Dear Editor,
This letter reports an unusual case of a giant inflammatory fibrous polyp (IFP) that originated from the submucosa of the gastric antrum.
Case report
A 64-year-old female presented with symptoms of progressive abdominal pain, nausea and vomiting. No specific past or family history was identified and the vital signs and laboratory analysis were normal. Physical examination revealed mild epigastric tenderness on deep palpation. The ultrasonography showed two hypoechoic masses linked together, mainly located in the gastric antrum. Abdominal computed tomography identified two low-density masses without extramural extension. Esophagogastroduodenoscopy showed two protuberant semi-pedunculated polyps connected at the base and joined as one giant polyp. The lesion measured nearly 8 cm, with a local irregular ulcer (Fig. 1A). There was a mixed echogenicity on EUS (Fig. 1B). Eventually, the patient underwent a successful surgery due to the non-specific findings and endoscopic biopsy results. The entire mass measured 10.0 × 6.0 × 5.0 cm (Fig. 1C). The definite diagnosis of IFPs was confirmed by a postoperative histopathologic evaluation of an onion-skin appearance (Fig. 1D) and immunohistochemistry (only CD34 was positive and CD117, DOG1, SMA, desmin and S-100 were negative). The patient had an uneventful recovery and was subsequently discharged on the 7th postoperative day.
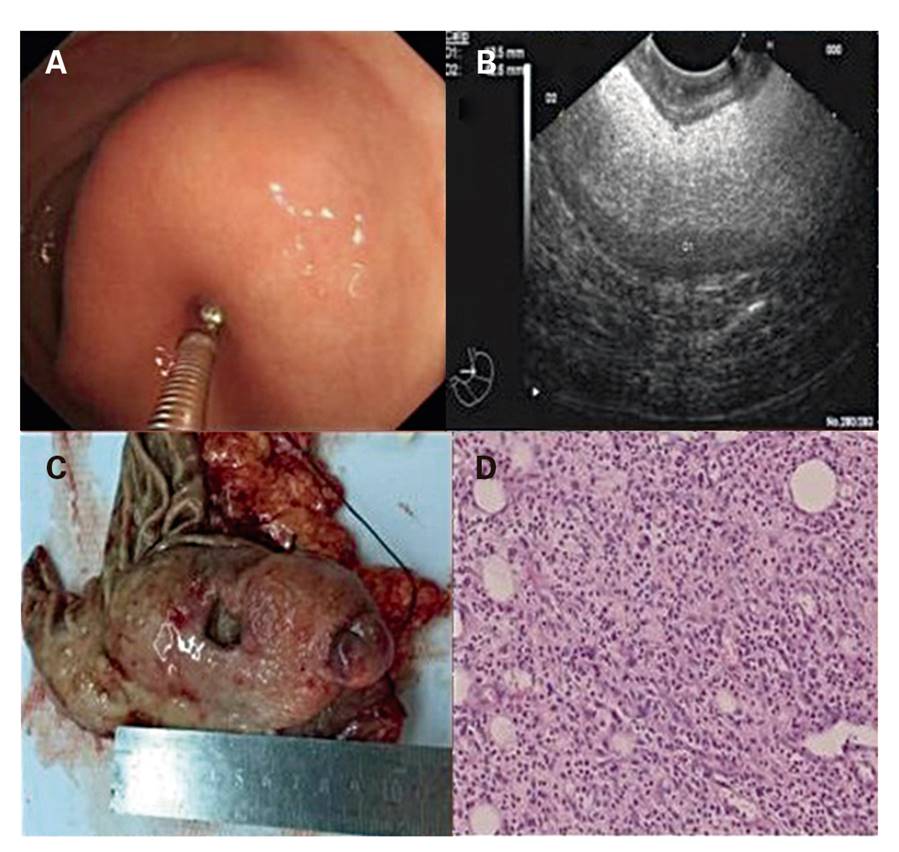
Fig. 1 A. The local part of the giant polyp in the gastric antrum under endoscopy led to the gastric outlet obstruction. B. EUS showed hypoecho and hyperecho with an indistinct margin in the third sonographic layer that was not completely separated from the fourth sonographic layer. C. The gross resected specimen was giant. D. The histopathological onion skin appearance presents a mixture of fibroblasts, proliferating blood vessels and inflammatory cells such as eosinophils (hematoxylin and eosin-staining, 200×).
Discussion
Consistent with the findings reported by Silva et al., IFPs have the following features 1,2: a) IFPs are frequently benign with a size range between 1-5 cm, larger lesions sometimes imitate malignancy 3; b) the lesion usually originates in the submucosa; c) clinical manifestations and examinations are asymptomatic; d) final diagnosis may only be confirmed by postoperative histology and immunohistochemistry 4; and e) therapy options usually include endoscopic treatment and surgical excision, depending on the size and location of the lesion 3). The pathogenesis remains unknown, including genetic, biological and other factors 3,5, which requires further exploration.
We present this case to remind doctors with more experience of IFPs, in order to avoid patients suffering excessive pain and costs.














