Dear Editor,
We present the case of a 65-year-old male with a history of type 2 diabetes mellitus and poorly controlled hypertension. He was admitted due to endocarditis on the native aortic valve with an abscess and biventricular dysfunction. When the patient was admitted to the Emergency Room, he had a cardiorespiratory arrest which required the implantation of an urgent aortic prosthesis. During hospital admission, he had a persistent pain in the right hypochondrium accompanied by nausea. Tests showed a pattern of incomplete cholestasis (FA 825 U/l, GGT 1987 U/l), associated with a moderate elevation of the tumor marker CA 19.9 (293 U/l). Magnetic resonance cholangiopancreatography identified a 10 mm ductus dilatation with abrupt termination. The presence of a cholangiocarcinoma was suspected.
During the following 24 hours, the patient suffered hematemesis and rectal bleeding with secondary hemorrhagic shock that required vasoactive drugs and the transfusion of blood products. An urgent upper digestive endoscopy identified an elongated blood clot originating from the papilla. Angio-CT identified a pseudoaneurysm rupture of a segmental branch from the right hepatic artery (segment V). An urgent arteriography was performed in order to embolize the injury. The bleeding was controlled (Fig. 1) and there were no further complications.
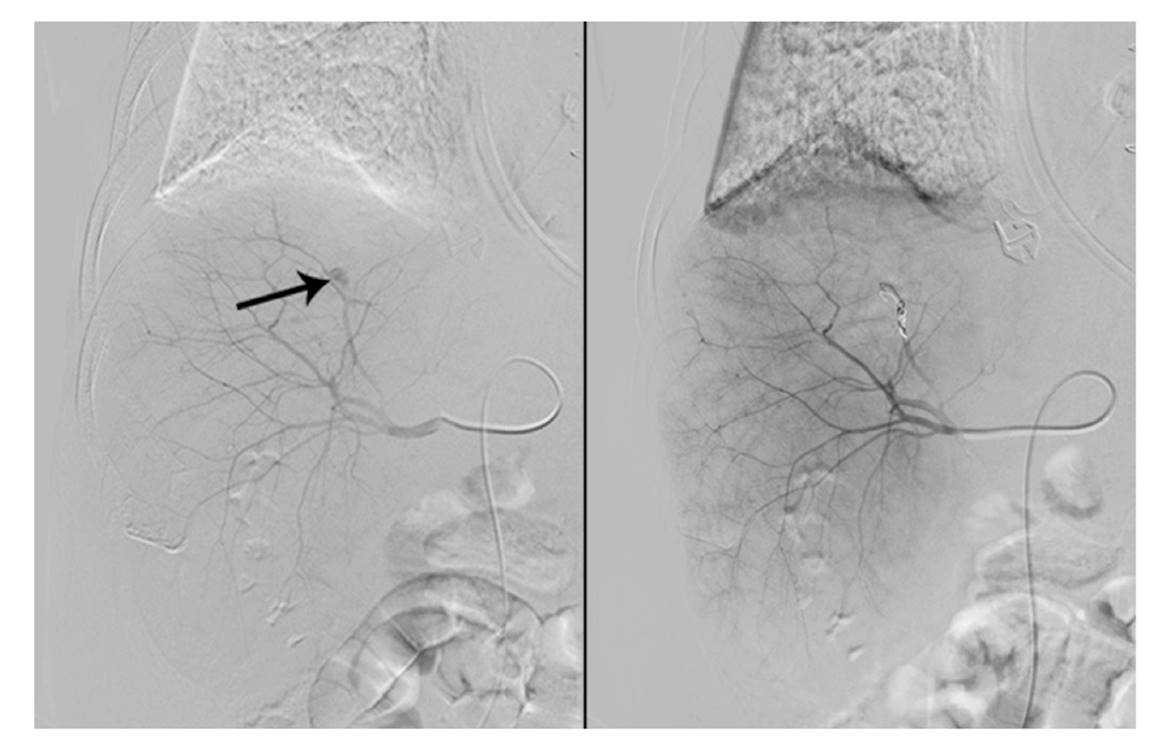
Fig. 1 A pseudoaneurysm rupture of the segmental branch of the right hepatic artery is shown that results in its embolization.
Discussion
A pseudoaneurysm of the hepatic artery is an uncommon cause of upper gastrointestinal bleeding. This represents 15 to 20% of the total number visceral aneurysms. However, pseudoaneurysms have the highest percentage of rupture, up to 80% 1,2. Although pseudoaneurysms usually occur asymptomatically, they may present as a hemorrhage, abdominal pain or jaundice. The main causes are traumatic and iatrogenic, although spontaneous forms have also been described in the context of infectious or inflammatory processes. A diagnosis is made via imaging tests and the gold standard is arteriography. Selective embolization may also be offered as a treatment option 3.














