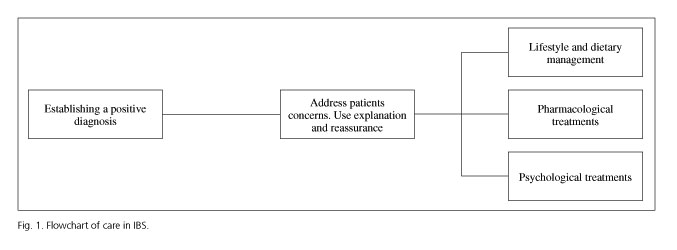
This is particularly relevant given the current guidelines for interventions in IBS. The current goal of treatment in IBS focuses primarily on symptom management and attempts to improve quality of life (21). Therefore, after a positive diagnosis several treatments are at the disposal of physicians, with lifestyle and dietary management, pharmacological treatments and psychological interventions as the most used and recommended (21,22). The practice guidelines for the management of IBS-constipation (23) is a useful resource that has been recently published in this journal.
Figure 1 shows an adapted flow chart of care resulting from a consensus between the recommendations of the British Society of Gastroenterology (22), the National Institute for Health and Clinical Excellence (NICE) (24) and the American College of Gastroenterology (25).
Although lifestyle and dietary management (e.g., exercise, fiber intake) have limited efficacy in IBS, generally speaking their safety and general health net benefits seem to justify their inclusion as a first line of management (22). With regard to conventional medical treatment (i.e., pharmacological), several studies and reviews have highlighted the limited efficacy of these approaches in providing adequate relief for IBS patients. Nevertheless, some drugs that are being used recently, such as linaclotide, rifaximine, melatonine or antidepressants, are showing good results (26). Therefore, other approaches such as psychological treatments have been proposed as viable alternatives or compliments to existing models of care (27).
Most forms of psychological therapies studied have been shown to be helpful in reducing symptoms and in improving psychological components of anxiety/depression and health-related quality of life (22,27,28). The success of psychological therapies for IBS global outcomes means that it is being implemented as a standard adjunctive treatment in the United Kingdom. According to current NICE/NHS (24) guidelines, physicians should consider referral for psychological treatment in patients who do not respond to pharmacotherapy for a period of 12 months and develop a continuing symptom profile (described as refractory IBS). Therefore, those patients who do not improve with first line treatments can benefit from psychological interventions, which may reduce pain and other symptoms and also improve quality of life.
The most studied and used forms of psychological treatment for IBS are relaxation training, brief psychodynamic psychotherapy, CBT, hypnotherapy and several forms of self-help. These forms of treatment have been used both in individual and group settings and are thought to be acceptable for patients, especially those who identify psychological factors as triggers for their IBS (29). Table 1 provides a simple overview of the most important psychological therapies in terms of understanding the (psycho)pathology, objectives of therapy, the techniques used and their strengths/weaknesses in an attempt to facilitate their comprehension beyond the psychological field.
So far, CBT is the best studied and has been proposed as the most promising treatment (26,30). However, some studies have challenged the effectiveness of CBT for IBS. In particular, one study concluded that CBT is no more effective than a attention placebo control condition (31) and another demonstrated that the effects seem to wane after six months of follow-up (32). In addition, studies exploring active components of CBT found that cognitive change (one of the key components of CBT) was not associated with any significant changes in outcome (33). A review of mind/body approaches to IBS has therefore suggested that strategies that target mechanisms other than thought content change might be helpful, specifically mindfulness and acceptance-based approaches (29).
In this article, we will review these new psychological treatment approaches in an attempt to raise awareness of these alternative treatments to gastroenterologists that treat this clinical syndrome.
Bibliographic search strategy
The biomedical literature search was performed in the PubMed database of the United States National Library of Medicine (pubmed.gov). The MeSH (Medical Subjects Headings) terms used to conduct the review and search of scientific evidence were: Irritable Bowel Syndrome [in the title] combined with Mindfulness [in the title] and also with Acceptance and Commitment Therapy or Acceptance-Commitment, respectively using the Boolean operator AND/OR. The results obtained were filtered with the following limits: types of studies: Systematic Reviews, Meta-Analysis, Guideline, Practice Guideline, Consensus Development Conference (and Consensus Development Conference NIH), Randomized Controlled Trial, Controlled Clinical Trial and Clinical Trial; age: adults (19 or more years); language: English and/or Spanish; also the abstract was available for all articles.
The database was searched for relevant studies published up until July 2016.
Initially, the title, abstract and keywords were screened of every record identified with the search strategy. All potentially relevant articles were retained and the full text of these studies obtained and evaluated in detail. Irrelevant articles were excluded on the basis of the title or abstract. Foreign language papers were translated when necessary.
One author (BS) performed the data extraction, which was then assessed by another author (NBF). The differences between reviewers were resolved by discussion until a consensus was reached.
