Introduction
HIV infection has undergone a huge transformation since the first cases were diagnosed, at the start of the 80s. These changes have occurred not only due to the variation in the transmission ways and distribution of new patients incorporated for clinical follow-up, but also due to the great changes experienced in the survival of persons infected with HIV, thanks to a generalized access to effective antiretroviral treatment combinations (ARTs)1. As a result, the future of HIV care will require a change of mentality. So far, patient care has focused on the morbimortality associated with HIV/AIDS; in the next years, this approach will turn towards a scenario where the health experience of the HIV+ population will resemble increasingly that of the non-infected population, because their life expectancy will be increasingly similar to that of the overall population2. This has led to the use of concepts so far seldom associated with this type of patients, such as pluripathology or polypharmacy, because some studies show that the risk of suffering complications not associated with AIDS is higher than in the overall population3,4 . In this sense, there has been research on cardiovascular conditions5,6, neoplasias7,8, liver conditions 9, chronic renal disease10, osteoporosis11,12, or neurocognitive disorders13. Similarly, an increasing number of publications show an increase in polypharmacy in this type of patients, an aspect that so far has been treated from a qualitative and less quantitative perspective, and how to manage it in real practice14.
It goes without saying that overall patient care, and particularly Pharmaceutical Care for this type of patients, must adapt to these new circumstances. The American model for pharmaceutical practice already included within its recommendations the need for patient follow-up based on a pharmacotherapy complexity index15. Until then, the only publication was precisely the study by Martín S et al.16, for HIV patients, that has been adapted and used in our setting with an on-line adaptation and update. However, this index referred exclusively to the complexity of antiretroviral treatment. Other authors have developed assessments for the quantitative estimation of the level of complexity of the complete pharmacotherapy, even with an analysis of its importance for HIV+ patients, though this has been mostly used in the outpatient setting17,18.
However, even though there are studies conducted on HIV+ population that evaluate certain treatment aspects (errors, pharmacy interventions, interactions), so far no study has analyzed the impact of hospital admission in the pharmacotherapy complexity of this type of subjects19-21.
The objective of this study is to know the impact of hospital admission in the pharmacotherapy complexity index (CI) of HIV+ patients.
Method
A retrospective, single-centre study, including all HIV+ patients who were admitted to a hospitalization ward between the years 2006 and 2014 were conducted. The study excluded all those patients with a hospital stay <24 hours, or those without record of the minimum data necessary to conduct the study.
Hospital admission was defined as a >24 hour stay in a hospitalization ward, excluding visits to the Hospital ER or observation.
The following variables were collected: demographical (age, gender and transmission path), analytical results such as plasma viral load (copies/mL) and CD4 lymphocyte count (cell/uL), clinical (duration and cause of the admission, previous hospitalizations during the past year, CDC stage and number and type of infectious and non-infectious comorbidities (including co-infection with the hepatitis virus), social (Barthel Index, education, living alone, mental disorders, socioeconomic difficulties, addiction to drugs/ alcohol), and finally pharmacotherapeutical variables, including antiretroviral and concomitant treatment, and adherence to ART before and after admission.
The primary endpoint of the study was the variation in the overall pharmacotherapy complexity index before and after hospital admission. The MCRI tool was used for calculating this index; this tool has been designed and validated by the University of Colorado, and is available in the following link: http://www.ucdenver.edu/academics/colleges/pharmacy/Research/researchareas/Pages/researchareas.aspx
The secondary objective was the analysis of the potential factors associated with the variation in the complexity index.
For the calculation of adherence to ART, the SMAQ questionnaire was used, as well as the dispensing records for six months before and after hospital admission. The combination of drugs administered was obtained through the dispensing program for outpatients of the Pharmacy Unit (Dominion).
The rest of variables were obtained through computer search of the patient’s Single Clinical Record.
In order to conduct the statistical analysis, data refinement was initially conducted, followed by a description of said data. Quantitative variables were summarized with means and typical deviations; or, in case of asymmetrical distributions, with medians and percentiles (P25 and P75); percentages were used for qualitative variables.
In order to compare the mean of quantitative variables, Student’s t test was used for paired samples, as well as Wilcoxon’s nonparametric test. Previously, data normality was confirmed through the Kolmogorov-Smirnov test, in order to decide on the use of parametric or non-parametric tests.
McNemar’s Test was used to analyze the modification in dichotomous variables before and after hospital admission.
Finally, and with the objective to find prognostic factors for the increase in the complexity index, a binary logistical regression model was conducted after a previous univariate analysis, in order to identify the independent variables associated with this increase. If any variables were found, these would be entered into a multivariate model for their final selection (p < 0.30).
Results
The study included 146 patients (84.9% male) with 45.3 ± 9.1 years as mean age. In the majority of cases (80.1%), the disease was contracted through parenteral use of drugs. At the time of admission, 62.2% of those patients with data presented undetectable viral load, and 70.9% had an acceptable immunological status, defined as a CD4 lymphocyte count >250 cell/µL22.
