INTRODUCTION
According to the most recent data of the Mexican Instituto Nacional de Estadística y Geografía, there were 655,688 deaths in 2015 and cancer was the main cause in 85,201 cases (12.99%). Six cancer types were responsible for highest mortality. These included tracheal, bronchial and lung (6,903, 8.10%); prostate (6,447, 7.57%); liver and intrahepatic bile duct (6,333, 7.43%); breast (6,304, 7.40%); stomach (6,065, 7.12%) and colon, rectal and anal (5,853, 6.87%) 1. In 2013 in Mexico, gastric cancer (GC) was the third highest cause of death by cancer in people aged ≥ 20 years 2. The GC mortality has remained relatively stable in recent decades in Mexico 3 and a decrease in mortality from 7.5 to 5.6 per 100,000 inhabitants was reported during the period 2000-2012 2. There are few reports in Mexico that detail stage at diagnosis, two studies carried out in tertiary hospitals indicated that 5.4% 4 and 3% 5 of cases are diagnosed at early stages. Simultaneously, studies in China, the Unites States and South Korea report an early diagnosis in 13.8% 6, 16.7% 7 and 87.7% 8 of cases, respectively.
Helicobacter pylori (H. pylori) is an established cause of GC. The reduction in prevalence of this pathogen can be explained partly by a reduced exposure to this bacterium and the increased use of refrigeration to preserve foods 9. However, infection by H. pylori may be a necessary but insufficient condition alone for the development of some types of GC 10. In Mexico, there is no difference in prevalence of H. pylori infection between urban and rural communities 11.
Heavy drinkers and tobacco users are at significantly higher risk of GC 12,13. Consumption of fruits, non-starchy and allium vegetables are factors that probably reduce GC risk. In contrast, the consumption of salty foods probably increases the risk 9. In Mexico, there is limited but a suggestive level of evidence that the consumption of chili, smoked foods, processed meats and grilled meats are factors that increase the risk of developing GC 14. In addition, a study reported an association between GC and the perception of the omission of breakfast and non-refrigeration of food 15.
The scientific evidence indicates that GC is preceded by a long period of latency 16 and an estimated 8% of cases have a familial background 17. Diet is linked to as many as 35% of GC deaths 18 and dietary risk factors for subjects with a first-degree relative with GC are no different from the risk factors established in the general population 19. This supports the design of public health strategies directed towards primary prevention of GC, focused on promoting and conducting protective actions and diminishing exposure to established risk factors. Moreover, prevention of GC has been considered as the most promising strategy to control the disease, hence clinical treatments have had no major impact on survival 16.
An epidemiological and medical approach of primary GC prevention are key to identifying subjects exposed to risk factors and who require intervention. These subjects could be identified via the Questionnaire to Find Factors Associated with Gastric Cancer (QUFA-GC(c)). This questionnaire was constructed after a meticulous review of the literature and was subsequently validated by a committee of experts and applied in the Mexican population during 2009-2010 15. The aim of this study was to use the QUFA-GC(c) to identify factors associated with the development of gastric cancer (GC) in the local population. The study hypothesis is that the failure to consume a suitable breakfast is associated with the development of GC.
METHODS
Characteristics of the study
The study included cases and controls paired by sex and ± 10 years of age at diagnosis The study was approved by the ethics committee of the "Dr. Miguel Dorantes Mesa" tertiary reference hospital and the "Dr. Luis F. Nachón" secondary reference hospital, both within the Veracruz State Health Service, Mexico. These hospitals are attended by people with no access to a social security scheme linked to the formal labor market. This study was conducted according to the principles of the Declaration of Helsinki and the Mexican General Health Law.
Interviewer training
Prior training was conducted with respect to the sections and questions of the QUFA-GC(c). The interviewer performed the questionnaire with 30 patients that attended the "Dr. Luis F. Nachón" hospital.
Subjects
Cases were defined as patients that attended the "Dr. Miguel Dorantes Mesa" hospital with a confirmed histopathological diagnosis of adenocarcinoma-type GC, as reported in the hospital records from May 2015 to May 2016. Controls were blood bank donors from the same hospital and were also recruited from May 2015 to May 2016.
