Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.4 Madrid jul./ago. 2009
Clinical analysis of our experience in over 100 cases of maxillary sinus lift
Elevación de seno maxilar. Análisis clínico de nuestra experiencia en más de 100 casos*
Gui-Youn Cho-Lee1, L. Naval-Gías2, M. Mancha de la Plata1, J. Sastre-Pérez2, A.L. Capote-Moreno2, M.F. Muñoz-Guerra2,F.J. Rodríguez-Campo2
1 Médico Residente
2 Médico Adjunto
Servicio de Cirugía Oral y Maxilofacial.
Hospital Universitario de La Princesa. Universidad Autónoma. Madrid. España.
* Este artículo refleja los resultados comunicados en el Congreso de Cirugía Oral e Implantología de la Sociedad Española de Cirugía Oral y Maxilofacial que se celebró el pasado mes de mayo en Santiago de Compostela, y que obtuvo el Primer Premio a la mejor Comunicación Oral.
ABSTRACT
Purpose: Maxillary sinus elevation surgery is one of the most versatile surgical procedures in maxillofacial surgery: there are various approaches to the sinus, different materials for sinus grafting, other preprosthetic procedures can be associated and the implants placement can be simultaneous or delayed, depending on the initial bone height. The aim of this study was to demonstrate this versatility by means of reporting the clinical outcome of sinus augmentation surgery in 131 cases.
Materials and Methods: 131 sinus augmentation procedures were undertaken on 91 consecutive patients (mean age 50,43 years (26-69)). The preoperative and postoperative radiological study was developed by means of orthopantomography and Dental-TC. The survival rate of implants, as measured by integration and succesfull loading, was compared between different graft materials, smoking/non-smoking patients, different groups of associated pathologies and simultaneous/delayed implants placement. The time (months) necessary for prosthesis loading was measured and compared between the different graft material groups.
Results: 228 screw-type implants were placed in sinus lifted regions. The mean residual ridge height was 6,59±2,11 mm. The mean postsurgical ridge height was 14,57±2,33 mm. After a mean follow-up period of 2,94 years (range 1 to 12 years) the global implant survival rate was 96,91%. There were not significant differences between different bone grafts, associated comorbidity and smoking habits.
Conclusions: On the basis of this retrospective study, it might be concluded that the sinus augmentation surgery is a very versatile procedure. Its efficacy and predictability in terms of implant survival rate is extremely high and independent on the bone graft material, surgical technique, associated morbility, smoking habit and immediate/delayed implant placement. The use of autologous bone requires less time to load the prosthesis.
Key words: Sinus augmentation; Technical versatility; Bone grafts; Simultaneous/delayed implant placement; Implant survival rate.
RESUMEN
Objetivos: La elevación de seno maxilar es uno de los procedimientos más versátiles en cirugía oral, de modo que hay descritos diversos abordajes, tipos de injertos, posibilidad de asociar otras técnicas preprotésicas y colocar implantes de manera simultánea o diferida, dependiendo de la altura ósea inicial. Nuestro propósito es comunicar nuestra experiencia después de intervenir 131 casos.
Materiales y métodos: Se analizó una serie de 131 procedimientos llevados a cabo en 91 pacientes consecutivos, entre 1996 y 2007. La edad media fue de 50,43 años (23-69). El control radiológico pre y postoperatorio se realizó mediante ortopantomografía y TC dental. Se analizó la tasa de éxito implantario (implantes osteointegrados y cargados) comparando los distintos injertos, el hábito tabáquico, las patologías asociadas y la colocación simultánea o diferida de los implantes. Así mismo, el tiempo (meses) necesario para cargar la prótesis se ha comparado entre los diferentes tipos de injerto.
Resultados: En las zonas aumentadas se colocaron un total de 228 implantes roscados. La altura preoperatoria media del suelo del seno fue de 6,59±2,11 mm y la postoperatoria de 14,57±2,33 mm. El seguimiento medio fue de 2,94 años (1-12). La tasa de éxito implantario global fue de 96,91%, no habiéndose encontrado diferencias significativas entre los distintos injertos, patologías asociadas o el hábito tabáquico.
Conclusiones: En base a este análisis retrospectivo, se concluye que la elevación de seno es una técnica versátil, eficaz, segura y predecible; con una tasa de éxito implantario muy alta independiente del tipo de injerto, comorbilidad, hábito tabáquico y colocación simultánea o diferida de los implantes. El empleo de injerto óseo autólogo requiere un tiempo de espera para la carga protésica significativamente menor.
