INTRODUCTION
Irritable bowel syndrome (IBS) is a chronic, functional gastrointestinal disorder characterized by abdominal pain and a change in bowel habits. The global prevalence of IBS ranges from 5% to 15% and the prevalence of IBS in Spain has been estimated at 10% via a personal interview, home-based study of 2,000 individuals in the general population 1,2. However, prevalence estimates can vary depending on the diagnostic criteria used. Prevalence estimates from a study in the UK, USA and Canada, with the currently used Rome IV criteria, appear to be lower. The range was 7.1% to 7.5% for females and 3.6% to 5.1% for males 3. IBS with constipation (IBS-C) is a subtype of IBS where pain persists with difficult, infrequent or incomplete defecation 4. IBS-C has been associated with poor health-related quality of life, greater loss of work productivity and impairment of activity, and an increased use of healthcare resources, as compared with people without IBS-C 5.
Treatment modalities for IBS-C depend on symptom severity 6. In Spain, initial treatments can involve patient education of IBS and instructions for a specific, balanced diet and exercise 6. Other methods for managing constipation include increased fluid intake and soluble fibers, as well as osmotic/stimulant laxatives 4,6. Treatment for pain includes spasmolytics and mint essence, as well as antidepressants such as serotonin reuptake inhibitors, including fluoxetine. Psychological treatments such as cognitive behavioral therapy and hypnosis may also provide relief.
Linaclotide, a guanylate cyclase-C receptor agonist, is approved for the treatment of IBS-C in Spain. It has been shown to be effective in Phase 3 clinical trials for the European Medicines Agency responder endpoints (abdominal pain/discomfort and degree of relief) and is also safe to use 4,7,8. In a meta-analysis, linaclotide treatment also improved bowel function and reduced abdominal pain and overall symptom severity compared with the placebo 9. Successful treatment of IBS requires a strong relationship between the healthcare provider (HCP) and the patient 10,11, where the HCP educates the patient regarding the utility and safety of available diagnostic tests and treatments 4. In a randomized clinical trial of patients with IBS from Boston, Massachusetts, in the USA, a supportive patient-HCP relationship was shown to significantly improve symptoms and quality of life 12.
However, the diagnosis and management of IBS can be challenging for HCPs. IBS is a heterogeneous disorder and symptoms are often non-specific and can also be somatic or psychological in nature. Furthermore, the response to treatment can vary 13. In addition, treatment failure is common, resulting in increased use of healthcare resources, despite the variety of therapeutic options available. A claims-based study of a US population that received public funding (Medicaid) found that over 50% of patients with IBS-C and patients with chronic constipation had more than one indicator of treatment failure. These included switching from one treatment to another, use of a more aggressive prescription and an inpatient stay or visit to an Emergency Department even after treatment 14. Overall, previous studies in Spain and the UK have demonstrated that patients are skeptical about the treatments they receive. They feel they have insufficient knowledge of IBS and do not perceive a benefit from their treatments 11,15.
An understanding of perceptions of public healthcare is important as 71.5% of healthcare spending in Spain was in the public sector in 2013 16. A previous study in Spain analyzed the problems experienced with IBS management within the public healthcare system, from both a patient and HCP perspective 11. Patients were most concerned with delays in confirming a diagnosis and the inability to understand IBS and cope with the disease on a daily basis. HCPs felt that the greatest difficulty in treating patients with IBS was the low adherence to treatment plans. Further understanding of the barriers to achieving a positive patient-HCP relationship may help to improve patient outcomes 11. This study aimed to assess the perceptions of the care received in the public healthcare system by patients with IBS-C who also received private healthcare in Spain. The study used established patient questionnaires to identify the barriers to receiving proper care. A previous survey indicated that 73% vs 31% of patients with IBS viewed their gastroenterologist (GE) vs their primary care physician (PCP) as being a source of knowledge about IBS 11. This led to the hypothesis that more patients in private healthcare would prefer the care given by a GE rather than a PCP in the public healthcare system for IBS-C.