Sample size
Perception of the omission of breakfast was considered as the main risk factor, with an exposure frequency of 71.4% assumed for cases and 15.4% for controls, with an estimated OR of 13.7 15. The minimum sample size calculated was 21 pairs of cases and controls (1:1) with a 95% confidence level and 95% statistical power.
Sampling
All GC patients who attended the "Dr. Miguel Dorantes Mesa" hospital during the inclusion period were considered as possible cases (n = 72). All blood bank donors from the same hospital during the same period were considered as possible controls (n = 175). After pairing by sex and ± 10 years at age of diagnosis, 46 pairs were obtained, which exceeded the minimum sample size.
Informed consent was obtained from all participants. All possible cases and controls were surveyed during the inclusion period as in our experience, about 70% of the patients are not reachable by telephone and their places of residence are usually located in difficult access areas.
Variables
Perception of the omission of breakfast: perception of the omission of breakfast of the interviewee 15. Breakfast: food or liquid consumed by the interviewee within two hours of waking. Food groups I-V: I) breads and cereals; II) vegetables; III) fruit; IV) dairy products; and V) meat, eggs, vegetarian meat alternatives and nuts 20. Extra food: food or drink not categorized into one of the groups I-V, which includes items high in sugar and/or saturated fat such as chocolate, soft drinks, cakes and pastries 20. Non-suitable breakfast of type 1 and 2: type 1 is no food or beverage, or water only and type 2 is food and/or beverage from the "extra" foods category only 20,21. Suitable breakfast of type 3, 4 and 5: type 3 is food or beverage from one food group; type 4 is food and/or beverage from two food groups; and type 5 is food and/or beverage from three or more food groups 20. Consumption capsaicin per day: estimate of capsaicin intake in mg/day according to the type of chili and quantity ingested reported by the interviewee. The concentrations of capsaicin were as follows: habanero, 8.55 mg/g; de árbol, 2.35 mg/g; jalapeño, 2.08 mg/g; and piquín, 1.44 mg/g 22. Weight per chili were one piece of habanero, 67 g; one piece of chili de árbol, 7 g; one piece of jalapeño, 78 g; and a tablespoonful of chili piquín, 8 g 23. Consumption of capsaicin per day was classified as high (> 29.9 mg) and low (≤ 29.9 mg). Consumption of pickled foods per day: estimation of the consumption of pickled foods in g per day, as reported by the interviewee, classified into ≤ 32.42 g per day or > 32.42 g per day. Consumption of fresh fruit: estimation of the consumption of pieces of fresh fruit per day according to the perception of the interviewee, classified into < 1 piece per day and ≥ 1 piece per day. Consumption of fresh vegetables: estimation of the consumption of pieces of fresh vegetables per day according to the perception of the interviewee, classified into < 1 piece per day and ≥ 1 piece per day. Eating rapidly, always or almost always: perception of interviewee of the speed of food ingestion. Consumption almost always or always of very hot food and drinks: perception of the interviewee of the frequency of consumption of very hot drinks and food per day. Use of refrigerator to conserve foods: daily use of a refrigerator at home reported by the interviewee. Period of tobacco consumption: number of years smoking ≥ 1 cigarette per month reported by the interviewee, classified into ≥ 10 years or < 10 years of tobacco consumption. Period of alcoholism: number of years consuming ≥ 1 alcoholic drink per month as reported by the interviewee, classified into ≥ 10 years or < 10 years of consumption of alcoholic drinks. Income was determined by dividing the monthly family income in USD by the number of inhabitants in the house. This was classified according to the standards of the Mexican government as an income that reflects poverty (≤ 276.14 USD) or income that does not reflect poverty (> 276.14 USD). Educational level: highest educational level reported by the interviewee which was classified as no formal education and Primary or above. Recreational exercise: taking of recreational exercise on ≥ 1 occasion per week as reported by the interviewee 9. Body mass index (BMI) was classified as follows: low, < 18.50 kg/m²; normal, 18.50-24.99 kg/m²; overweight, 25.00-29.99 kg/m²; and obesity, ≥ 30.00 kg/m² 24. Anemia was classified as < 13 g/dl of hemoglobin in males and < 12 g/dl of hemoglobin in females 25. Level of platelets were classified as follows: low, < 150,000 x 109/l; normal, 150,000-450,000 x 109/l; and high, > 450,000 x 109/l 26.
