INTRODUCTION
Meckel's diverticulum is the most widespread congenital abnormality of the gastrointestinal system 1. The reported incidence is 0.6-4% in most studies and is known to develop from incomplete obliteration of the omphalomesenteric canal causing the creation of a true diverticulum in the small bowel 2. The first descriptions of this condition were recorded by Fabricus Heldanus in 1650 3 and subsequently by Levator and Ruysch in 1671 and 1730, respectively 4,5. However, the name was attributed to the German comparative anatomist Johann Friedrich Meckel, who established the embryonic origin in 1809 6.
Since Meckel's diverticula are usually clinically asymptomatic, particularly in adults, it may be encountered during a laparotomy performed for another reason. It may be less frequently found as an incidental finding on diagnostic imaging. Life-threatening complications, such as intestinal obstruction, bleeding, inflammation and perforation may also develop. While bleeding is life-threatening in childhood, intestinal obstruction is more common in adulthood. However, the diagnosis of Meckel's diverticulum is often overlooked. Therefore, the aim of this study was to contribute to the management strategies by conducting a review of the current literature, including the knowledge of the clinical and diagnostic features and the management of Meckel's diverticulum.
CLINICAL FEATURES
The cells covering the vitelline channel are pluripotent. Therefore, the vitelline channel contains heterotopic gastric tissue (50%), pancreatic tissue (5%) and more rarely, hepatobiliary tissue and duodenal, colonic, endometrial or Brunner glands. Life-threatening and disturbing complications such as gastrointestinal hemorrhage (31%), inflammation (25%), intestine obstruction (16%), hernial involvement (11%), intussusception (11%), fistula or umbilical sinus (4%) and tumors (2%) occur as a result of the presence of heterotopic tissues 7,8.
As the majority of diverticula maintain a silent course, diagnosis is often made incidentally during a small intestine contrast study, unrelated laparotomy or laparoscopy procedures, or when complications result from the diverticulum 9. Establishing a diagnosis of symptomatic Meckel diverticulum is difficult preoperatively. Although symptoms can appear at all ages, clinical manifestations are more widespread in childhood 10. Higaki et al. 11 examined 776 patients and concluded that diagnosis in cases that present with symptoms, with the exception of bleeding, was more difficult than in those with per-rectal bleeding. The symptoms of complicated diverticulum may resemble symptoms of various other intra-abdominal pathologies such as other causes of small intestine obstruction, inflammatory bowel disease, acute appendicitis or peptic ulcer disease. This may make a differential diagnosis difficult 12.
Table 1 Complications of Meckel's diverticulum: incidence, causes, presentation in child/adult and symptoms

The life-time risk of diverticulum complications including bleeding, obstruction and diverticulitis is approximately 4% to 6%; 40% of these complications are seen in children below the age of ten years 13 (Table 1). The most general presentation in childhood is bleeding, which has been reported in approximately 50% of cases with symptoms related to the diverticulum 10. The most widespread complication of Meckel's diverticulum in adults is bowel obstruction, whereas this presentation occurs as the second most common complication in childhood 9,10,14. Intestinal obstruction resulting from Meckel's diverticulum occurs via distinct mechanisms such as: intussusception 15, volvulus 9,16, abdominal wall hernia 9,17,18, Meckel's diverticulitis 9, entrapment of the bowel loop beneath the mesodiverticular band (9, 19) (Fig. 1), lithiasis of the diverticulum 9,20, an ileum loop entrapped by a band stretching between the Meckel's diverticulum and the base of the mesentery 9, phytobezoar formation, gallstone ileus, impacted meconium in neonates and tumors (carcinoids, mesenchymal tumors, lipomas, hamartomas and others) 9,21,22. The presentation of obstruction related to the diverticulum may resemble other sources of small intestine obstruction.

Fig. 1 Intra-operative view: obstruction resulted from trapping of the small intestine loop under the meso-diverticular band of Meckel's diverticulum.