Palabras clave: Elevación de seno; Injertos óseos; Colocación simultánea/ diferida de los implantes; Tasa de éxito implantario.
Introduction
Implant rehabilitation of the posterior atrophic maxilla is a challenge for a maxillofacial surgeon. The ridge height of the posterior maxilla can become compromised because of increased pneumatization of the sinus or because of precipitated alveolar bone reabsorbing that accelerates after dental extraction, trauma or a concomitant pathology of the region. Furthermore, posterior maxilla bone density is usually poor.1,2 A ridge height of 10 mm is needed so that the implants placed are successful and predictable.3 In cases of atrophy, the maxilla sinus lift is an excellent therapeutic option. This technique increases the ridge height of the posterior sector of the maxilla via the interposition of different types of bone grafts between the Schneider membrane and the remaining alveolar bone. This allows for the placement of bone integrated implants in the region. This procedure was described by Tatum in 1976 and then later published by Boyne and James in 1980. Currently sinus lift is one of the most common preprosthetic surgical techniques used in maxillofacial surgery. It is also considered one of the most versatile techniques in preprosthetic surgery.6 Thus, the following have been described: many different approaches (lateral antrostomy or Caldwell-Luc and crest approach); instruments that can be used to perform lateral antrostomy (diamond o tungsten drills, piezoelectric scalpel and bone scapers);1,8,9 various types of bone grafts (autologous, allografts, xenografts, synthetic materials and a combination of these);10-20 or the possibility of not using any graft for example association or other techniques (onlay graft apposition, split osteotomy) and their execution once or twice (simultaneous or delayed implant placement) depending on initial ridge height.21,22,25
The purpose of this clinical study is to present a retrospective analysis of the 131 procedures that were carried out in our sample and show the relationship between the different parameters that affect implant success rate.
Material and method
This series is based on 131 maxilla sinus lifts performed between 1996 and 2007 on 91 consecutive patients in the Oral and Maxillofacial Surgery Service at the University Hospital of the Princess, Madrid Spain. The average patient age was 50.53 years (from 23-69). According to the Cawood and Howell scale 26, all of the patients had posterior maxilla atrophy grade.4-5 Various information was gathered before surgery: tobacco habit, periodontal disease (clinically diagnosed), prior cases of oral carcinoma and systematic illnesses. This procedure was advised against only in patients with active sinusitis and treatment with bisphosfonates. Pre and post operative radiological control were taken using an orthopantomogram and dental CT. Prosthetic rehabilitation was performed using fixed implant supported prosthesis or implant supported prosthesis.
Surgical protocol of sinus lift
The antibiotic Prophylaxis was used in all patients and was established for all patients consisting of an 875mg dose of amoxicillin clavulanic acid (1 pill every 8 hours) starting the day before surgery and continuing 7 days after surgery. Patients who are allergic to penicillin were given 300 mg of clindamycin (1 pill every 8 hours) for the same amount of time. 76.2% of the procedures were carried out under general anesthetic while 23.8% of patients received the local anesthetic articaine and adrenaline 1% (1:100,000).
Surgical technique of sinus lift has been described in various studies. The approach used in all of the cases we study is lateral anthrostomy or Caldwell-Luc. The procedure is only carried out in the anterior sector in order to avoid suture openings. A window is created in the buccal bone using drills, a piezosurgery® scalpel and bone scrapers (Zimmer Dental Iberica®), always under irrigation with saline solution. The sinus membrane is carefully detached using membrane elevators and later the graft is placed between the membrane and the remaining alveolar bone crest.
The grafts placed included intraoral autologous bone (maxilla tuberosity, lateral wall of the maxilla sinus), extra oral autologous bone (anterior and posterior iliac crests, calvarium) and a mix of autologous bone and inorganic bovine bone (Bio-oss®). In cases that needed more bone width, other procedures were incorporated like the apposition of "onlay" bone grafts and "split"osteotomy. Placement of implants is carried out simultaneously when the initial ridge height was at least 5 mm. A total of 228 screw-type implants(Mozo- Grau, Valladolid, Spain) were placed in the elevated zones. All of the patients were evaluated 1 week after intervention and then monthly. Waiting time for the placement of the prosthetic was at least 3 months.
