Obsessive-compulsive disorder (OCD) is a mental disorder in which people experience uncontrollable, intrusive thoughts (obsessions), which may be accompanied by distressing and repetitive mental/behavioral acts (compulsions). Obsessions and compulsions negatively affect quality of life among people with OCD (American Psychiatric Association [APA, 1994]). Over the last 15 years, several empirical studies have also shown that OCD has an adverse effect on relatives' quality of life and the presence of OCD symptoms has been linked to family accommodation and elevated expressed emotion between family members (Cicek et al., 2013; Gomes et al., 2016; Lebowitz et al., 2012). For instance, the presence of contamination obsessions may lead patients to involve family members in their cleaning rituals (family accommodation) or may result in conflicts with them because their reluctance to participate in or accept these compulsions (high expressed emotion). Also, growing research points out that relatives of people with OCD have high rates of psychopathology (Maliken & Katz, 2013). Regarding parents with OCD, community and family studies have shown that their children are at greater risk of suffering from mental disorders in general when compared with parents without OCD. Current data indicate children have greater prevalence of obsessive-compulsive spectrum disorders, major depression, autism, schizophrenia, and anorexia nervosa (Black et al., 2003; Browne et al., 2015; Meier et al., 2014; Meier, Bulik, et al., 2015; Meier, Peersen, et al., 2015). Also, research focused on the assessment of emotional symptoms has shown that children of parents with OCD are at higher risk of having internalizing, but not externalizing symptoms (Black et al., 2003; Boyd & Tervo-Clemmens, 2013; Challacombe & Salkovskis, 2009). However, these findings have been methodologically limited because they were mostly found when compared with control groups without any other primary psychiatric disorder. Unlike healthy controls, parents with other psychiatric disorders may exhibit emotional symptoms (depression, anxiety), which are also usually observed in parents with OCD beyond their primary diagnosis (Goodwin, 2015). Hence, by including parents with other psychiatric disorders as control groups, the findings obtained could be more specifically linked to parental OCD because other overlapping symptoms may be controlled. Ultimately, the need to address emotional symptoms in children of parents with OCD is warranted because psychological problems are likely to be subtle or subclinical across childhood, possibly manifesting as diagnosable mental disorder only later in their lives (Liu, 2016).
As part of this issue, the intergeneration transmission of psychopathology from parents with OCD to children through genetic heritance and/or environmental factors is still a matter of debate. On the one hand, there is preliminary evidence from family studies supporting the presence of genetic load for intergeneration transmission of OCD through altered glutamatergic transmission (Pauls, 2010). On the other hand, the few empirical studies focused on the influence of environmental factors have shown that parenting attitudes among parents with OCD did not influence their children's risk for OCD or that this association was only evidenced for mothers with OCD (vs. fathers with OCD; Black et al., 2003; Wilcox et al., 2008). In spite of the lack of firm evidence, there is still a need for delineating the link between parenting attitudes in parents with OCD and the risk of psychopathology on their children, including but not limited to childhood OCD. First, because Developmental Psychology in general and attachment theories in particular stress that parenting attitudes represent a key cognitive predisposition underlying child-rearing and children's emotional development (Leavitt, 1999). Second, because several observational studies have found that specific parenting attitudes (e.g., overprotection) were more prevalent among mothers with OCD when compared with healthy controls, although group differences were partly accounted for by comorbid major depression or general anxiety levels (Challacombe et al., 2016; Challacombe & Salkovskis, 2009; Reich, 2008). Accordingly, there could be only some accurate features of this broad construct linked to parental OCD. This is relevant taking into account that parenting attitudes represents a broad concept covering several aspects such as satisfaction with parenting, involvement, discipline or autonomy (Gerard, 1994). Third, it is also needed because previous studies in other psychiatric samples have reported that parenting attitudes in parents with major depression, borderline personality disorder, or eating disorders may negatively affect children's emotional development, and vice versa (Bartsch et al., 2015; Tsypes & Gibb, 2015). Overall, by finding specific parenting attitudes in people with OCD and their influence on their children's emotional symptoms, clinicians could tailor parenting therapies aimed at preventing or ameliorating this environmental risk factor (Challacombe et al., 2017; Reich, 2008).