The psychology of IBS
The psychosocial profile of the IBS patient
Although physical symptoms are at the forefront of IBS patient presentation, several studies have shown that a key factor in the maintenance and aggravation of IBS relates to psychosocial factors (cognitive and emotional) (34). Most patients are likely to report experiences such as worrying about their symptoms, consequences and duration, anxiety, depression, stress, shame and anger (35,36). Within these psychosocial phenomena, the most commonly reported is gastrointestinal specific anxiety (GSA). This is defined as "the cognitive, affective and behavioral response stemming from fear of gastrointestinal sensations, symptoms and the context in which these visceral sensations and symptoms occur" (37). GSA is thought to contribute to IBS maintenance by acting as an endogenous stressor that perpetuates alterations in autonomic and neuroendocrine responses even in the absence of an external stressor (38). The literature has shown that higher levels of GSA are related to higher symptom severity and lower quality of life in IBS (37,39,40).
Linked to GSA is the behavior displayed by IBS patients, with avoidance being the main strategy used to cope with the aversive experiences of the illness, even in the absence of symptoms (41). Patients tend to avoid situations or events such as certain foods or food-related situations (e.g., eating out), social or work related situations (e.g., gatherings or meetings), leisure or travelling, personal relationships and intimate contact (42). Even though most patients believe that this type of response is essential for the management of their condition, they also recognize this to be the main cause of their suffering (43).
The literature seems to support this with several studies showing that avoidant coping mechanisms are associated with poorer quality of life, high levels of anxiety and depression (44,45). Furthermore, it has been shown that recurrent avoidance as a coping strategy is only effective in the short term and has a rebound effect in the long term (for example, the more one tries to eliminate a thought, the more frequent it becomes) (46-48).
Strategies such as distraction are not useful and can increase pain awareness (49). Therefore, it has been suggested that the content or nature of the distressing experiences (physical or psychological) does not cause the suffering in IBS, but rather how patients relate to these experiences and try to deal with them.
The alternative seems to be discriminating, observing and accepting private experiences without trying to alter their form but altering the function of the behavior (50,51). From this perspective, the goal of psychological intervention is to help the patient develop and enhance skills that allow him/her to view and accept the private events related to his/her illness (thoughts and feelings of shame or guilt, fear, anxiety, stress, specific symptoms, etc.) without changing them and therefore directing and maintaining behavior toward his/her values and life goals.
Contextual behavioral models and IBS
As previously noted, some authors (29) have recommended that psychological treatments of IBS should not focus on changing the form and frequency of the symptoms or experiences related to IBS, but to change how patients deal with these experiences instead.
Treatment models developed from a contextual behavioral (or third wave) perspective seem to address this issue. New psychological treatments have arisen as a result of significant shifts in the philosophy of science (from mechanism to functional contextualism) (52) and advances in the study of language and cognition as forms of behavior (relational frame theory) (53).
As a whole, these treatment models aim to: a) build broad, flexible and effective behavioral repertoires in the patient that are in line with their personal values; b) modifying the way the patient relates to their experiences (symptoms, thoughts, emotions and sensations), so instead of focusing on eliminating them (53,54) the patient can effect valued behavior in their presence; and c) instil moment-by-moment awareness so that the patient can sense the context and function of their experiences whilst not becoming entangled in them to the point that they dictate their behavior.
Third-wave approaches include a wide number of therapeutic models such as dialectical behavior therapy (DBT) (55), mindfulness-based cognitive therapy (MBCT) (56), behavioral activation (BA) (57), as well as functional analytic psychotherapy (FAP) (58).
For the purposes of this article, we will be using ACT as a frame of reference as it provides the most comprehensive account of how these interventions can be useful for IBS whilst also having the most robust evidence base (59).
ACT brings a new conceptualization of the suffering of patients with IBS in the following way: "A proportion of IBS patients can be functionally characterized by the use of behaviors that seek to control, eliminate or alter the physical, emotional and cognitive experiences associated with IBS both in the presence or absence of symptoms. These behaviors seem to be motivated by an excessive fusion with a self-conceptualization of being an IBS patient, fusion with unhelpful illness specific beliefs or cognitions and by a dominance of feared future consequences or comparison with an idealized past. IBS patients also tend to choose to engage in these avoidant behaviors that provide short-term relief from their experiences over engaging in behaviors that are values-consistent and that might lead to better life satisfaction on the long-term." (60).
These are simultaneously occurring processes that contribute to this process known as psychological inflexibility (PI), narrowing the patient's repertoire and taking them to inaction, persistent avoidance and to an increasing limitation of life (61).
Acceptance and commitment therapy (pronounced as one word, "ACT") (62) is a new behavioral therapeutic approach that uses processes of acceptance, defusion (see below), commitment and behavior change to increase psychological flexibility, defined as "the ability to contact the present moment more fully as a conscious human being and to either change or persist in behaviors when doing so serves valued ends" (63).
The use of defusion in ACT could be behaviorally described as a way to train discrimination between private events and the individual self, i.e., the individual is able to observe events such as thoughts, emotions, memories or physical sensations as part of a repertoire of experiences that a human being is likely to experience, without becoming entangled in these experiences to a point that it exerts undue influence on their behavior (64). In order to contact this type of discrimination on a moment-by-moment basis, ACT attempts to reinforce a sense of being in the present in patients via mindfulness practices. In this defused stance, the patient is then more likely (or accepting) to hold distressing experiences if it then allows him/her to move and behave coherently towards a valued end (e.g., family, friendships).