Descriptive study and statistical analysis
The following parameters were evaluated for the descriptive study: bone height of the alveolar ridge before and after surgery (radio graphically verified using orthopantomogram and dental TC), smoking habit (smoker/non smoker) comorbidity (periodontal illness, systematic illnesses and prior oral carcinoma), type of anesthetic(local or general), type of bone graft (posterior/anterior iliac crest, maxilla tuberosity, lateral wall of the sinus, calvarium or inorganic bovine bone mixed with autologous bone), associated preprosthetic surgical procedures (apposition of onlay bone grafts, osteotomy split) placement of implants (simultaneous or delayed) and the type of prosthetic rehabilitation used (implant-mucosupported or fixed implant-supported prosthesis).
Implant success rate and wait time for setting of prosthetic (in months) were established as the dependent variables for our statistical analysis. The success rate was calculated for each sinus lift using the following formula (number of implants placed/number of implants lost)/ number of implants placed. The main variable that determined the other parameters is represented in the analysis using the implant success rate. The independent variables were: graft origin( posterior/anterior iliac crest, maxilla tuberosity, lateral wall of maxilla sinus , calvarium, mix of inorganic bovine bone and autologous bone), smoking habit (smoker/ nonsmoker) associated comorbidity (periodontal disease, systematic disease, prior oral carcinoma) and the placement of implants (simultaneous or delayed). Results of our analysis of the survival of implants were calculated as an average ± standard deviation for each independent variable. The time results (months) were calculated as a median and range (maximum and minimum values). Due to the asymmetric and heterogeneous distribution of the different variables in the sample, the different groups were evaluated using the Mann-Whitney non parametric test to compare the averages; the Kruskal-Wallis test and the Bonferroni correction to compare multiple averages. P < 0.05 values were considered statistically significant. Statistical analysis was carried out using the SPSS 15.0 program.
Results
Descriptive study of the sample
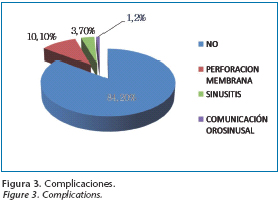
The average preoperative height from sinus floor was 6.59 ± 2.11mm and the postoperative height was 14.57± 2.33 mm. 71.4% of the sinus lifts were performed on healthy patients, while 11.3 % were performed on patients with varying systematic illnesses; 10.5% had periodontal disease and 5.3% had prior oral carcinoma. 70.21% of procedures were carried out on patients who were non smokers and 29.78% of them on smokers. The bone graft was taken from the lateral sinus wall using scrapers in 15% of cases, from calota in 14% of the cases, from the anterior iliac crest in 10.5% of cases, from the posterior iliac crest in 10.5% of cases, from the maxilla tuberosity in 2% and finally a mix of inorganic bovine bone and autologous bone in 48.9% of cases (Fig. 1) The apposition of the onlay bone grafts were incorporated in 41.66% of cases while osteotomy split was used simultaneously in 55.55% of cases (Fig. 2). The placement of implants was simultaneous in 64.7% of lifts and was delayed in 30.8% of cases with a wait time (in months) for implants setting of 4.33± 1.71 months. In 84.2% of cases there were no signs of complications. The most common complication was membrane tearing (10.1%) Other complications include: sinusitis (3.7%) and orosinusal communication (0.9%) (Fig.3). 95% of patients achieved complete implant rehabilitation (91.3% using fixed prosthesis implantsupported and 3.7% using prosthesis implant-mucosupported) the global implant success rate was 96.91%.
Statistical Analysis
Implant success rate
a) The average implant success rate was 100 % (ranging from 50% to 100%) for every type of graft (anterior and posterior iliac crest, calvarium, maxilla tuberosity, lateral wall of the maxilla sinus and inorganic bovine bone). Only 6 sinus lifts did not have a 100% success rate: 1 case using anterior iliac crest (50% rate), 2 cases using lateral wall of the maxilla sinus (66% and 75%) and 3 cases of inorganic bovine bone mixed with autologous bone (50% rate). There were no statistical differences found between the groups. b) There were no significant statistical differences found between the groups regarding tobacco habit and associated comorbidity. c) The average implant success rate for simultaneously placed implants was 98.65%± 7.57 and 93.57% ±16.43 for implants placed in a delayed way. This difference is statistically significant (P=0.046).