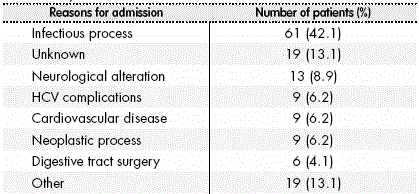
Of these patients, 30.8% had been admitted to hospital once during the previous year, with 7 days as median hospital stay (IQR: 4.0-12-5). The main causes for admission are shown in figure 1.
Two or more non-infectious comorbidities were experienced by 31.8% of patients; while 79.5% of patients suffered at least one infectious comorbidity; it is worth highlighting that 79.5% of patients were co-infected with the Hepatitis C virus. Table 1 shows the basal demographical and clinical characteristics of the patients included in the study.
Table 1 Demographical, analytical and clinical characteristics of the population at baseline.
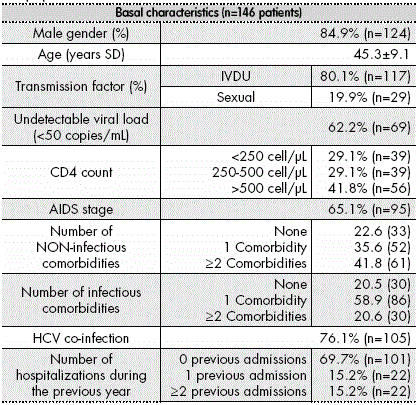
SD: Standard Deviation; IVDU: Intravenous Drug User; HCV: Hepatitis C virus.
Barthel Index was assessed in 38 patients; 76.1% of them had >80 scores out of 100. Only eight patients provided information about their level of education, five about their family support, and seven about their financial problems.
The main antiretroviral treatment was based in a combination with a protease inhibitor (45.9% of patients), followed by 39.7% patients treated with a combination of 2 Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs) plus 1 Non-nucleoside Reverse Transcriptase Inhibitor (NNRTI); while 4.1% patients were on a combination of 2 NRTIs + Integrase Inhibitors (INSTIs). The remaining 10.3% of patients had been prescribed other non-conventional treatments.
Regarding concomitant medication, the mean number of drugs prescribed per patient was 2.3 ± 2.1; the most frequently prescribed drugs were those used against opioid dependency in 45 patients (13.4%), followed by anxiolytics in 41 patients (12.2%) and drugs for prevention and treatment of peptic ulcer in 40 patients (11.9%). The distribution of the rest of drugs appears in figure 3.
When analysing the primary variable, the overall mean CI previous to admission was 14.5 ± 7.2 vs. 16.5 ± 8.0 after admission, reaching statistical significance (1.97 (CI: 0.85; 3.09)). An identical conclusion was obtained from the non-parametric test (p = 0.001).
Regarding the assessment of adherence to ART, 58.3% of patients were adherent before admission vs. 41.8% who were adherent after admission (p = 0.023).
Finally, there was an analysis of potential factors responsible for an increase in complexity during admission. The multivariate analysis included treatment with NRTIs, treatment with INSTIs, taking ≥ 5 concomitant drugs, and a high basal pharmacotherapeutical complexity. The only factor associated with an increase in complexity was the prescription of 5 or more chronic drugs before admission, which triples the risk of increase in complexity after admission (OR = 3.146 (1.045- 9.471)). The complete outcomes for univariate and multivariate analysis are shown in Table 2, Table 3 and Table 4
Table 3 Distribution of the pharmacological groups more widely used by patients as concomitant medication.
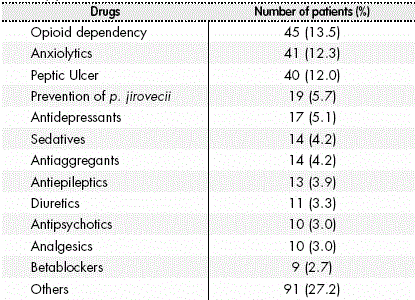
Table 4 Factors predicting an increase in complexity in HIV+ patients after hospital admission. Univariate and multivariate analysis.
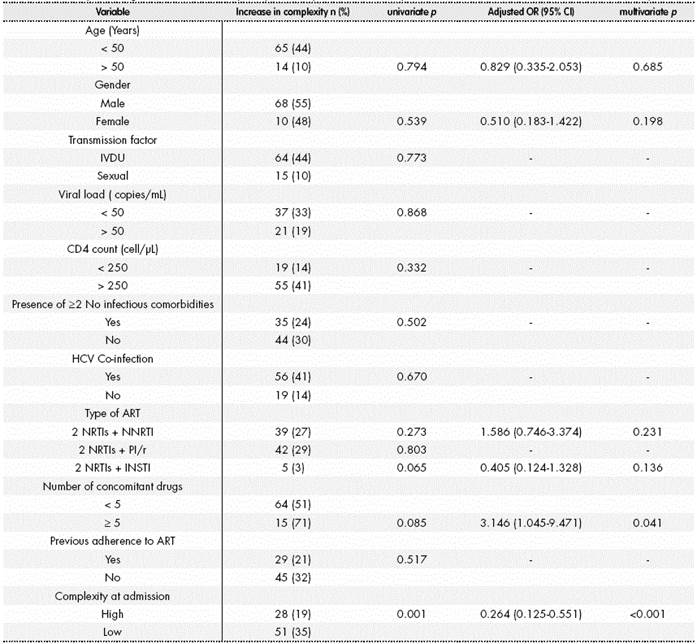
n: number of patients; OR: odds ratio; CI: confidence interval; IVDU: Intravenous Drug User; HCV: Hepatitis C virus; ART: antiretroviral treatment; NRTIs: nucleotide reverse transcriptase inhibitors; NNRTIs: non-nucleotide reverse transcriptase inhibitors: PI/r: boosted protease inhibitor; INSTI: integrase inhibitor.