Within this clinical framework, the main aims of this empirical, exploratory study were: i) to delineate whether children of parents with OCD had significantly greater emotional symptoms when compared with children of parents without OCD; ii) to elucidate whether parents with OCD had significantly poorer parenting attitudes when compared with parents without OCD – if so, to verify this after controlling for parents' and children's differences in severity of depression and anxiety; and iii) within parents with OCD, to determine whether there were any OCD features significantly associated with any emotional symptoms in their children. If so, to elucidate the mediation role of any parenting attitudes on this relationship.
Method
Participants
Detailed data on the selection process is depicted in Figure 1. Forty Caucasian parents with a current primary diagnosis of OCD were consecutively recruited from the Adult Outpatient Mental Health Center of Mataró (Barcelona) from January 2015 to September 2016. A control group composed of 37 Caucasian parents with a current primary diagnosis of adjustment disorder and matched for sociodemographic variables was also collected from this clinical setting. A comparison group of parents with adjustment disorders was chosen because our purpose was to delineate whether parenting attitudes in people with OCD could be disorder-specific. For this reason, and following Challacombe and Salkovskis (2009), we included another clinical group as a control condition. Particularly, a diagnosis of an adjustment disorder represents a broad clinical category of mixed symptoms (e.g., anxiety, depression), which are also usually observed in people with OCD and may be controlled in order to exclude symptom-specific parenting attitudes. The current main diagnoses for both clinical groups were based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA, 1994).
Inclusion criteria for both groups were: 1) parents should be primary caregivers and have at least one targeted child living partly or fully with them; 2) children assessed should be aged 7-16 in order to meet age criteria for the questionnaires noted below (see Assessment Instruments). Exclusion criteria were: 1) for both groups, prior diagnoses of neurological disorder, intellectual disability, autism, or schizophrenia according to chart reviews; 2) for both groups, current (hypo)manic episode and/or substance intoxication/withdrawal; 3) for the non-OCD group, a lifetime diagnosis of OCD; 4) for the OCD group, a lifetime diagnosis of adjustment disorder.
Patients from both groups received naturalistic treatment consisting of individual bimonthly cognitive-behavioral therapy implemented by their clinical psychologists. Also, antidepressant prescriptions were as follows when recruited: for the OCD-group, 26 participants took selective serotonin reuptake inhibitors (SSRIs) and 19 received tricyclic antidepressants; for the non-OCD group, 31 took SSRIs, two received tricyclic antidepressants, and six were prescribed selective serotonin noradrenaline reuptake inhibitors.
Patients were initially referred to us by their main clinicians (mostly psychiatrists) once they were initially diagnosed at intake with the required mental disorders. All patients were from different families. Patients attended one assessment session conducted by the authors of the current research, on average 3.4 (± 1.7) months after their tenure with the treatment center. The authors are psychiatrists and clinical psychologists widely experienced in OCD. First, assessment interviews were held with each parent to ensure main diagnoses and exclude other current mental disorders. In all cases, diagnoses at intake were confirmed by the researchers using standardized assessment instruments. Then, each parent and his/her child separately completed self-report questionnaires in different rooms. The study was approved by the hospital's institutional review board, and informed consent was obtained from all parents after a full explanation of the nature of the study. Parental consent for children participation in the study was also obtained.
All procedures performed in studies involving human participants and/or animals were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Assessment Instruments
Parents' assessment
Structured Clinical Interview for DSM-IV Axis I Disorders. The Spanish translation of the SCID-I/P (research version, patient edition) was used for diagnosing OCD and adjustment disorders. Also, it was employed for ruling out other current mental disorders according to the exclusion criteria (First et al., 1995).
Yale-Brown Obsessive-Compulsive Scale (Y- BOCS). Y-BOCS' Spanish version was used to determine the severity and content of any current OC symptoms. Cronbach's alpha coefficients range from .87 to .94. A cut-off score > 15 for the total Y-BOCS is considered clinically significant (Vega et al., 2002).
Parent-Child Relationship Inventory (PCRI). PCRI's Spanish version was used. This is a self-reported questionnaire which was used to measure parental attitudes towards parenting. It comprises 78 items with four response options (totally disagree, disagree, agree, and strongly agree), which are grouped into seven subscales. The seven subscales are support, satisfaction with parenting, involvement, communication, discipline, autonomy, and role orientation, along with a social desirability subscale. Cronbach's alpha coefficients range from .68 to .78 (Roa & Del Barrio, 2001).