The second most widespread complication in adults is related to the inflammatory process. The combined rate of diverticulitis and perforation is almost 20% and can often not be differentiated from acute appendicitis until observed via laparotomy 21. Acute inflammation of the Meckel's diverticulum is thought to be caused by obstruction of the diverticular opening as a result of an enterolith, inflammatory tissue, food, other parasites (Taenia saginata or Ascaris lumbricoides), tumors or a foreign body 23,24,25. Obstruction leads to bacterial overgrowth and an inflammation similar to acute appendicitis 26. Meckel's diverticulitis can also result from torsion of the diverticulum or peptic ulceration due to heterotopic gastric tissue. If not treated, it generally results in perforation and peritonitis 9.
DIAGNOSIS
Despite all the improvements, the most significant challenge is still the preoperative diagnosis of Meckel's diverticulum 2. The diverticulum is occasionally identified incidentally on imaging studies and may be found during the course of a laparotomy performed for other reasons. The preferred diagnostic method is laparoscopy in doubtful cases. However, laparoscopy is not an initial step of diagnostic modalities as it is more invasive compared to conventional imaging methods 10.
Radiological imaging
Plain X-ray, barium studies and computed tomography (CT) scans are seldom beneficial for a preoperative diagnosis of the diverticulum. The typical appearance of an intestinal obstruction may be demonstrated by plain abdominal radiographs. When distension develops in a diverticulum, diagnosis may be established due to a gas-filled viscous appearance in the right iliac fossa or middle abdomen region. If a perforation develops as a complication, the findings of pneumoperitoneum may be seen on upright chest and plain abdominal radiographs. Characteristically, the diverticulum is delineated as a contrast-filled out pouching which has a junctional fold pattern and is seated on the anti-mesenteric margin of the small bowel 10.
Ultrasonography, although not specific enough for imaging this condition, may reveal a tubular diverticulum swollen with fluid in a region away from the cecum, invagination, segmental thickening of the bowel walls, swelling of diverticular wall and pelvic abscess 27. Anomalous vessels may be detected via Doppler ultrasonography 28. On CT scan, differentiation of the Meckel's diverticulum from the normal small intestine is difficult in uncomplicated patients. However, CT may reveal a gas-filled structures or blind-ending fluid in continuity with the small intestine 29. With regard to uncomplicated patients such as those with intussusception, CT imaging can be applied and the inverted diverticulum is typically demostrated as an interior nucleus of fat attenuation which is encircled by an annulus of soft tissue attenuation 30. In cases where a lesion in the small intestine is suspected, the alternative radiological examination to conventional tomography is CT enteroclysis 31.
Angiography
The diagnosis of a bleeding diverticulum can usually be made via a Meckel's scan or mesenteric arteriography 32. Angiograms of the arteria mesenterica superior may not only display the location of the hemorrhage by extravasation of focal radiopaque substance but also the reason for the hemorrhage. The accuracy rate of angiography is 59% 10. Active signs of hemorrhage can be identifed on high-resolution CT angiography. With regard to the detection of active gastrointestinal hemorrhage, CT angiography was shown to have a specificity of 92% and sensitivity of 85% in a meta-analysis of 22 studies that included 672 cases 33. Although another study of 124 patients reported a CT angiography accuracy rate of 100% 34, the type of patients and the context should be taken into consideration when evaluating the accuracy of CT angiography.
Nuclear imaging
Technetium-99m pertechnetate scanning, a diagnostic tool for Meckel's diverticulum, is the most commonly used non-invasive technique for diagnosis. Furthermore, patients with gastrointestinal bleeding do not require general anaesthesia. This is a useful method due to its tendency to concentrate on ectopic gastric tissue 2. The reported specificity is 95%, with a sensitivity of 80%-90% and an accuracy of 90% in children 35, whereas specificity is 9%, sensitivity 62.5% and accuracy 46% in adults. Thus, it is less reliable in adults 36. However, both false-negative and false-positive scan results may occur due to technical problems or the bladder overlapping the region of the diverticulum 10. Pre-treatment with pentagastrin, which accelerates Tc uptake or H-2-receptor antagonists and reduces Tc release by the gastric mucosa, decreases the rate of false-negative results 37).