Some mindfulness practices are described and used in more depth in other third-wave therapies such as the mindfulness-based stress reduction (MBSR) program (65), one of the first procedures to integrate Eastern practices such as meditation and yoga into the management of chronic pain and illness. Similarly, MBCT includes formal meditation and promotes a decentered view of thoughts, emotions and body sensations (66).
The importance of looking at the function of MBSR and MBCT procedures should be noted. Although these techniques are aimed to train the person to become more aware of the symptoms and not behave according to them (that is, to change the function of the symptoms), they can be easily interpreted or used as a way to reduce or change the symptoms (and thus behave accordingly to them).
This model has received a lot of support and has proved to be very effective in health conditions (59) such as diabetes (67), epilepsy (68), tinnitus (69) and chronic pain (70-72), and its application to IBS is under consideration (73,74).
Evidence of the application of third generation therapies to IBS
Some encouraging results have been found with regard to the application of third-wave psychological therapies in IBS.
The following is a narrative review of studies on the application of mindfulness techniques with CBT components, the application of mindfulness techniques alone and finally, the application of ACT.
Mindfulness combined with CBT
One study (75) applied a CBT-based protocol combining mindfulness techniques and exposure aimed at reducing GSA. The inclusion criteria were female gender and age between 18 and 65 years. Patients were excluded if any somatic or psychiatric disorder deemed to interfere with the treatment was present. A mindfulness component allows patients to be less likely to act on impulses, which, together with the exposure component (provocation of symptoms, prevention of response and exposure to situations that evoke symptoms), helps the patient to accept his/her symptoms and aversive thoughts. This protocol led to a significant improvement in all symptoms (except for diarrhea) and quality of life. The same effects were observed in an internet-based version of the same protocol and were maintained for up to six months (76,77).
Mindfulness alone
The first non-controlled trial (78) was conducted in a veteran population with the following exclusion criteria: a) psychotic disorder; b) mania or bipolar disorder; c) personality disorders; d) suicidal or homicidal ideation; and e) active substance abuse or dependence. The results showed that participation in an MBSR group was associated with improvements in IBS-related quality of life and GSA. Changes in mindfulness skills were correlated with improvements in GSA in those meeting the Rome IBS criteria, and there was a significant decrease in the percentage of subjects meeting Rome IBS criteria during the 6-month follow-up.
A randomized controlled clinical trial of the application of mindfulness to IBS (79) was conducted in a female only population who had a medical diagnosis of IBS and who also met the Rome II criteria for IBS. Exclusion criteria included: a) diagnosis of mental illness with psychotic features; b) a history of an inpatient admission for a psychiatric disorder within the past two years; c) a history or current symptoms of inflammatory bowel disease or gastrointestinal malignancy; d) active liver or pancreatic disease; e) uncontrolled lactose intolerance; f) celiac disease; g) a history of abdominal trauma or surgery involving gastrointestinal resection; or h) pregnancy or intention to become pregnant during the study. This protocol involved an 8-week mindfulness training that included techniques such as body scan, meditation, yoga and exercises that help the patient to learn to observe thoughts and body sensations in a non-judgmental manner. This protocol had a clinically significant therapeutic effect on the severity of bowel symptoms (26.4% reduction compared to 6.2% in the control group), and improved the quality of life related to health, even at three months of follow-up. In addition, the protocol also had an effect on psychological symptoms (anxiety, general severity, visceral anxiety) that was thought to have been mediated by an increase in mindfulness (79). The authors suggest that the program allows the patient to learn specific techniques with lasting effects which can be performed in groups and are more cost-effective than other treatments such as CBT or hypnosis.
A second controlled study (80) was conducted with the following exclusion criteria: a) diagnosis of a DSM-IV axis I mood, anxiety, or psychotic disorder; b) current use of antipsychotics; or c) previous participation in an MBSR group. In order to ensure the stability of medication during the course of the study, if there had been a change in medication, patients were asked to wait three months before being enrolled in the next cohort for randomization and not to change regimens or dosages for the duration of the study. Results showed a greater improvement of symptoms (from moderate to severe) in patients in a MBSR group in comparison to a control group. However, a rebound effect of symptoms during follow-up was observed, i.e., the rate of improvement due to the program was not found to be maintained over time. In addition, the control group also improved over time, perhaps due to the beneficial effects of attention, self-monitoring and the anticipation of participating in the MBSR group, and no differences were observed between the groups in terms of quality of life, alterations of mood and spirituality.
Finally, a recent study (81) comparing mindfulness-based treatments (MBT) with CBT has shown that the former is more effective in reducing IBS symptoms and has a longer lasting effect.
ACT
The application of ACT in IBS is still in an early stage, although significant steps have recently been made for its implementation. For example, a pilot study (82) that analyzed the effectiveness of ACT in adolescents with functional abdominal pain (some with IBS) showed that 12 to 14 sessions were effective in improving quality of life, levels of depression, anxiety and somatic complaints during the first month of follow-up. Methodological shortcomings limit the conclusions of the study, although this preliminary evidence suggests that ACT could be an effective approach to IBS.