Spielberger State-Trait Anxiety Inventory (STAI- S/T). STAI-S/T's Spanish validation was used to assess anxiety severity. Cronbach's alpha coefficients are .87 and .93. A cut-off score of 39-40 has been suggested to detect clinically significant symptoms for the STAI subscales (Spielberger et al., 1982).
Beck Depression Inventory (BDI). The Spanish validation of the 13-item BDI short form was used to assess depression symptom severity. Cronbach's alpha coefficient was .90. Adults with a cut-off score of 13/14 are considered at risk for clinical depression (Conde & Useros, 1975).
Children's assessment
Children's Depression Inventory (CDI). CDI's Spanish validation was used to assess depression symptom severity. This self-reported questionnaire provides a total score based on 27 items scored according to one of the following alternatives: 0 = absence of the symptom, 1 = moderate symptom, 2 = severe symptom. Youth with cut- off score ≥ 13 are considered at risk for clinical depression. Cronbach's alpha coefficient was .82 (Del Barrio, 1999).
Revised Children's Manifest Anxiety Scale (R-CMAS). R-CMAS' Spanish validation, testing anxiety symptom severity, was used. This self-reported questionnaire consists of 37 items. A total anxiety score is based on 28 items, which are in turn divided into three anxiety subscales: physiological anxiety, restless/hypersensitivity and social concerns/concentration. Also, there are nine additional items that corresponded to a Lie subscale. Score of each subscale was determined by the number of items answered with "yes" (= 1). Youth with a cut-off score of > 18 for the total anxiety are considered at risk for anxiety disorders. Cronbach's alpha ranges between .79 and .85 (Reynolds, 1997).
Piers-Harris Children's Self-Concept Scale (PH-CSCS). PH-CSCS' Spanish validation was used to assess self-esteem. This self-reported questionnaire consists of 80 items, each scored 1 ("yes") or 0 ("no"). The item scores are summed to yield a total score and six factor scores: physical appearance, intellectual and school status, freedom from anxiety, behavior, happiness and satisfaction, and popularity. Higher scores for total self-concept and factor scores reflect a more positive self-concept. Cronbach's alpha ranges between .75 and .83 (Cardenal & Fierro, 2003).
Statistical Analysis
Chi-square test and t-test were first used to analyze the sociodemographic data. Then the Shapiro-Wilk test was used to confirm the normal distribution of quantitative clinical data for both groups. Also, Levene's test for homogeneity of variance was performed before testing for between-group differences on clinical data.
One-way multivariate analysis of variance (MANOVA) was used to test for significant differences between both groups, either in parents' anxiety/depression symptom severity (STAIS/T, BDI) or in their children's emotional symptoms (CDI, R-CMAS, PH-CSCS). Then one-way multivariate analyses of covariance (MANCOVA) was conducted to look for between-group differences in parenting attitudes (PCRI), after controlling for general anxiety levels (STAI-S/T), depression symptom severity (BDI), and emotional symptoms in their children (CDI, R-CMAS, PH-CSCS).
Within the OCD group, hierarchical linear regression analyses were then conducted to determine the mediating role of parenting attitudes (PCRI) in the relationship between OCD features (Y-BOCS) and emotional symptoms in their children (CDI, total score from the R-CMAS and the PH-CSCS). Mediation analysis followed the method by Baron and Kenny (1986), which has usually provided the same results compared with other tests (e.g., Sobel test) used to assess indirect effects. The regression analyses at step 1 included each OCD feature (Y- BOCS) as a univariate predictor and each emotional symptom as a dependent variable (CDI, total score from the R-CMAS, and the PH-CSCS). The regression analyses at step 2 included each OCD feature (Y-BOCS) as a univariate predictor and each parenting attitude (PCRI) as a dependent variable. At step 3, bivariate regression analyses included several models resulting from the interaction between each significant OCD feature (Y-BOCS) at both prior steps and each parenting attitude (PCRI). Emotional symptoms (CDI, total score of the R-CMAS and the PH-CSCS) were dependent variables. A particular model would fully support the mediation hypothesis if the OCD feature (Y-BOCS) was no longer significant while the parenting attitude (PCRI) was significant. At step 4, multiple regression analyses including parents' psychopathology (BDI, STAI-S) were performed to further ensure the mediation model.