Data collection
The QUFA-GC(c) was used to collect data. QUFA-GC(c) is a section of the Questionnaire to Find Factors Associated with Diseases of the Digestive Tract, which was previously validated at the same hospital 15. The QUFA-GC(c) comprised the following elements: interviewer data, general data of the participant, socioeconomic information, food, regularity of food consumption, speed and quantity of food consumption, consumption of salt, consumption of very hot food and drinks, use of a refrigerator, physical activity, consumption of tobacco, consumption of alcohol, personal history of cancer, family history of cancer, medication, associated illnesses and treatment (such as H. pylori infection), clinical procedures, symptomatology and clinical data. QUFA-GC(c) is available on request by email to csampieri@uv.mx.
Statistical analysis
Minimum sample size was calculated using the program Epidat version 3.1. In the univariate analysis, proportions and means were compared by Chi-squared and Student's t tests, respectively. Risk factors were estimated by OR for paired cases by sex and ± 10 years at age of diagnosis with a 95% CI. Multivariate analysis was carried out by logistic regression adjusted using the forward conditional method. The initial model included all of the variables that presented differences in the univariate analysis and that had not been included in health promotion programs of the Mexican government. The dependent variable was GC diagnosis and the covariates were sex, age, marital status, educational level, income, occupation, histopathological classification, site of tumor, clinical framework, body mass index, hemoglobin level, level of platelets and blood type. Statistical significance was considered at p < 0.05. Analyses were performed using the IBM SPSS Statistic for Windows version 23, Epidat version 3.1, R Stats Package and R Software. A decision tree was constructed with the WEKA software version 3.8.0 using the J48 algorithm. This procedure builds decision trees from data by iteratively adding nodes that minimize entropy 27,28.
RESULTS
Forty-six cases and controls paired by sex and ± 10 years of age at diagnosis (response rate: 100%) were included. All subjects were interviewed face to face by a single qualified interviewer. Cases responded to the QUFA-GC(c) in a mean of 18.65 ± 5.07 minutes (mean ± SD) and controls, in 11.43 ± 2.58 minutes. The sociodemographic and clinical characteristics of the studied population are shown in table 1. There were differences between the groups in terms of income and there were no differences with regard to age and marital status (Table 1). According to the classification of Lauren, diffuse and intestinal GC types were found in equal percentages and the most common tumors occupied ≥ 2 sites (C16.8) and the cardia site (C16.0). Involuntary weight loss, sensation of fullness and nausea were the most common symptoms (Table 1). A considerable proportion of the controls (19.6%) reported pyrosis (Table 1). There were no differences with regard to the geographic and Mexican sanitary jurisdictions in which cases and controls have lived for most of their lives (data not presented).
Table 1 General characteristics of the subjects included: n (%)


NA: not applicable; SD: standard deviation. *In cases corresponding to the time of diagnosis. †Expressed in USD. ‡Adapted from the Instituto Nacional de Estadística y Geografía de México 29. §According to the International Statistical Classification of Diseases and Related Health Problems 10th Revision.
The H. pylori status of most of the subjects included in the study was unknown and only three cases had a H. pylori infection; two at the time of GC diagnosis and one three years prior to GC diagnosis. One control had an infection ten years prior to the interview and was diagnosed via gastric biopsy. Seven subjects had undergone an endoscopy in a stomach disease clinic prior to diagnosis of GC, gastric biopsies were obtained in three cases. The type of gastritis that existed prior to diagnosis of GC was unknown.
