Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 no.6 Madrid nov./dic. 2007
PÁGINA DEL RESIDENTE
What should the diagnosis and treatment be?
¿Cuál sería su diagnóstico y su manejo terapéutico?
Female, 34 years old with no medical history of interest, attended the emergency department complaining of an eyelid edema and slight discomfort in the left eye.
The examination revealed slight left-sided proptosis, but no other pathologic signs. The patient was sent to the outpatient section of the department of Oral and Maxillofacial Surgery of our hospital for monitoring.
Four hours later, she was brought into the Emergency Department on a trolley with greater proptosis, pain and diplopia after vomiting. Examination revealed proptosis of the left eye with a stony consistency, edema of both lids, complete ophthalmoplegia, Marcus- Gunn pupil and an intraocular pressure (IOP) of > 70 mmHg. The back of the eye had a spontaneous pulse and the temporal artery was dilated (Fig. 1).
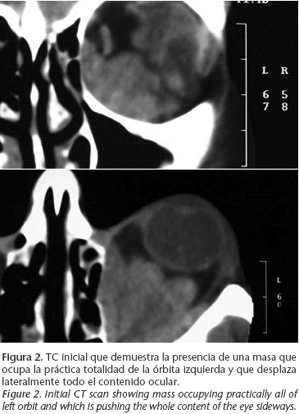
A CT scan was urgently requested (Fig. 2).
PÁGINA DEL RESIDENTE
Acute thrombosis of an orbital varix. A case report
Trombosis aguda de variz orbitaria. A propósito de un caso
G. Gómez Oliveira1, F. Lorenzo Franco2, G. Rodríguez3, J.L. López Cedrún4, Á. Martínez5
1 Médico Residente. Servicio de Cirugía Oral y Maxilofacial.
2 Médico Adjunto. Servicio de Cirugía Oral y Maxilofacial.
3 Médico Adjunto . Servicio de Oftalmología.
4 Jefe de Servicio de Cirugía Oral y Maxilofacial.
5 Jefe de Servicio de Neurorradiología.
CHU Juan Canalejo. La Coruña, España.
With the diagnosis of acute thrombosis of the orbital varix and given the high risk of blindness of the patient, urgent orbital decompression was decided on. Under general anesthesia and using a subciliary approach, resection of the left orbital floor was carried out with preservation of the infraorbital nerve in order to reduce the intraorbital pressure (Fig. 3). After the surgery, ocular mobility, the back of the eye, IOP and the pupils returned to normal (Fig. 4).
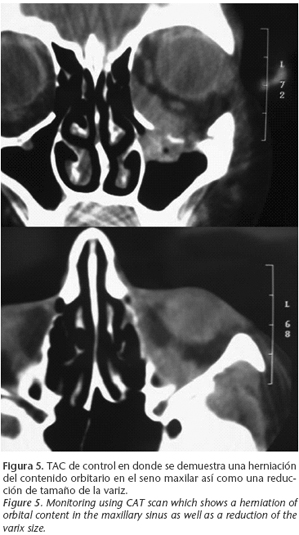
After 24 hours a CT scan was carried out in addition to MRI in order to evaluate the outcome (Figs. 5 and 6).
The case was discussed with the Department of Neuroradiology and it was decided that an arteriography should be carried out in order to diagnose the exact origin of the varix and to possibly carry out definitive treatment. No relevant vascular disturbance was observed.
Ten months after the surgery the patient has shown no symptoms related with the pathology.
Discussion
Orbital varices are uncommon intraorbital masses. They are considered congenital venous malformations.1-3,5 They are made up of anomalous venous vessels with low flow and low pressure that are directly communicated with the systemic venous system.2,3,5 They may be made up of a single venous vessel or by a plexus.8 They commonly manifest as a unilateral mass although in the literature bilateral cases have been described.6,9,11,12
They more commonly affect young people and there are no differences with regard to sex.5,8,9,11,12
They can be primary (congenital) or secondary to orbital trauma or to considerable hemodynamic changes.8,12
They tend to be located in the anteromedial portion of the orbit and the most common origin is the superior ophthalmic vein although any venous segment of the orbit can be involved.9,11 On rare occasions they may appear in the conjunctiva, sclera or lid.11
Clinically they appear as acute, transitory proptosis sometimes accompanied by diplopia, induced by changes in intra-orbital pressure such as Valsalva maneuvers, supine position, cough or vomiting, that disappear with rest.2-5,9 Sometimes these clinical symptoms are absent and they appear only as a progressive edema or an eyelid mass.11
Occasionally varices can suffer thrombosis and hemorrhaging, and they may even lead to an orbital compartmental syndrome with intense pain, loss of visual acuity, nauseas and vomiting, although fortunately these are very uncommon.1-3,8,9,11
The diagnosis is based on clinical and radiological findings that include CT, MRI, Echo–Doppler and arteriography. There are authors that are of the opinion that the changes in the radiological findings before and after carrying out a Valsalva maneuver or jugular compression, are diagnostic of orbital varix.5,9,11
A high-resolution CT scan with contrast provides an excellent view of varices as well as any possible phleboliths on the inside, which are considered by many authors as diagnostic.1-3,5,11,12
MRI provides greater definition with regard to soft tissue despite its limitations: low bone resolution, artifacts with patient movement and lengthy procedure.4,5,9,11,12