The first study (74) to investigate the application of ACT in IBS was conducted with the following specific exclusion criteria: a) pregnant or breastfeeding women; b) any symptoms suggestive of significant inflammatory or neoplastic gastrointestinal disorder (such as unexplained weight loss or unexplained rectal bleeding); and c) a known cognitive impairment. The protocol included a one-day group workshop combined with working with a self-help workbook for a period of two months (83). The limitations of this study were a highly selected population, a very specific format of intervention, and the absence of a formal control group condition (this was compensated by using a within subject design). However, the results showed that ACT was effective at reducing symptoms, GSA and the use of IBS-related avoidance behaviors, and improved IBS-related and general quality of life. These results were maintained at the 6-month follow-up with a trend for further gains (albeit non-statistically significant).
Part of this study also involved the development of a measure of psychological flexibility specific to IBS, the Irritable Bowel Syndrome Acceptance and Action Questionnaire (IBSAAQ) (84). The development of this scale allowed the authors to explore the role of psychological flexibility in the biopsychosocial model of IBS. The results indicated that psychological flexibility was a significant predictor of all IBS-related outcomes beyond the effects of symptom severity or cognitive variables. In addition, the authors also explored the putative mechanism through which an ACT intervention works, i.e., that improvement in outcomes occurs via an increase in psychological flexibility. The authors reported that all gains in IBS related outcomes following the ACT intervention were fully mediated by increases in psychological flexibility thus favoring the validity of the intervention model.
Final considerations
The research conducted to date on the implementation of third-generation therapies for IBS has shown promising results. Two recent reviews have shown that (85,86) MBT, when combined with CBT, appears to be effective in reducing symptoms and improving quality of life in IBS. Furthermore, improvement in symptoms seems to occur even when accounting for the different IBS presentation types (e.g., constipation or predominant diarrhea). However, both reviews indicated that the results should be interpreted with caution as most of the studies were of poor quality and had many methodological limitations (small and heterogeneous samples, dropouts, risk of bias, etc.).
On the other hand, the ACT approach, which incorporates a more comprehensive model that is based on a growth agenda (getting patients to enact their valued behaviors) rather than trying to address a deficit agenda (changing symptoms or thoughts), seems to be more effective.
Indeed, those patients who have trouble managing their bowel disorder and meet criteria for psychological comorbidity might be the most suitable candidates for this kind of psychological therapy. Especially when the condition interferes with daily life and progressively results in a restricted life. For example, if a patient avoids different situations (e.g., personal relationships and intimate contact, work related situations, leisure or travelling) this might be a good indication. Nevertheless, a patient's functional analysis of behavior might be an effective general recommendation in order to explore if a pattern of PI is occurring. Over time, a pattern of PI may alter a person's behavior resulting in more severe symptoms (both physical and psychological) and a lower quality of life. The core therapeutic strategy of ACT could aid in changing the PI pattern and the patient can start to build a more flexible and effective way of living with the illness.
Although ACT could be conceived primarily as a form of individual therapy, it is extremely flexible and can be adapted to a group format and can also be used in a telephone (87) or Internet (75) format. This allows the adjustment to economic resources and available time within hospitals, medical specialty centers and health centers. In addition, training in this therapeutic approach is not as intensive as in other intervention procedures (CBT, for example) and can be rolled out to different professionals (not just psychologists) (88).
Empirical evidence of ACT for IBS, albeit preliminary, shows that the results are maintained in the long-term (up to six-months of follow-up) and that improvements occur through the hypothesized path of an increase in psychological flexibility. These results are very encouraging and invite different professionals to continue working in this direction.
These findings add to the extensive literature that has shown the usefulness of ACT in improving different medical conditions, by either promoting healthy behavior (diabetes control, smoking cessation and weight maintenance) or by changing the attitude that patients have with their difficult experiences of the illness (chronic pain), resulting in significant improvements in quality of life (74).
Interesting pioneering work with patients with chronic pain (64) have shown the benefits of the joint work of different professionals (physiotherapists, occupational therapists, nurses, doctors and psychologists) in the patient's experience of the illness and the related quality of life.
Similarly, patients with other illnesses such as IBS (and other functional gastrointestinal disorders) may benefit from the interaction between gastroenterologists, nutritionists/dieticians, nurses and psychologists. Even though the purpose of pharmacological treatment is to affect the pathophysiological mechanism or the symptoms, initially it is not incompatible with psychological therapy, and IBS patients could actually benefit from the combination of both approaches. However, the idea is that all professionals work together in unison to teach patients how to behave effectively when faced with symptoms, feelings of shame or anxiety, and, instead of trying to control them, learn to integrate them as part of their life. Thus, from a contextual perspective, and with the supporting empirical evidence, the goal will be to focus on training the person to observe and react to symptoms (stress, for example) in a way that is consistent to his/her objectives, goals and values. After all, although IBS patients have an illness, they also have a life worth living, even if they have to carry the burden of the illness.