Standardized regression coefficients (β) were used as measures of effect sizes for stepwise linear regression analyses, while partial eta squared (η2) were employed for MANOVA and MANCOVA. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS 18.0). All tests were two-tailed and p-values of less than .05 were considered statistically significant.
Results
Sociodemographic Features of Parents with and without OCD and Their Respective Children
As detailed in Table 1, there were no statistically significant differences in sociodemographic features between parents with OCD (n1 = 40) and non-OCD (n2 = 37) and between their respective children (p > .05). Basically, both groups consisted of middle-aged parents, predominantly female, who lived with the other parent. Over half of both parents' groups were unemployed at the time of the assessment. The targeted samples of children (n1 = 46 and n2 = 40) were mostly in early adolescence and equally composed by gender.
Clinical Comparison between Parents with OCD and without OCD
Concerning parents' psychopathology, the MANOVA reported a statistically significant difference between groups (F = 14.56, df = 13, 63, p < .001, Wilks λ = .65). As shown in Table 2, univariate analyses showed that depression symptom severity (BDI) was statistically significantly greater in the non-OCD group (F = 3.38, p = .05), while general anxiety severity (STAI-S/T) was statistically significantly higher in the OCD group (F = 9.9, p = .02; F = 3.83, p = .04). For both groups, raw scores on depression severity were clinically significant, while anxiety scores ranged on subclinical intervals.
Clinical Comparison between Children from Parents with OCD and without OCD
Regarding children's emotional symptoms, the MANOVA reported a statistically significant difference between groups (F = 37.95, df = 13, 72, p < .001, Wilks λ = .12). As detailed in Table 3, univariate analyses showed that depression symptom severity (CDI) and anxiety levels (R-CMAS) were statistically significantly higher in children of parents with OCD compared to children of parents without OCD (p < .05). Also, children of parents with OCD reported statistically significantly lower self-esteem (PH-CSCS; p < .05). None of the outcome measures were clinically significant for either group, but scores on depression and anxiety symptom severity were at subclinical levels among children of parents with OCD.
Comparison between Parents with and without OCD in Parenting Attitudes
Concerning parenting attitudes, the MANCOVA reported a statistically significant difference between groups, after controlling for parents' and children's emotional symptoms (BDI, STAI-S/T, CDI, R-CMAS, PH-CSCS; F = 430.92, df = 8, 66, p < .001, Wilks λ = .01). As detailed in Table 4, univariate analyses showed that, except for social desirability, the remaining parenting attitudes were statistically significantly poorer in parents with OCD relative to parents without OCD (p < .05).
Mediation Role of Parenting Attitudes on the Relationship between Parents' OCD Features and Children´s Emotional Symptoms
Initial descriptive analyses showed that parents with OCD reported clinically significant OCD symptoms (Y-BOCS total, M = 22.3, SD = 4.91). Over half of them recognized having either contamination (60%) or symmetry obsessions (60%). Also, parents with OCD usually presented cleaning (65%), arranging (60%), and repetition compulsions (50%).
Hierarchical linear regression analysis was performed to test whether any parenting attitude (PCRI) may mediate the association between parents' OCD features (Y-BOCS) and children's emotional symptoms (CDI, R-CMAS, PH-CSCS). Table 5 shows each step for those models fully meeting the mediation hypothesis. At step 1, the presence of aggressive and somatic obsessions was found to significantly predict both children's depression (β = .53, p < .001; β =. 42, p = .003) and total anxiety severity (β = .43, p = .003; β = .30, p = .04). The presence of sexual obsessions also significantly predicted children's total anxiety severity (β = .31, p = .03). Neither content nor severity of compulsions were significantly associated with any emotional symptom in children (p > .05). Also, children's self-esteem was not significantly predicted by any OCD feature in parents (p > .05). At step 2, the presence of sexual and somatic obsessions was found to significantly predict parental involvement (β = .33, p = .02; β = .32, p = .02). Unlike in step 1, aggressive obsessions did not significantly predict any parenting attitude (p > .05). At step 3, models including children's depression severity as a dependent variable did not meet the full mediation hypothesis. However, sexual and somatic obsessions were no longer significant predictors of children's total anxiety (β = .19, p = .17; β = .19, p = .19) when parental involvement was included in both models (β = .32, p = .03; β = .33, p = .02). At step 4, both full mediation models were confirmed after controlling for depression and anxiety severity in parents with OCD (Figure 2 and 3).