Wait time for setting of the prosthetic
The wait time (in months) for the prosthetic to set was compared according to the origin of the graft. (Fig. 4) The results were: anterior iliac crest:6.5 months (range 5.5-10.5); posterior iliac crest: 5.5 months (range 5.5-6.5); calvarium: 4.5 months (range 3.5-4.5); maxilla tuberosity: 4 months (range 3.5-4.5); lateral wall of the maxilla sinus: 4.5 months (range 3.5-4.5) and a mix of inorganic bovine bone and autologous bone: 7.5 months (range 5.5-12.5). The difference between the use of only autologous bone and the combination of autologous bone and inorganic bovine bone is significant (P<0.01) When comparing this variable according to the different origins of the autologous bone, there are statistically significant differences between the iliac crests and the autologous bone of other origins (calvarium, maxilla tuberosity and maxilla sinus wall) (P<0.01). Finally, there were no statistically significant differences between the calvarium bone, maxilla tuberosity and the lateral wall of the maxilla sinus.
Discussion
The placement of implants in premolar and molar areas in the upper maxilla can become difficult because of a lack of ridge height. Maxilla sinus lift surgery has proved to be a clinically predictable procedure that makes it possible to place implants in such cases.1,3-5,16 This study analyzes one of the "unicentric" series of the major sinus lifts published in the literature. Our series confirms that it is one of the most versatile preprosthetic surgeries. The results we gathered regarding the survival of implants has been excellent, with a global implant success rate (96.91%) that is higher than those reported by other similar series.11,16,28,29 Statistical analysis showed that this rate did not depend on the type of bone graft used, the presence of comorbidity or tobacco habit. In contrast to other studies, being a smoker did not have a negative effect in these patients30. However, the asymmetric and heterogeneous distribution of the independent variables made the use of non parametric statistical tests necessary for the analysis. This factor should be taken into account when interpreting the results.
Comparing the implant success rates of the implants placed simultaneously and delayed (averages of 98.65%± 7.57 and 93.57% ±16.43 respectively) there are statistically significant differences that favor simultaneous placement. However, due to fact that the average value of both rates is very high we don't consider this difference to be clinically relevant. There are diverse types of grafts that can be used in sinus lifts. These can be divided into 4 groups: autologous bone, allografts (obtained from human cadavers) alloplastic or synthetic grafts and xeno grafts (obtained from non human species like inorganic bovine bone) 1. For a long time autologous bone was considered to be the gold standard because of its high biocompatibility, high bone inductive potential and good clinical results.14,31,32 Retrieving autologous bone requires the approach of the donor site, which increases morbidity of the procedure especially when the donor site is extra oral. On the other hand, retrieving autologous bone from intraoral locations does not provide enough graft material for cases of severe maxilla atrophy. In order to avoid or reduce the risks associated with the retrieval of autologous bone many authors advise the use of other materials such as inorganic bovine bone, calcium sulfate and hydroxylapatite. However those materials are disadvantageous because they only present bone conductive qualities and, in some cases, cause strange bodily reactions. In order to minimize morbidity of the donor site without loosing potential autologous bone induction, the use of a combination of autologous bone and bone substitutes is highly recommended. 11,13,17,18,33 That is the reason why our series uses a combination of autologous bone and inorganic bovine bone in the majority of the cases where autologous bone was not enough. The most frequent complication was membrane tearing that was produced in 10.1% of cases. This percentage is similar to the one published by Wallace et al.34 and Zijderveld et al.35 We should mention that on the basis of the experience gained in this series the use of scrapers when lifting a sinus offers important technical advantages.8,9 It allows for the sinus window to be carved out and for chips of bone graft material to be retrieved simultaneously. The carving out of the window is done quickly and extremely carefully since it gives a great view of the membrane, which is especially useful when there are intrasinus divisions (Fig. 6) An average of 1cc of chips of bone graft is easily achieved which eliminates or lowers the need for autologous grafts from other areas, which notably reduces the morbidity of the procedure.
Conclusions
Sinus lift is a predictable, secure and versatile technique that allows for rehabilitation of implantation and prosthetic of an atrophic posterior maxilla. The implant success rates that we achieved are very high and don't depend on the type of graft used, associated morbidity or tobacco habit. The combined use of inorganic bovine bone and autologous bone allows for an implant success rate that is similar to the exclusive use of autologous bone but requires more time for the prosthesis to set. The use of bone scrapers for carving out the sinus window has many important technical advantages.