In summary, although ACT was originally designed for psychological disorders, it has recently been applied to medical conditions with very promising results. The present review is the first compilation of the new evidence from a psychological perspective for non-psychologists (in this case, for gastroenterologists). Despite the limitations of the initial attempts (few studies with few and highly selected populations and other methodological shortcomings), this new direction is very promising and more research is needed so that we can address this syndrome in a more precise and efficient way. ACT is not difficult to apply (brief protocols can be used and better results are obtained if different professionals work together as a team), nor to evaluate (there are general measures of PI as well as specific measures for IBS). Thus, we hope this review sheds light on this treatment option and that more practitioners start to implement these therapies in order to help patients with IBS to live their life in a better way and accept their illness as a part of it.
References
1. Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin Gastroenterol Hepatol 2012;10(7):712-21. DOI: 10.1016/j.cgh.2012.02.029. [ Links ]
2. Saha L. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine World J Gastroenterol 2014;20(22):6759-73. [ Links ]
3. Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterol 2016;150:1393-1407. DOI: 10.1053/j.gastro.2016.02.031. [ Links ]
4. Makker J, Chilimuri S, Bella JN. Genetic epidemiology of irritable bowel syndrome. World J Gastroenterol 2015;21(40):11353-61. DOI: 10.3748/wjg.v21.i40.11353. [ Links ]
5. DuPont AW, Jiang ZD, Harold SA, et al. Motility abnormalities in irritable bowel syndrome. Digestion 2014;89(2):119-23. DOI: 10.1159/000356314. [ Links ]
6. Farzaei MH, Bahramsoltani R, Abdollahi M, et al. The role of visceral hypersensitivity in irritable bowel syndrome: Pharmacological targets and novel treatments. J Neurogastroenterol Motil 2016;22(4):558-74. DOI: 10.5056/jnm16001. [ Links ]
7. Bealty JK, Bhargava A, Buret AG. Post-infectious irritable bowel syndrome: mechanistic insights into chronic disturbances following enteric infection. World J Gastroenterol 2014;20(14):3976-85. DOI: 10.3748/wjg.v20.i14.3976. [ Links ]
8. Surdea-Blaga T, B ban A, Dumitrascu DL. Psychosocial determinants of irritable bowel syndrome. World J Gastroenterol 2012;18(7):616-26. DOI: 10.3748/wjg.v18.i7.616. [ Links ]
9. Mooney PD, Hayman J, Pickering G, et al. Are we underestimating the prevalence of small intestinal bacterial overgrowth in irritable bowel syndrome? Neurogastroenterol Motil 2015;27(8):1190-1. [ Links ]
10. Dupont HL. Review article: Evidence for the role of gut microbiota in irritable bowel syndrome and its potential influence on therapeutic targets. Aliment Pharmacol Ther 2014;39(10):1033-42. DOI: 10.1111/apt.12728. [ Links ]
11. Van Oudenhove L, Crowell MD, Drossman DA, et al. Biopsychosocial aspects of functional gastrointestinal disorders. Gastroenterol 2016;pii:S0016-5085(16)00218-3. DOI: 10.1053/j.gastro.2016.02.027. [ Links ]
12. Arebi N, Gurmany S, Bullas D, et al. Review article: The psychoneuroimmunology of irritable bowel syndrome - An exploration of interactions between psychological, neurological and immunological observations. Aliment Pharmacol Ther 2008;28(7):830-40. DOI: 10.1111/j.1365-2036.2008.03801.x. [ Links ]
13. Sebastián Domingo JJ, Sebastián Sánchez B. Psychoneuroimmunology in irritable bowel syndrome. Gastroenterol Hepatol 2015;38(7):413-6. [ Links ]
14. Hislop, IG. Psychological significance of the irritable colon syndrome. Gut 1971;12(6):452-7. DOI: 10.1136/gut.12.6.452. [ Links ]
15. Liss JL, Alpers D, Woodruff RA Jr. The irritable colon syndrome and psychiatric illness. Dis Nerv Syst 1973;34(4):151-7. [ Links ]
16. Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: What are the causes and implications? Gastroenterol 2002;122(4):1140-56. DOI: 10.1053/gast.2002.32392. [ Links ]
17. Lackner JM, Ma CX, Keefer L, et al. Type, rather than number, of mental and physical comorbidities increases the severity of symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2013;11(9):1147-57. DOI: 10.1016/j.cgh.2013.03.011. [ Links ]
18. Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: Relations with functional, mental, and somatoform disorders. World J Gastroenterol 2014;20(20):6024-30. DOI: 10.3748/wjg.v20.i20.6024. [ Links ]
19. Tosic-Golubovic S, Miljkovic S, Nagorni A, et al. Irritable bowel syndrome, anxiety, depression and personality characteristics. Psychiatr Danub 2010;22(3):418-24. [ Links ]