Table 5. Hierarchical Linear Regression Analyses for Those Models Fully Meeting Mediation Role of Parenting Attitudes in the Relationship between Parents' OCD Features (n = 40) and Children's Emotional Development (n = 46)
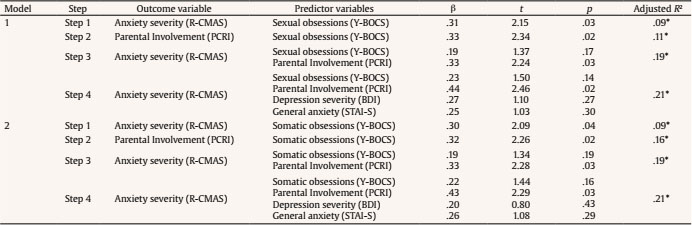
Note.OCD = obsessive-compulsive disorder. Parents' measures: BDI = Beck's Depression Inventory; PCRI = Parent-Child Relationship Inventory; STAI-S = Spielberger Trait-State Anxiety Inventory; Y-BOCS = Yale-Brown Obsessive-Compulsive Scale. Children's measures: R-CMAS = Revised Children Manifest Anxiety Scale.
*p < .05

Note. BDI = Beck's Depression Inventory; CMAS-R = Revised Children's Manifest Anxiety Scale; PCRI = Parent-Child Relationship Inventory; STAI-S = Spielberger State-Trait Anxiety Inventory; Y-BOCS = Yale-Brown Obsessive-Compulsive Scale. The figure in parenthesis refers to β, *p < .05.
Figure 2. Full Mediation Model: Effect of Parents' Sexual Obsessions on Children's Total Anxiety Severity through Parental Involvement, after Controlling for Parents' General Anxiety/Depression Symptoms.

Note. BDI = Beck's Depression Inventory; CMAS-R = Revised Children's Manifest Anxiety Scale; PCRI = Parent-Child Relationship Inventory; STAI-S = Spielberger State- Trait Anxiety Inventory; Y-BOCS = Yale-Brown Obsessive-Compulsive Scale.
Figure 3 Full Mediation Model: Effect of Parents' Somatic Obsessions on Children's Total Anxiety Severity through Parental Involvement, after Controlling for Parents' General Anxiety/Depression Symptoms.
Discussion
This study sought to delineate distinctive parenting attitudes in people with obsessive-compulsive disorder (OCD), specific emotional symptoms in their children, and the association between them. Main findings from the current research showed: 1) children of parents with OCD reported significantly greater anxiety and depression symptoms when compared with children of parents diagnosed with adjustment disorders; 2) after controlling for parents' and children's emotional symptoms, parents with OCD reported significantly poorer overall parenting attitudes relative to parents with adjustment disorders; and 3) within the OCD sample, parental involvement mediated the relationship between sexual/somatic obsessions in parents and anxiety in their children.
Similar to other previous studies, the current research showed that children of parents with OCD reported greater presence of internalizing/emotional symptoms than children of control parents (Black et al., 2003; Boyd & Tervo-Clemmens, 2013; Challacombe & Salkovskis, 2009). This finding may be considered disorder-specific, taking into account that we included a control group composed of parents with a different primary psychiatric disorder who also exhibited depression and anxiety symptoms. Unlike the current study, the research by Challacombe and Salkovskis (2009) did not reveal significant differences in internalizing/emotional symptoms between children of parents with OCD and children of parents with panic disorder. Regarding the latter study, it is likely that some clinical differences between both psychiatric groups were overlooked because of the small sample sizes (n < 24). Apart from this finding, the fact that children of parents with OCD reported subclinical levels for these internalizing/emotional symptoms may also suggest the need to carry out longitudinal assessment in order to identify the subset of children who may eventually develop clinically significant symptoms later on (Liu, 2016).