Although the above-mentioned diagnostic tools have been widely used for the diagnosis of Meckel's diverticulum for many years, new diagnostic methods such as capsule endoscopy, double-balloon enteroscopy and magnetic resonance (MR) enterography have emerged in recent years. After the emergence of both capsule endoscopy and double-baloon enteroscopy, the diagnosis of small intestine diseases has dramatically developed over the past decade.
The whole small intestine can be endoscopically reached by both capsule endoscopy and double-baloon enteroscopy 38.
Capsule endoscopy and double-balloon enteroscopy
Capsule endoscopy is a novel technological tool for the examination of the small bowel in a noninvasive and simple manner. It has been proved in a number of studies that capsule endoscopy has the capability to detect small intestine lesions in cases with obscure gastrointestinal hemorrhage. The entire small intestine can be examinated by both double-baloon enteroscopy and capsule endoscopy. For the detection of hemorrhagic lesions in the small bowel, other studies proved that the efficacy of both capsule endoscopy and double-baloon enteroscopy is similar. However, capsule endoscopy is contra-indicated and also difficult in cases under ten years of age. Furthermore, it is relatively simple to reach via the retrograde double-balloon enteroscopy method, as the distance of the Meckel's diverticulum is generally closer than a meter from the ileocecal valve. During capsule endoscopy, the capsule may pass rapidly through the opening of the Meckel's diverticulum and an image may not be obtained. The management of cases with an obscure gastrointestinal hemorrhage results in a consumption of resources and time. Research has demostrated that initial double-balloon enteroscopy (compared with push enteroscopy, angiography, intra-operative enteroscopy and capsule endoscopy) is the most cost-effective method for cases with small intestine hemorrhage 38.
Gasbarrini et al. 39 first defined the use of double-balloon enteroscopy for the detection of Meckel's diverticulum. The various clinical studies noted that double-balloon enteroscopy is a reliable method for the study of small bowel pathology. The entire small intestine can be visualized and treated and biopsies can also be performed using this procedure 38. Konomatsu et al. 40 used double-balloon enteroscopy for both diagnosis and treatment of bleeding Meckel's diverticulum. The most widespread indication for double balloon enteroscopy is obscure gastrointestinal hemorrhage. The detection ratio of obscure hemorrhage using this techenique is 68.1%. However, due to the potential adverse events, limitations and own unique set of indications, experience is limited in children. Double-balloon enteroscopy intervention may lead to complications such as pancreatitis, pneumonia, bowel obstruction and perforation. Acute pancreatitis, which occurs after 0.3% of interventions, is a source of concern. However, this is not an issue for those cases undergoing retrograde double-baloon enteroscopy, as in cases undergoing the procedure for the detection of Meckel's diverticulum. Most studies have shown that double balloon enteroscopy performed in childhood is a reliable and safe method 38. In the Leung's study 41, retrograde double-balloon enteroscopy was recommended for children over 14 kg.
CT enterography and MR enterography
CT enterography not only maximizes the visibility of the bowel structure and mucosa with the support of radiopaque substances but also detects peri-enteral abnormalities. For this reason, it has been proven to be more benifical than conventional CT for the detection of lesions in the small intestine. MR enterography, which allows the assessment of bowel functionalities using MR fluoroscopy, is a novel technique without radiation. It unites the advantages of both the morphological imaging of MR and the conventional enterography. In this way, it can analyze both the morphology and function of the small bowel. Its perfect soft tissue contrast and three-dimensional imaging capability means that changes around the intestinal canal and the mucosa can be examined 42.
Diagnostic laparoscopy or laparotomy
Laparoscopy is an efficient and safe way of localizing the lesion for the removal of the Meckel's diverticulum. However, it is more invasive and therefore not recommended as an initial step for diagnosis 10.