20. Lydiard RB, Falsetti SA. Experience with anxiety and depression treatment studies: Implications for designing IBS clinical trials. Am J Med 1999;107(5A):65S-73S DOI: 10.1016/S0002-9343(99)00082-0. [ Links ]
21. Grundmann O, Yoon SL. Irritable bowel syndrome: Epidemiology, diagnosis and treatment - An update for health-care practitioners. J Gastroenterol Hepatol 2010;25(4):691-9. DOI: 10.1111/j.1440-1746.2009.06120.x. [ Links ]
22. Spiller R, Aziz Q, Creed F, et al. Guidelines on the irritable bowel syndrome: Mechanisms and practical management. Gut 2007;56(12):1770-98. DOI: 10.1136/gut.2007.119446. [ Links ]
23. Mearin F, Ciriza C, Mínguez M, et al. Clinical Practice Guideline: Irritable bowel syndrome with constipation and functional constipation in the adult. Rev Esp Enferm Dig 2016;108(6):332-63. DOI: 10.17235/reed.2016.4389/2016. [ Links ]
24. Hookway C, Buckner S, Crosland P, et al. Irritable bowel syndrome in adults in Primary Care: Summary of updated NICE guidance. BMJ 2015;350:h701. DOI: 10.1136/bmj.h701. [ Links ]
25. Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109(Suppl 1):S2-26. DOI: 10.1038/ajg.2014.187. [ Links ]
26. Sebastián Domingo JJ. Irritable bowel syndrome: The next-to-last that is being investigated. Med Clin (Barc) 2016;146(6):260-2. DOI: 10.1016/j.medcli.2015.10.010. [ Links ]
27. Zijdenbos IL, De Wit NJ, Van der Heijden GJ, et al. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database Syst Rev 2009;(1):CD006442. [ Links ]
28. Ford AC, Quigley EM, Lacy BE, et al. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: Systematic review and meta-analysis. Am J Gastroenterol 2014;109(9):1350-65. DOI: 10.1038/ajg.2014.148. [ Links ]
29. Naliboff BD, Fresé MP, Rapgay L. Mind/body psychological treatments for irritable bowel syndrome. Evid Based Complement Alternat Med 2008;5(1):41-50. DOI: 10.1093/ecam/nem046. [ Links ]
30. Toner BB. Cognitive-behavioral treatment of irritable bowel syndrome. CNS Spectr 2005;10(11):883-90. DOI: 10.1017/S1092852900019854. [ Links ]
31. Blanchard EB, Lackner JM, Sanders K, et al. A controlled evaluation of group cognitive therapy in the treatment of irritable bowel syndrome. Behav Res Ther 2007;45(4):633-48. DOI: 10.1016/j.brat.2006.07.003. [ Links ]
32. Kennedy TM, Chalder T, McCrone P, et al. Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in Primary Care: Randomised controlled trial. Health Technol Assess 2006;10(19):iii-iv,ix-x,1-67. DOI: 10.3310/hta10190. [ Links ]
33. Lackner JM, Jaccard J, Krasner SS, et al. How does cognitive behavior therapy for irritable bowel syndrome work? A mediational analysis of a randomized clinical trial. Gastroenterol 2007;133(2):433-44. DOI: 10.1053/j.gastro.2007.05.014. [ Links ]
34. Levy RL, Olden KW, Naliboff BD, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterol 2006;130(5):1447-58. DOI: 10.1053/j.gastro.2005.11.057. [ Links ]
35. Schneider MA, Fletcher PC. "I feel as if my IBS is keeping me hostage!" Exploring the negative impact of irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) upon university-aged women. Int J Nurs Pract 2008;14(2):135-48. DOI: 10.1111/j.1440-172X.2008.00677.x. [ Links ]
36. Toner BB, Stuckless N, Ali A, et al. The development of a cognitive scale for functional bowel disorders. Psychosom Med 1998;60(4):492-7. DOI: 10.1097/00006842-199807000-00017. [ Links ]
37. Labus JS, Mayer EA, Chang L, et al. The central role of gastrointestinal-specific anxiety in irritable bowel syndrome: Further validation of the visceral sensitivity index. Psychosom Med 2007;69(1):89-98. DOI: 10.1097/PSY.0b013e31802e2f24. [ Links ]
38. Mayer EA, Naliboff BD, Chang L, et al. V. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol 2001;280(4):G519-24. [ Links ]
39. Jerndal P, Ringström G, Agerforz P, et al. Gastrointestinal-specific anxiety: An important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterol Motil 2010;22(6):646-e179. DOI: 10.1111/j.1365-2982.2010.01493.x. [ Links ]
40. Labus JS, Bolus R, Chang L, et al. The Visceral Sensitivity Index: Development and validation of a gastrointestinal symptom-specific anxiety scale. Aliment Pharmacol Ther 2004;20(1):89-97. DOI: 10.1111/j.1365-2036.2004.02007.x. [ Links ]
41. Corney RH, Stanton R. Physical symptom severity, psychological and social dysfunction in a series of outpatients with irritable bowel syndrome. J Psychosom Res 1990;34(5):483-91. DOI: 10.1016/0022-3999(90)90022-V. [ Links ]
42. Rønnevig M, Vandvik PO, Bergbom I. Patients' experiences of living with irritable bowel syndrome. J Adv Nurs 2009;65(8):1676-85. DOI: 10.1111/j.1365-2648.2009.05030.x. [ Links ]