![]() Correspondence:
Correspondence:
Gui-Youn Cho Lee
Hospital Universitario de La Princesa. Madrid, España
C/ Diego de León, 62. 28006 Madrid, España
E-mail: gui-youncho@hotmail.com,
choguiyoun@gmail.com
Recibido: 22.11.2008
Aceptado: 31.03.2009
References
1. Kaufman E. Maxillary sinus elevation surgery: an overview. J Esthet Restor Dent 2003;15:272-82. [ Links ]
2. Truhlar RS, Orenstein IH, Morris HF, Ochi S. Distribution of bone quality in patients receiving endoosseous dental implants. Int J Oral Maxillofac Surg 1997;55:38-45. [ Links ]
3. Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. J Oral Implantol 1987;4 49-58. [ Links ]
4. Boyne PJ, James PA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 1980;38:613-6. [ Links ]
5. Tatum H. Maxillary and sinus implant reconstruction. Dent Clin North Am 1986;30:207-29. [ Links ]
6. Krennmair G, Krainhöfner M, Schmid-Schwap M, Piehslinger E. Maxillary sinus lift for single implant-supported restorations: a clinical study. Int J Oral Maxillofac Implants 2007;22:351-8. [ Links ]
7. Woo I, Le BT. Maxillary sinus floor elevation: review of anatomy and two techniques. Implant Dent 2004;13:28-32. [ Links ]
8. Martos-Díaz P, Naval-Gías L, Sastre-Pérez J, González-García R, Bances del Castillo F, Mancha de la Plata M, Galindo-Moreno P, Muñoz- Guerra M. Sinus elevation by in situ utilization of bone scrapers: technique and results. Med Oral Patol Oral Cir Bucal 2007;12:E537-41. [ Links ]
9. Naval-Gías L, Martos-Díaz P, González-García R, Naval B, Cho-Lee GY. Sinus lift by the use of bone scrapers: technique and results. Cranio Maxillofacial Surgery and Orthodontics. 2008;4-5:128-33. [ Links ]
10. Crespi R, Vinci R, Capparè P, Gherlone E, Romanos GE. Calvarial versus iliac crest for autologous bone graft material for a sinis lift procedure: a histomorphometric study. Int J Oral Maxillofac Implants 2007;22:527-32. [ Links ]
11. Galindo-Moreno P, Ávila G, Fernández-Barbero JE, Aguilar M, Sánchez- Fernández E, Cutando A, Wang HL. Evaluation of sinus floor elevation using a composite bone graft mixture. Clin Oral Impl Res 2007;18:376-82. [ Links ]
12. Schwartz Z, Goldstein M, Raviv E, Hirsch A, Ranly DM, Boyan BD. Clinical evaluation of demineralized bone allograft in a hyaluronic acid carrier for sinus lift augmentation in humans: a computed tomography and histomorphometric study. Clin Oral Implants Res 2007;18:204-11. [ Links ]
13. Barone A, Crespi R, Aldini NN, Fini M, Giardino R, Covani U. Maxillary sinus augmentation: histologic and histomorphometric analysis. Int J Oral Maxillofac Implants 2005;20:519-25. [ Links ]
14. Thorwarth M, Srour S, Felszeght E, Kessler P, Schultze-Mosgau S, Schlegel KA. Stability of autogenous bone grafts after sinus lift procedures: a comparative study between anterior and posterior aspects of the iliac crest and an intraoral donor site. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;100:278-84. [ Links ]
15. Steigmann M, Garg AK. A comparative study of bilateral sinus lifts performed with platelet-rich plasma alone versus alloplastic graft material reconstituted with blood. Implant Dent 2005;14:261-6. [ Links ]
16. McCarthy C, Patel RR, Wragg PF, Brook IM. Sinus augmentation bone grafts for the provision of dental implants: report of clinical outcome. Int J Oral Maxillofac Implants 2003;18:377-82. [ Links ]
17. Karabuda C, Ozdemir O, Tosun T, Anil A, Olgaç V. Histological and clinical evaluation of 3 different grafting materials for sinus lifting procedure based on 8 cases. J Periodontol 2001;72:1436-42. [ Links ]