MANAGEMENT
As double-balloon enteroscopy can be used for therapeutic interventions such as argon plasma coagulation, balloon dilatation, polypectomy and performing biopsies, some clinicians use it effectively for the endoscopic treatment of bleeding Meckel's diverticula 43. Double-ballon enteroscopy has also been used for endoscopic full-thickness resection of inverted Meckel's diverticulum 40,44).
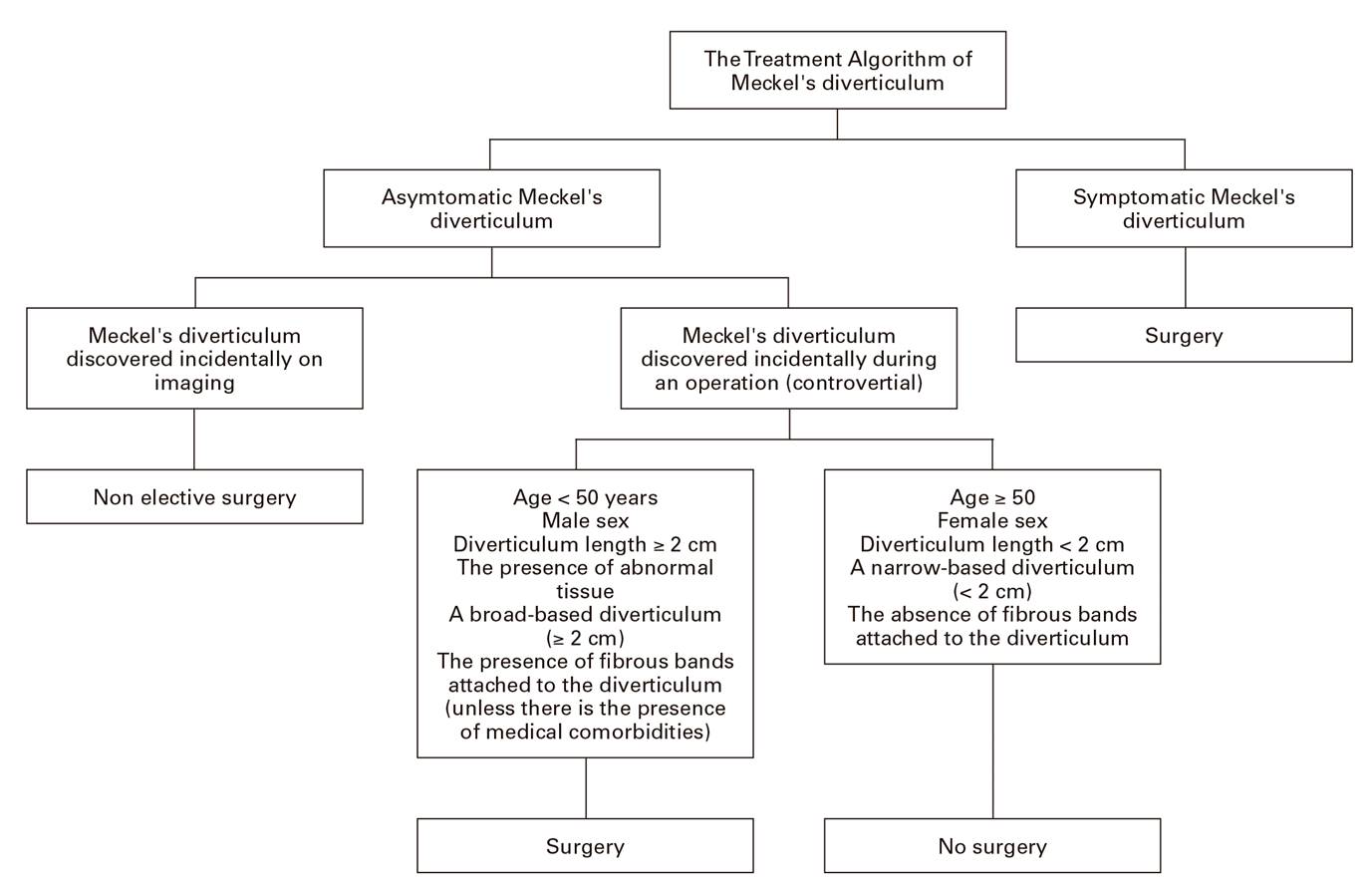
Although endoscopic therapeutic procedures have been used recently, the main treatment for Meckel's diverticulum is surgical resection. However, whether resection should be applied to all incidentally detected Meckel's diverticula or not is still controversial. Elective surgery is not recommended for cases where the diverticulum is discovered incidentally on radiological imaging. In general, it is not possible to determine the increased risk of complications associated with incidentally detected Meckel's diverticulum by intraoperative palpation or inspection 2. Therefore, for this reason, the intraoperative approach to asymptomatic or incidentally encountered Meckel's diverticulum remains a matter of debate. Many surgeons advocate resection of an incidentally encountered diverticulum due to the potential for life-threatening complications that may develop 45. The clinical circumstances of the case, the life-long risk of complications and anatomic characteristics associated with symptoms should be taken into account when asymptomatic diverticula are encountered during an abdominal exploration 15,46. Some surgeons use a risk score as a guide to make a decision of the need for a resection. Robijn et al. 46 recommend a scoring system based on the four risk factors for decision-making using weighted criteria and a more objective basis; these include: patient age < 45 years, male gender, fibrous band presence and diverticula > 2 cm long. When the risk score is ≥ 6 points, the resection of asymptomatic Meckel's diverticula is recomended.
Based on the data of the relevant literature, all incidentally detected diverticula that meet any of the following criteria should be removed.
Patient age < 50 years 47.
Male gender 47.
Length of the diverticulum > 2 cm 47.
Presence of abnormal tissue on histopathological examination 47.