MATERIAL AND METHODS
Study design and patient selection
This was a multicenter, cross-sectional observational study of patients aged ≥ 18 years who had previously received care from a PCP and/or a GE in the public healthcare system and who subsequently attended a private GE consultation due to constipation and abdominal discomfort. Subjects met two criteria at the time of survey completion during the visit. One criterion was that patients experienced constipation and abdominal discomfort, with no confirmed previous IBS diagnosis. Constipation was defined as a patient's perception of a reduction in the frequency of bowel movements and difficulty with bowel movements, and abdominal discomfort included any symptoms of pain, discomfort, abdominal distension, abdominal bloating and flatulence. The second criterion was that patients met the Rome III criteria for IBS 17, including the presence of pain or abdominal discomfort (symptoms present for at least three days a month in the past three months, having started a minimum of six months previously) combined with two or more of the following symptoms: pain improved with defecation; the onset of pain was associated with a change in bowel movement frequency; and the onset of pain was associated with a change in stool form (based on the Bristol Stool Form Scale 18)). No patients were excluded based on IBS subtype. Written informed consent was obtained from each patient included in the study.
Patients were excluded if they did not sign the informed consent for the study, had any medical or psychological disorder that could limit their ability to understand and answer questions regarding their condition, or had any clinical history suggestive of the presence of any gastrointestinal-related disease other than IBS. These included: unexplained weight loss, fever, blood in the stool, previous ingestion of antibiotics, onset of symptoms aged over 50 years, family history of bowel cancer, IBS or celiac disease, and ongoing bowel cancer or suspicion of celiac disease or gluten-sensitive enteropathy. The Clinical Research Ethics Committee of the Hospital Clínic de Barcelona was responsible for evaluating the study ethics and approval of the study was granted by the Committee on the 13th of March 2015. The study protocol conforms with the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in the ethical approval by the human research committee of the Hospital Clínic de Barcelona.
Primary and secondary objectives
The primary objective of this study was to determine the perceptions of patients with IBS visiting GE specialists in the private healthcare system in relation to the care they received from PCPs and GE specialists in the Spanish public healthcare system. The secondary objectives were to determine the severity of IBS and the health-related quality of life. Patients' perceptions of care from PCPs and GEs in public healthcare and treatments received from public healthcare were evaluated via the IBS Patient Experience questionnaire 11. Symptom severity and health-related quality of life were assessed using the IBS Symptom Severity Score questionnaire 19 and the EuroQol five-dimensions 20,21,22 questionnaire, respectively.
Questionnaires
A total of 174 GE specialists from the private healthcare system were recruited into the study and data was collected from patients between the 2nd of March 2015 and the 16th of October 2015. A total patient population of 897 was estimated in order to evaluate the primary endpoint, considering an expected satisfaction percentage of 70%, 3% accuracy and 95% confidence level. The GE specialists selected patients who met the inclusion criteria. The selected patients provided their medical history and completed three questionnaires regarding their current symptoms and previous experiences with the public healthcare system within a single visit.
The IBS Patient Experience questionnaire developed in Spain 11 was used to determine patients' perceptions in relation to the public healthcare they had previously received. The questionnaire comprised questions with a yes/no response that related to experiences with PCPs and GEs in the public healthcare system. This included questions on topics such as the ability of the provider to provide comprehensible explanations of IBS and control of IBS symptoms via treatment or lifestyle changes, as well as their ability to listen. This questionnaire was validated by comparison to other findings from similar studies in the United Kingdom 23 and Boston in the USA 24. The IBS Symptom Severity Score questionnaire 19 was used to characterize the severity of IBS. The results were based on a visual analog scale and the overall symptom severity score was defined using the following formula: pain severity + distension severity + satisfaction with bowel habits + impact of symptoms. Severity was presented on a scale of 0-100, where 0 indicated no pain and 100 indicated the greatest pain severity. Patients completed the EuroQol five-dimensions questionnaire 20,21,22 to describe their health-related quality of life. Patients reported whether they had no problems, mild problems, moderate problems, severe problems or a complete incapacity in lifestyle categories including mobility, personal care, everyday activities, pain/discomfort and anxiety/depression. The IBS Patient Experience questionnaire 11, the IBS Symptom Severity Score questionnaire 25) and the EuroQol five-dimensions questionnaire 26,27 have been adapted and validated for use in Spain.