18. Yildirim M, Spiekermann H, HandtS, Edelhoff D. Maxillary sinus augmentation with the xenograft Bio-Oss and autogenous intraoral bone for qualitative improvement of the implant site: a histologic and histomorphometric clinical study in humans. Int J Oral Maxillofac Implants 2001;16:22-33. [ Links ]
19. Raghoebar GM, Brouwer TJ, Reintsema H, Van Oort RP. Augmentation of the maxillary sinus floor with autogenous bone for the placement of endosseous implants: a preliminary report. J Oral Maxillofac Surg 1993;51:1198-203. [ Links ]
20. Smiler DG, Johnson PW, Lozada JL, et al. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent Clin North Am 1992; 6:151-86. [ Links ]
21. Thor A, Sennerby L, Hirsch JM, Rasmusson L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: an evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg 2007;65:64-72. [ Links ]
22. Chen TW, Chang HS, Leung KW, Lai YL, Kao SY. Implant placement immediately after the lateral approach of the trap door window procedure to create a maxillary sinus lift without bone grafting: a 2- year retrospective evaluation of 47 implants in 33 patients. J Oral Maxillofac Surg 2007;65:2324-8. [ Links ]
23. Muñoz-Guerra MF, Naval-Gías L, Escorial V, Sastre-Pérez J. Dentin dysplasia type I treated with onlay bone grafting, sinus augmentation, and osseointegrated implants. Implant Dent 2006;15:248-53. [ Links ]
24. Wiltfang J, Schultze-Mosgau S, Nkenke E, Thorwarth M, Neukam FW, Schlegel KA. Onlay augmentation versus sinuslift procedure in the treatment of the severely resorbed maxilla: a 5-year comparative longitudinal study. Int J Oral Maxillofac Surg 2005;34:885-9. [ Links ]
25. Halpern KL, Halpern EB, Ruggiero S. Minimally invasive implant and sinus lift surgery with immediate loading. J Oral Maxillofac Surg 2006;64:1635-8. [ Links ]
26. Cawood JI, Howell A. Reconstructive preprosthetic surgery. I. Anatomical considerations. J Oral Maxillofac Surg 1991;23:75-82. [ Links ]
27. Zinner ID, Small SA. Maxillary sinus grafts and prosthetic management. In: Zinner ID, Panno V (eds). Implant Dentistry: From Failure to Success. Hong-Kong: Quintessence, 2004:99-100. [ Links ]
28. Kent JN, Block MS. Simultaneous maxillary sinus floor bone grafting and placement of hydroxiapatite-coated implants. J Oral Maxillofac Surg 1989;47:238-42. [ Links ]
29. Blomquist JE, Alberius P, Isaksson S. Two-stage maxillary sinus reconstruction with endosseous implants. A prospective study. Int J Oral Maxillofac Implants 1998; 13: 758-66. [ Links ]
30. Kan JYK, Rungcharassaeng K, Lozada JL, Goodacre CJ. Effects of smoking on implants success in grafted maxillary sinuses. J Prosthet Dent 1999; 82: 307-11. [ Links ]
31. Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int Oral Maxillofac Implants 1998; 13(Suppl): 11-45. [ Links ]
32. González-García R, Naval-Gías L, Muñoz-Guerra MF, Sastre-Pérez J, Rodríguez-Campo FJ, Gil-Díez Usandizaga JL. Preprosthetic and implantological surgery in patients with severe maxillary atrophy. Med Oral Patol Oral Cir Bucal 2005;10:343-54. [ Links ]
33. Hallman M, Cederlund A, Lindskog S, Lundgren S, Sennerby L. A clinical histological study of bovine hydroxiapatite in combination with autogenous bone and fibrin glue for maxillary sinus floor augmentation Results over 6 to 8 months of healing. Clin Oral Implants Res 2001;12:135-43. [ Links ]
34. Wallace SS, Mazor Z, Froum SJ, Cho SC, Tarnow DP. Schneiderian membrane perforation rate during sinus elevation using piezosurgery: clinical results of 100 consecutive cases. Int J Periodontics Restorative Dent. 2007;27:413-9. [ Links ]
35. Zijderveld SA, Van der Bergh JPA, Schulten E, Bruggenkate CM. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J Oral Maxillofac Surg 2008;66:1426-38. [ Links ]











 texto en
texto en