The probable factors associated with GC are detailed in table 2. We found associations between GC and no formal education, consumption of a non-suitable breakfast within two hours of waking, eating rapidly almost always or always, consumption always or almost always of very hot food or drinks, having smoked for ≥ 10 years, consuming > 32.42 g of pickled foods per day, and consuming > 29.9 mg of capsaicin per day. In contrast, a protective association was found between GC and the habit of taking recreational exercise, consuming ≥ 1 piece of fresh fruit per day and consuming ≥ 1 piece of fresh vegetable per day. No association was found between the development of GC and not using a refrigerator to conserve foods, the perception of the omission of breakfast and a period of alcoholism ≥ 10 years (Table 2).
Table 2 Association between sociodemographic characteristics, habits, diet and pathological history of gastric cancer

OR: odds ratio paired by sex and ± 10 years of age at diagnosis.
When income was classified into two classes, one reflecting poverty and one that does not reflect poverty, 97.8% (45/46) of the cases and 87.0% (40/46) of the controls had an income that reflected poverty. There were no differences between the groups (p value > 0.05). It was not possible to estimate OR paired by sex and ± 10 years of age at diagnosis using the variable of income that reflects poverty, since values of zero were obtained with this analysis. Nevertheless, there were differences in income between the groups when the variable was analyzed in a continuous manner (Table 1).
Two models were constructed using multivariate analysis and nine variables formed the initial model. Variables were removed in order to improve statistical efficiency (Table 3). In the final model, having no formal education, consuming a non-suitable breakfast within two hours of waking and an estimated consumption of > 29.9 mg capsaicin per day were factors associated with the development of GC. This model had accuracy values of 87.0% for cases and 76.1% for controls (Table 3).
Table 3 Multivariate analysis

Multivariate analysis conducted using logistic regression with the R Stats Package and IBM SPSS. SE: standard error; CI: confidence interval; OR: odds ratio. *Initial model was obtained by the enter method. †Final model was adjusted by the forward conditional method. p value Hosmer and Lemeshow test = 0.51; -2 Log likelihood = 82.08; Cox & Snell R square = 0.39; Nagelkerke R square = 0.52; areas under the ROC curve, initial model = 0.90, final model = 0.87.
In addition, an inductive learning analysis was performed using a decision tree produced by the J48 algorithm with the variables included in the multivariate model (Table 3). According to this algorithm, educational level was selected as the most informative for the classification of GC, followed by the breakfast type within two hours of waking and the consumption of capsaicin. This classification method was able to correctly classify the observation with a precision of 86.9% of the GC cases and 73.9% for the controls (Fig. 1).
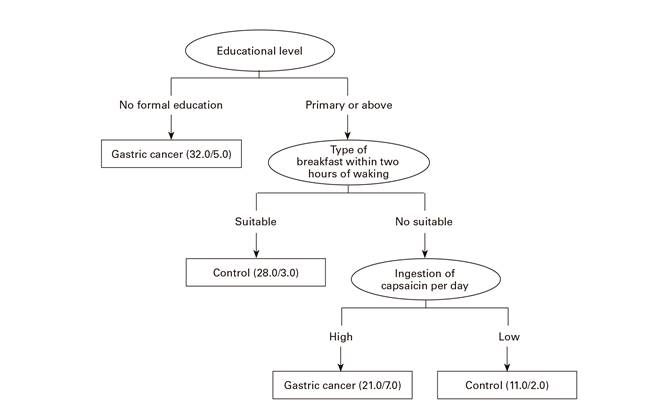
Fig. 1 Decision tree model for factors associated with gastric cancer. Elliptic nodes show the variables found by the J48 algorithm as the most informative to predict the class variable diagnosis (shown as rectangles). Values of the variables are shown in the arcs of the tree. Classification statistics are shown in brackets. The first term represents the total number of instances under this category (n); the second number represents the number of instances that were incorrectly classified (e). Then, the classification error in each node can be computed as the ratio e/n.
DISCUSSION
The Mexican Health System aims to design and validate health interventions that allow the development of effective and efficient policies of disease prevention. In this context, it is vital that the Mexican population be educated with regard to habits that could be considered as risk or protective factors of GC. The data compiled via the QUFA-GC(c) could function as a useful tool for identifying subjects with an exposure to risk factors for the development of GC.