Echo-Doppler shows a typical blood flow image when carried out during Valsalva maneuvers. Initially the flow can be seen to stop and a reverse flow follows.5 This is useful for differentiating vascular lesions from non-vascular lesions, and also it will demonstrate the quantity of the existing flow, the anatomic location, and it will be useful for long-term monitoring.5,9,10 The pathologic anatomy will confirm the diagnosis if necessary.1,6,9,11
There is no consensus in the literature as to which is the more suitable therapeutic option, although it is clear that the treatment should be as conservative as possible. 2-5,7,9,11 The therapeutic options available include surgery, embolization, sclerosing agents and electrothrombosis.8
Surgery includes urgent orbital decompression and excision of the varix. The approach varies depending on the location of the varix. Thus, for medial lesions an anterior or lateral orbitotomy can be carried out, or an upper blepharoplasty.11 For anterior or inferior lesions a lower lid approach and anterior orbitotomy can be carried out,7,9 and for lateral lesions a lateral canthotomy can be used.9
However, the surgery is technically complicated8,1 and there is a high risk of blindness due to hemorrhaging or damage to the optic nerve or to the ophthalmic artery.3,8,11 Therefore, it is just used in specific cases when there are repetitive symptomatic episodes or unresolved thrombosis,2 functional defects,3,7-9 untreatable pain,7-9,11 aesthetic reasons,2,3,7,8,11 compression of the optic nerve,8 displacement of the eyeball, 2,9,11 hemorrhaging with risk of blindness and as a method of diagnosis.11 However Wright et al.,11 in a review of 158 patients, used surgery in 58% of the cases. Electrothrombosis and the injection of sclerosing agents tend to be performed in combination with other techniques, and they are rarely used on their own.8 Endovascular embolization can be carried out by means of percutaneous femoral catheterization and the results are good.13 However, there are authors who prefer direct catheterization of the varix within the orbit after surgical exposure.8 This technique is the most useful in cases of sac or segmental types of varices as opposed to those that are made up of a venous plexus.8 This is contraindicated in cases of thrombosis or active hemorrhaging.8,13
Conclusión
Orbital varix is a very rare entity and its treatment is somewhat unclear. Complications are unusual although when these appear the patients vision can be at risk, and diagnosis and treatment will be urgently needed.
![]() Correspondence:
Correspondence:
Dr. Guillermo Gómez Oliveira
c/ Almirante Mourelle 29 2º
15011 La Coruña, España.
Email: guis@canalejo.org
References
1. Menon SV, Shome D, Mahesh L, Subramanian N, Krishnakumar S, Biswas J, y cols. Thrombosed orbital varix - a correlation between imaging studies and histopathology. Orbit 2004;23:13-8. [ Links ]
2. Islam N, Mireskandari K, Rose GE. Orbital varices and orbital wall defects. Br J Ophthalmol 2004;88:1092-3. [ Links ]
3. Islam N, Mireskandari K, Burton BJ, Rose GE. Orbital varices, cranial defects and encephaloceles: and unrecognized association. Ophthalmology 2004;111:1244-7. [ Links ]
4. Guigon - Souquet B, Grubian - Netter S, Macarez R, Giordano P, Bazin S. Uncomplicated orbital varix: a difficult therapeutic problem. J Fr Ophthalmol 2002; 25:840-2. [ Links ]
5. Secil M, Soylev M, Ada E, Saatci AO. Orbital varices: imaging findings and the role of color doppler sonography in the diagnosis. Comput Med Imaging Graph 2001;25:243-7. [ Links ]
6. Yazici B, Yazici Z, Gelisken O. An unusual case: bilateral orbital varices. Acta Ophthalmol Scand 1999;7:453-5. [ Links ]
7. Kim JW, Stewart WB, Spencer WH, Ellis DS. Accute expansion of an orbital vascular malformation. Arch Ophthalmol 1999;117:844-5. [ Links ]
8. Weill A, Cognard C, Castaings L, Robert G, Moret J. Embolization of an orbital varix after surgical exposure. AJNR Am J Neuroradiol 1998;1:921-3. [ Links ]
9. Rubin PA, Remulla HD. Orbital venous anomalies demonstrated by spiral computed tomography. Ophthalmology 1997;104:1463-70. [ Links ]
10. Kawaguchi S, Nakase H, Noguchi H, Yonezawa T, Morimoto T, Sakaki T. Orbital varix diagnosed by color doppler flow imaging - case report. Neurol Med Chir (Tokyo) 1997;37:616-9. [ Links ]
11. Wright JE, Sullivan TJ, Garner A, Wulc AE, Moseley IF. Orbital venous anomalies. Ophthalmology 1997;104:905-13. [ Links ]
12. Cohen JA, Char DH, Norman D. Bilateral orbital varices associated with habitual bending. Arch Ophthalmol 1995;113:1360-2. [ Links ]
13. Takechi A, Uozumi T, Kiya K. Embolization of orbital varix. Neuroradiology 1994;36: 487-9. [ Links ]











 texto en
texto en