Statistical analysis
The number of patients was recorded and relative frequencies (percentages) were calculated for each categorical variable. With regard to continuous variables, the mean, standard deviation, median, minimum and maximum were calculated where applicable. Percentages were calculated considering the total number of patients with available data. Statistical analyses were performed using SPSS Statistics version 23.0 (IBM SPSS, Inc., Chicago, IL, USA).
RESULTS
Patient demographics and characteristics
A total of 926 patients were recruited and 922 had recorded patient histories and completed questionnaires; 707 evaluable patients were analyzed (Fig. 1). The mean age was 45.6 years and 80.9% were female (Table 1). The majority of patients in the study had IBS-C (87.1%), with an overall mean bowel movement frequency of two times per week (range, 0-25) and comorbidities including headaches (35.6%), back pain (28.1%) and insomnia (23.8%). The most common recurring IBS symptoms included pain (81.6%), abdominal distension (67.6%) and bloating (66.6%).
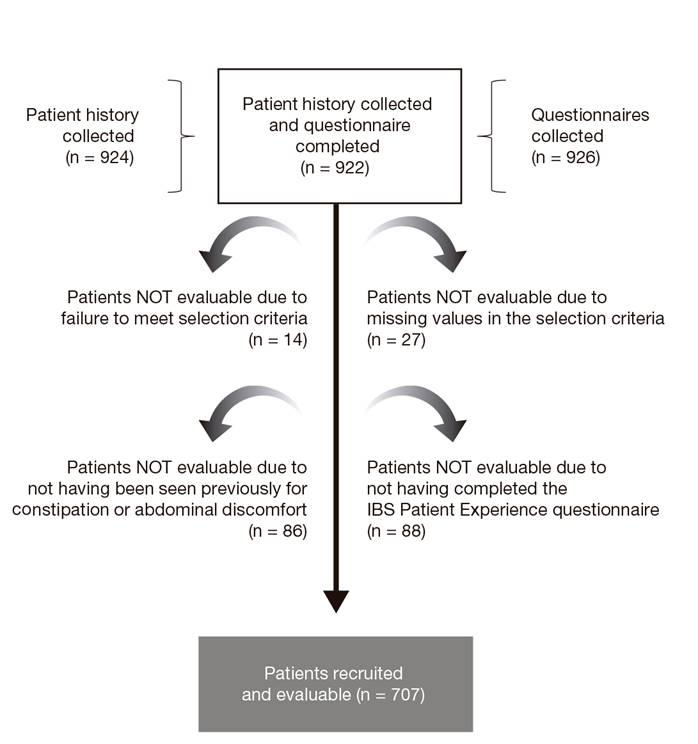
Fig. 1 Patient recruitment. The IBS Patient Experience questionnaire was developed by the Spanish Society for Quality in Healthcare (Sociedad Española de Calidad Asistencial).
Table 1 Patient demographics and disease characteristics


Percentages were calculated considering the total number of patients with available data. *Treatments may include those received in the public or private healthcare system. GE: gastroenterologist; GI: gastrointestinal; HCP: healthcare provider; IBS: irritable bowel syndrome; IBS-C: irritable bowel syndrome with constipation; IBS-D: irritable bowel syndrome with diarrhea; PCP: primary care physician; SD: standard deviation.
Most patients had seen a public PCP (80.5%) or GE (63.4%) within the past 12 months. The main reasons patients reported for visiting a private GE were to seek a second opinion (41.4%) or because they felt that their public HCP had not satisfactorily resolved their condition (36.6%). Less than half of the patients (45.9%) reported that their medical public and/or private healthcare visits included an explanation of the condition, the physician listened to them, established prognostic limits or involved them in the treatment. The median time elapsed since symptom onset and their first visit to a HCP for their symptoms was three and two years, respectively.