In accordance with prior research, the current study found that parenting attitudes were poorer in parents with OCD than controls (Challacombe et al., 2016; Challacombe & Salkovskis, 2009; Farrell et al., 2013). However, poor parenting was not limited to specific attitudes. It should be noted that methodological divergences between the current and prior research may account for differences in parenting. Unlike these other studies, our study consisted of not only mothers with OCD, but also fathers with OCD. In addition, our samples of children were older than those used in the other studies. Because of these divergences, further research is warranted aimed at addressing parenting differences by parents' gender and children's age. Also, forthcoming studies should take into account the role of the other parent or caregiver, if present. Regarding this issue, it is likely that some clinical characteristics closely associated with couples (e.g., low marital support) may moderate parenting attitudes among parents with OCD, for example by increasing over-involvement towards children (Taraban et al., 2017). Also, the presence of adequate parenting attitudes (e.g., warmth, optimism, distress tolerance) in the other parent or caregiver may serve as a buffer against poor parenting attitudes in the parent with OCD (Rosa-Alcázar et al., 2019).
Interestingly, when analyzing subtypes of OCD symptoms in parents with OCD, obsessions rather than compulsions were associated with internalizing/emotional symptoms in their children. Specifically, the association between somatic/sexual obsessions in parents with OCD and anxiety symptoms in their children was mediated by parental involvement. To the best of our knowledge, this is the first empirical study which shows the extent to which specific OCD symptoms in parents may predict emotional symptoms in their children. The fact that parenting involvement acted mostly as a mediator variable suggests that the presence of intrusive and unwanted thoughts, commonly associated with their children (e.g., fear of disease contagion or sexual assault), may predispose parents with OCD to higher hyper-responsibility and over-involvement in terms of parenting (Abramowitz et al., 2003). As a result, children may be exposed to a modelling of anxious behavior by parents, which in turn may sensitize children to anxious reactions throughout their lives (Murray et al., 2009). Also, following cognitive models, this pernicious effect within OCD dyads may enhance children's personal sense of responsibility and an inflated threat perception in their lives (Farrell et al., 2013; Pietrefesa et al., 2010). Ultimately, the aforementioned relationship should be addressed even in mothers with OCD in the perinatal (postpartum) period, where the presence of intrusive thoughts is highly prevalent (Collardeu et al., 2019).
The current study has several limitations. First, both groups had relatively small sample sizes, though similar to other related studies (Challacombe et al., 2016). In spite of this fact, effect sizes were usually large, which added substantive relevance to these findings. Second, assessment of parenting attitudes relied on a self-report questionnaire instead of using observational methods by independent raters within parent-child dyads (Challacombe & Salkovskis, 2009). To attenuate this limitation, confounding effects from parents' depression and anxiety symptomatology were controlled for when analyzing data on parenting. Third, data from categorical diagnoses were not obtained for children cohorts (e.g., OCD) as well as for comorbid disorders in both parents groups (e.g., major depression disorder), except for exclusion criteria. Hence, our results are particularly relevant for dimensional approaches to psychopathology. Fourth, the study sample was a convenience sample of individuals being served by one particular clinic and cannot be seen as definitive nor generalizable to all parenting adults with OCD. Fifth, the choice of the comparison group (parents with an adjustment disorder), whose clinical symptoms were broad and self-limited by definition, limits the extent to which our results on parenting among OCD parents may be assumed to be disorder-specific. Sixth, the cross-sectional nature of the study impedes establishing causal relationships between variables. Hence, longitudinal studies should be prioritized in forthcoming research.
In sum, parents with OCD may exhibit overall poor parenting attitudes, which could be disorder-specific and independent of other co-occurring symptoms. Specifically, some parents' obsessions may predispose children to greater levels (subclinical) of anxiety severity through parental involvement. Clinical implications from these findings are: 1) clinicians should assess parenting attitudes in those patients with OCD that are periodically treated with cognitive-behavior therapy; 2) the presence of intrusive thoughts in parents with OCD, specially somatic/sexual obsessions, should be prioritized as a target intervention, not only for own patients, but also for their children's well-being (Reich, 2008); 3) children of parents with OCD at high-risk for anxiety symptoms should be assessed at least in order to prevent the presence of more relevant psychopathology at mid/long-term; and 4) parenting interventions either in individual or parent-child format sholud be developed by implementing clinical trials in patients with OCD.



