In Mexico, GC is a public health problem 1,2. Unfortunately, there is still no official Mexican standard (norma oficial mexicana) for the prevention, detection, treatment and control of GC 3. Despite knowing the mortality of cancer in Mexico, it took until 2016 for the entire Mexican Chamber of Deputies (lower house of the federal government) to approve a project to create the National Cancer Register as an instrument to prevent and reduce the number of deaths from cancer. Political will is required for the Mexican government to invest in cancer prevention and in early detection programs.
Lack of a formal education has previously been associated with the development of cancer 30,31; it is conceivable that the lack of a formal education is a powerful determinant of the particular diseases that people will develop, as well as how they react to that disease. A study in Japan reported an inverse correlation between education level and death from GC in males 32. In Mexico, this factor represents a window of opportunity via educational interventions.
To our knowledge, this is the first study of paired cases and controls in the Mexican population that associates the consumption of an inadequate breakfast within two hours of waking with the development of GC. Even though the perception of the omission of breakfast was not associated with GC. A previous cross-sectional analytical study reported that the perception of the omission of breakfast was as a factor associated with GC 15. However, we consider that these apparently conflictive data can be explained by the particular design of each study. A study in China reported that irregular eating was associated with GC 32; while it is not the same variable, it can be speculated that it is an example that coincides with our findings. We consider that a poor quality breakfast, which could be eating nothing or water only, causes an alteration of the natural environment of the stomach. This promotes a susceptibility to infections and the precursor condition, since food intake is the strongest natural stimulus for the secretion of gastric acids and omitting breakfast is associated with chronic gastric ulcers 33. Omission of breakfast has recently been associated with all causes of mortality in Japan 34.
Another factor associated with development of GC was the consumption of > 29.9 mg of capsaicin per day, which is consistent with other studies 9,22. According to reports 9,22,23, we estimate that the consumption of > 29.9 mg of capsaicin can be achieved by ingesting one habanero chili, two chilies de árbol, one jalapeño chili or three tablespoons of piquín chili.
We found that the length of a smoking habit was associated with GC but not with the length of an alcoholism habit. Studies of the links between these habits and GC are controversial 35,36. An association was found between protection against GC and the consumption of fresh fruit and vegetables, which is consistent with recommendations for the prevention of cancer 9. Recreational exercise was a variable associated with protection against GC, which is consistent with other studies 37,38. The use of a refrigerator was not associated with development of GC. The decline in GC is likely to have been partly due to the increased availability of refrigeration 9. Differences were found by univariate analysis with regard to income among the groups. However, when this variable was analyzed according to the parameter used by the Mexican government to define an income that reflects poverty, no differences were apparent.
For the prevention of GC, it is important to conduct longitudinal studies in order to identify risk profiles in specific population groups for intervention in subjects with an elevated risk of GC development. Similar models for other types of cancer have been performed in other countries 39,40. However, the establishment of risk patterns in Mexico is challenging due to the wide genetic, sociocultural, climatological, geographical, dietary and linguistic diversity. For example, in Mexico in 2005, more than 90 indigenous languages were identified 41 and the incidence rate of poverty in 2014 was 53.2% 42.
This study has different limitations, the sample size used may seem small but exceeds the expected sample size. Due to the complexity of our geographic region and social conditions, all possible cases (n = 72) and controls (n = 175) were surveyed. However, a low match rate was obtained (n = 46). We believe that this was a consequence of differences in age and sex between the possible cases and possible controls.
A further limitation is that the status of H. pylori infection prior to development of GC was unknown in most of the cases. This can be explained by the low percentage of the population with access to social security 43 and the lack of programs for H. pylori detection. Finally, consideration must be given to the limitation of memory bias, which is typical of case-control studies that collect information retrospectively.
The strengths of this study were the type of design and the selection of controls, as they came from the same geographic area as the cases. Thus complying with the assumption that, if these subjects were to develop the disease, they could be placed in the cases group 44.
In conclusion, after applying the QUFA-GC(c), the multivariate analysis revealed three factors associated with the development of GC. These were lack of formal education, consumption of an inadequate breakfast within two hours of waking and an estimated consumption of > 29.9 mg of capsaicin per day.