With regard to socio-economic characteristics, patients had various levels of education and most had completed university studies (34.9%). Although the majority of patients were working (64.8%), some patients reported being unemployed (17.7%), unfit for work (6.8%) or on leave from work (4.2%). Many patients reported no problems with their employment (64.4%). However, some patients reported a lack of understanding from co-workers (17.2%) and that IBS symptoms affected their ability to look for work (7.0%), to maintain academic performance (7.0%) and to maintain a work position (4.1% left or changed work and 2.6% took leave from work).
Patient perceptions of treatment and the care received in the public healthcare system
Patients in this study received various treatments in the public and/or private healthcare system, including a specific diet, exercise, alternative medicines and pharmacological treatments (Table 1). With regard to perceptions of treatment received from the public healthcare system, the majority of patients (73.1%) understood what the medication was and how it should be administered (Table 2). However, a high proportion of patients observed no (11.7%), little (47.0%) or some (25.9%) improvement in their condition as a result of the treatment. A similar proportion of patients (60.1%) discontinued their medication as it did not suit them or did not improve their condition.
Table 2 Patients' perceptions of treatment in the public healthcare system

Percentages were calculated considering the total number of patients with available data.
With regards to care received in the public healthcare system, patients had a more positive perception of their GE than their PCP in terms of listening (77.4% vs 59.4%) (Fig. 2). During communications between patients and their HCP, more patients felt that their GE provided enough time for consultation compared to their PCP (53.5% vs 30.5%). Furthermore, patients were provided with written advice on treatment and management of IBS more often by their GE than their PCP (50.1% vs 28.9%). Fewer patients felt they were wasting their time when attending a consultation with their GE (27.8%) compared to their PCP (52.4%). More patients trusted that their GE was knowledgeable about their condition and chose the appropriate treatment (63.6%) compared with their PCP (33.7%). Overall, 74.2% of patients thought that coordination between PCPs and GEs was fair, poor or very poor. Patient perceptions were generally more positive towards their GE (62.8%) than their PCP (43.9%).
Symptom severity
Patients reported frequently suffering from both abdominal pain (90.0%) and distension (91.5%) in the IBS Symptom Severity Score questionnaire (Table 3). With regard to severity, the mean scores (± standard deviation) were all over 50 (abdominal pain: 58.3 ± 18.3; abdominal distension: 61.9 ± 17.9; satisfaction with bowel habits: 73.2 ± 21.7; interference of IBS with life in general: 61.5 ± 21.1). The overall symptom severity score was 258.6 ± 57.5 and the majority of patients were considered to have moderate (68.9%) or severe (21.7%) symptoms.