43. Drossman DA, Chang L, Schneck S, et al. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig Dis Sci 2009;54(7):1532-41. DOI: 10.1007/s10620-009-0792-6. [ Links ]
44. Rutter CL, Rutter DR. Illness representation, coping and outcome in irritable bowel syndrome (IBS). Br J Health Psychol 2002;7(Part 4):377-91. DOI: 10.1348/135910702320645372. [ Links ]
45. Rutter CL, Rutter DR. Longitudinal analysis of the illness representation model in patients with irritable bowel syndrome (IBS). J Health Psychol 2007;12(1):141-8. DOI: 10.1177/1359105307071748. [ Links ]
46. Törneke N, Luciano MC, Valdivia-Salas S. Rule-governed behavior and psychological problems. Int J Psych Psychol Ther 2008;8(2):141-56. [ Links ]
47. Chawla N, Ostafin B. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. J Clin Psychol 2007;63(9):871-90. DOI: 10.1002/jclp.20400. [ Links ]
48. Törneke N, Luciano C, Barnes-Holmes Y, et al. RFT for clinical practice: Three core strategies in understanding and treating human suffering. Wiley Handbook Context Behav Sci 2016:254-73. [ Links ]
49. McCracken LM. "Attention" to pain in persons with chronic pain: A behavioral approach. Behav Ther 1997;28(2):271-84. DOI: 10.1016/S0005-7894(97)80047-0. [ Links ]
50. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [ Links ]
51. Luciano MC, Wilson KG. Terapia de aceptación y compromiso. Un tratamiento conductual orientado a los valores. Madrid: Editorial Pirámide; 2002. [ Links ]
52. Biglan A, Hayes SC. Should the behavioral sciences become more pragmatic? The case for functional contextualism in research on human behavior. Appl Prev Psychol 1997;5(1):47-57. DOI: 10.1016/S0962-1849(96)80026-6. [ Links ]
53. Fletcher L, Hayes SC. Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. J Ration Emot Cogn Behav Ther 2005;23(4):315-36. DOI: 10.1007/s10942-005-0017-7. [ Links ]
54. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav Ther 2004;35(4):639-65. DOI: 10.1016/S0005-7894(04)80013-3. [ Links ]
55. Robins CJ, Schmidt III H, Linehan M. Dialectical behavior therapy: Synthesizing radical acceptance with skillful means. In: Hayes SC, Follette VM, Lineham MM (eds.). Mindfulness and acceptance: Expanding the cognitive behavioral tradition. New York: Guilford Press; 2004. pp. 30-44. [ Links ]
56. Segal Z, Williams J, Teasdale J. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press; 2002. [ Links ]
57. Kanter JW, Busch AM, Rusch LC. Behavioral activation: Distinctive features. London: Routledge Press; 2009. [ Links ]
58. Kohlenberg RJ, Kanter JW, Bolling MY, et al. Enhancing cognitive therapy for depression with functional analytic psychotherapy: Treatment guidelines and empirical findings. Cogn Behav Pract 2002;9:213-29. DOI: 10.1016/S1077-7229(02)80051-7. [ Links ]
59. Ruiz FJ. A review of acceptance and commitment therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. Int J Psych Psychol Ther 2010;10(1):125-62. [ Links ]
60. Ferreira NB, Eugenicos M, Morris PG, et al. Using acceptance and commitment therapy in irritable bowel syndrome. Gastrointest Nurs 2011;9(9):28-35. DOI: 10.12968/gasn.2011.9.9.28. [ Links ]
61. Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: Model, processes and outcomes. Behav Res Ther 2006;44(1):1-25. DOI: 10.1016/j.brat.2005.06.006. [ Links ]
62. Hayes SC, Kirk DS, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. pp. 1-304. [ Links ]
63. Hayes SC, Follette VM, Linehan M, eds. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford Press; 2004. [ Links ]
64. Bach PA, Moran DJ. ACT in practice: Case conceptualization in acceptance and commitment therapy. Oakland, Califorina: New Harbinger Publications; 2008. [ Links ]
65. Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. London: Hachette UK; 2009. [ Links ]
66. Morgan D. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Psychother Res 2003;13(1):123-5. DOI: 10.1080/713869628. [ Links ]
67. Gregg JA, Callaghan GM, Hayes SC, et al. Improving diabetes self-management through acceptance, mindfulness, and values: A randomized controlled trial. J Consult Clin Psychol 2007;75(2):336-43. DOI: 10.1037/0022-006X.75.2.336. [ Links ]
68. Lundgren T, Dahl J, Hayes SC. Evaluation of mediators of change in the treatment of epilepsy with acceptance and commitment therapy. J Behav Med 2008;31(3):225-35. DOI: 10.1007/s10865-008-9151-x. [ Links ]
69. Hesser H, Westin V, Hayes SC, et al. Clients' in-session acceptance and cognitive defusion behaviors in acceptance-based treatment of tinnitus distress. Behav Res Ther 2009;47(6):523-8. DOI: 10.1016/j.brat.2009.02.002. [ Links ]
70. Veehof MM, Oskam MJ, Schreurs KMG, et al. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain 2011;152(3):533-42. DOI: 10.1016/j.pain.2010.11.002. [ Links ]