A broad-based diverticulum, which has been shown in other studies to be prone to complications 46.
The presence of fibrous bands attached to the diverticulum may also be significat 46.
Symptomatic Meckel's diverticula should be managed surgically by laparotomy, laparoscopy or laparoscopy-assisted approaches 19. Generally, a wedge resection is performed of the diverticulum and sometimes an end-to-end anastomosis is applied following the resection of an ileum segment. The extent of resection is determined according to the intraoperative findings and any intraoperative complications. If the omphalomesenteric remnant is narrow-based and there is no palpable mass within the lumen of the ileum, this diverticulum may be managed by a simple wedge resection, followed by a primary closure of the remaining defect 9,48. If the diverticulum base is broad, heterotopic tissue is palpated or there are ischemic or inflammatory alterations in the ileum adjoining the diverticulum, resection of the associated intestine and end-to-end anastomosis should be applied. A segmental ileal resection must be performed in cases of gastrointestinal bleeding, as the hemorrhage is generally located in the adjoining ileum. Depending on the size and location of benign tumors within the diverticulum, simple diverticulectomy is sufficient, whereas malignant tumors require wide resection of the intestine and mesentery 45.
The treatment algorithm created by the authors of this review for Meckel's diverticula is shown in Figure 2.
CONCLUSION
Meckel's diverticulum, which contains all the layers of the small intestine, is the most commonly seen congenital abnormality of the gastrointestinal tract. Although present in only a small percentage of the general population, the complications of this disorder can be severe. These include intestinal obstruction, hemorrhage, intussusception, diverticulitis and perforation causing peritonitis. It can be difficult to diagnose a complicated Meckel's diverticulum preoperatively as the radiological and clinical findings can resemble features of other acute abdominal disorders. A good level of knowledge of the clinical, embryological, radiological and pathological features of Meckel's diverticulum will enable a rapid and proper diagnosis of patients, thereby allowing treatment via a timely surgical intervention.