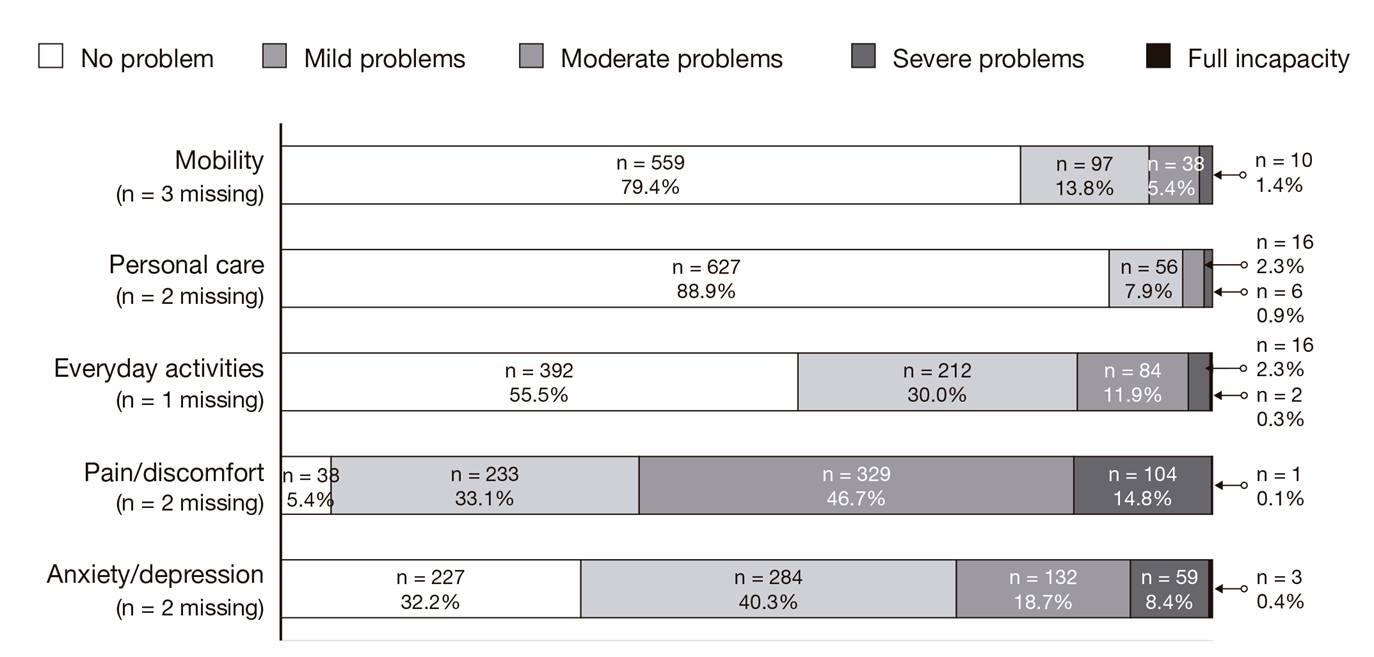
Impact of ibs on patients' health-related quality of life
The majority of patient-reported problems were pain/discomfort and anxiety/depression, followed by problems with everyday activities (Fig. 3). Over 90% of patients had pain/discomfort, with many reporting mild (33.1%), moderate (46.7%) and severe (14.8%) problems. About two-thirds of patients had anxiety/depression, with many reporting mild (40.3%), moderate (18.7%) and severe (8.4%) problems. Approximately half of patients had problems with everyday activities as follows: mild (30.0%), moderate (11.9%) and severe (2.3%). The majority of patients did not have any problems with mobility (79.4%) or personal care (88.9%).
DISCUSSION
The majority of patients within the study cohort throughout Spain felt that their PCP did not provide enough time during their consultation to explain the problem. These results parallel a previous online study that found that a little over half of patients (n = 106, 54%) characterized their relationship with their HCP as negative. The primary concern was that HCPs did not provide enough empathy and listening time for patients to explain how IBS affected their lives 10. However, this study was not performed in Spain, therefore, a direct comparison cannot be made.
Nevertheless, a greater number of patients consistently reported more positive feelings towards GEs than PCPs for every question in the questionnaire. More patients felt that their GE was knowledgeable about IBS and chose the appropriate treatment (63.6%) compared to their PCP (33.7%). This is similar to a previously reported study of a Spanish population, where 73% of patients felt that their GE was knowledgeable about IBS compared with 31% for PCPs 11. Even though patients felt more positive about their GE than their PCP, 27.8% still felt that they were wasting their time attending a consultation and 37.2% were not satisfied with the care they received from their GE. This study confirmed several barriers that led to a lack of patient satisfaction, including not enough time spent with the HCP and a lack of information on IBS. This is similar to that reported previously 11.
Typical symptoms were reported in this study, including abdominal pain and distention, and many patients had experienced symptoms for several years before diagnosis. Patient health-related quality of life was diminished, with patients suffering limitations in daily activities and experiencing pain/discomfort and anxiety/depression. Results from the EuroQol five-dimensions questionnaire were similar to those reported by a German population, where the majority of patients reported moderate to severe problems with pain/discomfort, followed by anxiety/depression 28. Over half of the patients observed some, little or no improvement of IBS as a result of their treatment. This is likely due to the general reservation patients have about the efficacy of available IBS treatments, as described in previous studies from Spain and the UK (11,15), rather than the use of public vs private healthcare.