71. Vowles KE, McCracken LM. Comparing the role of psychological flexibility and traditional pain management coping strategies in chronic pain treatment outcomes. Behav Res Ther 2010;48(2):141-6. DOI: 10.1016/j.brat.2009.09.011. [ Links ]
72. Wicksell RK, Olsson GL, Hayes SC. Psychological flexibility as a mediator of improvement in acceptance and commitment therapy for patients with chronic pain following whiplash. Eur J Pain 2010;14(10):1059.e1-1059.e11. DOI: 10.1016/j.ejpain.2010.05.001. [ Links ]
73. Ferreira NB, Eugenicos M, Morris PG, et al. Using acceptance and commitment therapy to understand and improve outcomes in irritable bowel syndrome. Gastrointest Nurs 2011;9(9). [ Links ]
74. Ferreira NB. Investigating the role of psychological flexibility and the use of an acceptance and commitment therapy based intervention in irritable bowel syndrome (Doctoral dissertation). The University of Edinburgh; 2011. Available at: http://hdl.handle.net/1842/6312. [ Links ]
75. Ljotsson B, Andreewitch S, Hedman E, et al. Exposure and mindfulness based therapy for irritable bowel syndrome - An open pilot study. J Behav Ther Exp Psychiatry 2010;41(3):185-90. DOI: 10.1016/j.jbtep.2010.01.001. [ Links ]
76. Ljótsson B, Falk L, Vesterlund AW, et al. Internet-delivered exposure and mindfulness based therapy for irritable bowel syndrome - A randomized controlled trial. Behav Res Ther 2010;48(6):531-9. DOI: 10.1016/j.brat.2010.03.003. [ Links ]
77. Ljótsson B, Hedman E, Lindfors P, et al. Long-term follow-up of internet-delivered exposure and mindfulness based treatment for irritable bowel syndrome. Behav Res Ther 2011;49(1):58-61. DOI: 10.1016/j.brat.2010.10.006. [ Links ]
78. Kearney DJ, McDermott K, Martínez M, et al. Association of participation in a mindfulness programme with bowel symptoms, gastrointestinal symptom-specific anxiety and quality of life. Aliment Pharmacol Ther 2011;34(3):363-73. DOI: 10.1111/j.1365-2036.2011.04731.x. [ Links ]
79. Gaylord SA, Whitehead WE, Coble RS, et al. Mindfulness for irritable bowel syndrome: Protocol development for a controlled clinical trial. BMC Complement Altern Med 2009;9:24. DOI: 10.1186/1472-6882-9-24. [ Links ]
80. Zernicke KA, Campbell TS, Blustein PK, et al. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: A randomized wait-list controlled trial. Int J Behav Med 2013;20(3):385-96. DOI: 10.1007/s12529-012-9241-6. [ Links ]
81. Zomorodi S, Abdi S, Tabatabaee SK. Comparison of long-term effects of cognitive-behavioral therapy versus mindfulness-based therapy on reduction of symptoms among patients suffering from irritable bowel syndrome. Gastroenterol Hepatol Bed Bench 2014; 7(2):118-24. [ Links ]
82. Kanstrup M, Wicksell RK, Kemani M, et al. A clinical pilot study of individual and group treatment for adolescents with chronic pain and their parents: Effects of acceptance and commitment therapy on functioning. Children 2016;3(4).pii:E30. DOI: 10.3390/children3040030. [ Links ]
83. Ferreira NB, Gillanders D. Better living with IBS: A step-by-step program to managing your symptoms so you can enjoy life to the full! Narin: Exisle Publishing; 2012. [ Links ]
84. Ferreira NB, Eugenicos MP, Morris PG, et al. Measuring acceptance in irritable bowel syndrome: Preliminary validation of an adapted scale and construct utility. Qual Life Res 2013;22(7):1761-6. DOI: 10.1007/s11136-012-0299-z. [ Links ]
85. Aucoin M, Lalonde-Pasi MJ, Cooley K. Mindfulness-based therapies in the treatment of functional gastrointestinal disorders: A meta-analysis. Evid Based Complement Alternat Med 2014;2014:140724. DOI: 10.1155/2014/140724. [ Links ]
86. Altayar O, Sharma V, Prokop LJ, et al. Psychological therapies in patients with irritable bowel syndrome: A systematic review and meta-analysis of randomized controlled trials. Gastroenterol Res Pract 2015;2015:549308. DOI: 10.1155/2015/549308. [ Links ]
87. Bricker JB, Mann SL, Marek PM, et al. Telephone-delivered acceptance and commitment therapy for adult smoking cessation: A feasibility study. Nicotine Tob Res 2010;12(4):454-8. DOI: 10.1093/ntr/ntq002. [ Links ]
88. Lappalainen R, Lehtonen T, Skarp E, et al. The impact of CBT and ACT models using psychology trainee therapists: A preliminary controlled effectiveness trial. Behav Modif 2007;31(4):488-511. DOI: 10.1177/0145445506298436. [ Links ]
![]() Correspondence:
Correspondence:
Juan J. Sebastián Domingo.
Gastroenterology Unit.
Hospital Royo Villanova.
Av. San Gregorio, s/n.
50015 Zaragoza, Spain
e-mail: jjsebastian@salud.aragon.es
Received: 12-10-2016
Accepted: 22-01-2017