The diagnosis and management of IBS can be challenging regardless of the attending HCP type. Altered peripheral regulation of gut function, altered brain-gut signaling and psychological distress have all been identified as potential components of IBS symptoms. However, a single integrated explanatory model for IBS has not yet been developed 29. A combination of physiological, psychological and social aspects of IBS could influence symptom severity, health-related quality of life and the global perception of the disease. Factors such as lifestyle habits or comorbidities, such as dyspepsia and psychological abnormalities, among others, could also influence and contribute to the complexity of the disease. Although PCPs can identify IBS symptoms, they have a heterogeneous view of the causes of IBS and relatively few PCPs have heard of formal diagnostic criteria (Manning or Rome) 30. Although GEs are aware of clinical guidelines for the diagnosis and management of IBS, studies have shown that they do not systematically follow these guidelines. Eighty per cent of respondents to a survey of GEs in Spain managed IBS symptoms using their own criteria based on a patient's symptoms 1. A survey of international PCPs, GEs and IBS experts found that IBS was often endorsed as a diagnosis of exclusion, which resulted in an increased use of healthcare resources 31. Developing research on the mechanisms of IBS, conceptualizing IBS using explanatory models for clinical practice and increased education initiatives for both patients and HCPs will improve patient-HCP communication of IBS and may help to overcome these barriers.
Although findings from this study mirror those of previous studies, limitations must be taken into consideration when interpreting the results. There may be bias resulting from the exclusive participation of patients from private practices, who may have a different socio-economic status from those routinely using the public healthcare system. Those who never received private healthcare due to various reasons such as lack of resources were not included. This study focused on perceptions of patients attending a private rather than public consultation, as the majority of these patients had experienced both healthcare systems, switching from the public to the private system when seeking care for their IBS-C symptoms. Therefore, observations may be more applicable to certain autonomous regions that have higher rates of private care. In 2014, approximately 56% of all private hospitals were located in Catalonia, Madrid and Andalusia and the greatest number of private hospitals among the total hospitals were in Catalonia, Navarra and Galicia 16.
Participants who suffered delays or a misdiagnosis of IBS-C while receiving public healthcare that resulted in a dissatisfaction with the system and those who were concerned about malignancies and thus demanded further diagnostic evaluations such as colonoscopy may also influence our findings. Although patients were asked to provide their perceptions on PCPs and GEs in the public healthcare system, patients may have assessed private healthcare GEs previously sought for consultation, rather than those in the public system. These patients may have returned to visit the same GE as they had built trust from previous consultations. Abdominal symptoms reported by some patients may have been due to other disorders rather than IBS and patients with diarrhea were not excluded. Therefore, patients with a false diagnosis may have been included. In addition, only patients meeting the Rome III criteria during the private GE visit and hence diagnosed at the time of completing the survey were included. This was to avoid the bias towards past medical practices when a proper diagnosis of IBS was less common 3.
CONCLUSIONS
In this study, patients with IBS-C reported that their symptoms affected their health-related quality of life; these symptoms included abdominal pain and distention. Furthermore, many patients experienced these symptoms for years before being formally diagnosed. The perceptions of patients with a previous experience of public healthcare on the care they received within the public healthcare system were more positive towards their GE than their PCP. However, many patients with IBS feel that they are not listened to or are wasting their time seeing a HCP, especially in the case of primary care. Although the majority of patients were receiving pharmacological treatment, they perceived little or no improvement in their condition. The socio-labor consequences of IBS should be addressed. This is a priority that is not always given sufficient attention during consultations. Results from this study suggest that empathy via listening, openness in discussing symptoms and providing enough time for the consultation appear to be essential for the patient-HCP interaction and may relieve the stigma that patients often associate with their symptoms. Further understanding of IBS pathophysiology and stronger communication between patients and HCP may lead to improve diagnosis, treatment and management of IBS.