Discussion
This study confirmed that after hospital admission there was an increase in pharmacotherapeutical complexity for HIV+ patients. Additionally, there was a reduction in adherence to antiretroviral treatment after these hospitalization episodes.
Different studies have analysed the modification in drug prescription after hospital admission in the overall population, particularly in elderly patients23-25. The study by Elliot et al.23 reviewed the impact of hospitalization on pharmacotherapy complexity for elderly patients in an Internal Medicine Unit. There was a 4-point increase in chronic medication complexity, and of 6.7 points in overall medication. In our case, the absolute difference was of approximately 2 points. This difference can be due to the disparity in age and comorbidities between the patients in both studies (mean age 45.3 vs. 79.7). Regarding the simplification strategies used in the pharmacy intervention, these were confirmed to be more effective for the reduction of complexity in patients with a low number of drugs at admission, and in those admitted to Specialized Geriatric Units. The study by Stange et al.26 analysed the evolution in pharmacotherapy complexity and adherence in >18-year-old patients with some chronic prescription for treating a cardiovascular or metabolic condition before, during and after admission. No significant differences were detected in any of these two parameters, though a positive trend was observed in adherence to medication. This can be due to the brief post-admission period (42 ± 7 days) taken, and the effect of recent hospitalization upon taking their medication.
Regarding the variation in pharmacotherapeutical adherence, the majority of studies point at the process of transition in care and hospital discharge as essential elements that can have a noticeable impact on this parameter27-29. In the study by Sengstock et al.27 the following are stated as factors that contribute to non-adherence: treatment failure after hospital discharge, and lack of education on the importance of treatment and its adverse effects by the hospital staff, as well as the lack of specific indications. Besides, the presence of polypharmacy and multiple doses taken daily will also play an important role, as well as the excessive cost of drugs. At this point, health-care education by healthcare professionals, particularly by the Pharmacist, who is an expert in medications, seems to be the key for an improvement in adherence after hospital admission.
On the other hand, only a limited number of studies have analyzed so far the complexity index and its impact on patient health outcomes. A relationship has been determined between an increase in complexity and the reduction of adherence in patients with cardiovascular disease, though the methodology for assessing complexity differs from the one used in this study30. The study by Jimenez et al.31 associated a higher complexity index with a worse compliance of the objectives proposed in HIV+ patients on treatment with lipid lowering medication. At the same time, the low adherence to lipid lowering treatment also had a negative impact on the objectives proposed.
It seems clear that the analysis and the reduction in pharmacotherapy complexity should be a priority for all types of patients, but particularly for HIV+ patients. Even though the complexity of treatments for this infection has been drastically reduced in recent years, HIV evolution and chronification has led to patients presenting increasingly more age-related comorbidities, and an increase in the number and complexity of their overall pharmacotherapy regimens. Some of the barriers analyzed for the implementation of simplification strategies at hospital discharge include lack of time by physicians and the low acceptance of the strategies proposed by the pharmacists involved32.
Finally, after analyzing the predictive factors associated with an increase in pharmacotherapy complexity after hospital admission, a high number of drugs prescribed before admission increased threefold the likelihood of higher complexity at hospital discharge.
The study by Montes et al.33 already described how the number of concomitant drugs was a factor predicting re-hospitalization in HIV patients, together with the number of previous admissions during that year, the use of drugs and/or alcohol, detectable viral load, or a CD4 lymphocytes count < 200 cell/µL.
Regarding the study limitations, one of the main ones is the retrospective and single-centre design of the study. The lack of digitalization of clinical records prevented the incorporation of patients admitted before 2006. Regardless of this, the sample size was sufficient, and the statistical tests applied in the multivariate analysis allowed to establish the validity of the statistical analysis with the population included in the study (the Hosmer-Lemeshow test (p = 0.815) indicates that results are valid and reliable). Moreover, the percentage of hospitalized patients and the treatments available for HIV+ patient management in previous years were radically different to the current ones.
Other aspect not assessed in the present study is the adherence to concomitant medication, and how this can be modified after hospital admission in the HIV population. Considering that HIV patients will typically present better adherence to antiretroviral treatment than to the rest of medications34, we could reach the hypothesis that the data for adherence to concomitant medication will be lower than those before admission. In order to confirm these facts, it will be necessary to conduct a prospective study to analyze the overall complexity and adherence of all medication, and the potential impact on HIV patients of incorporating a strategy based on information, education, and pharmacotherapy simplification at discharge, conducted by a multidisciplinary team.
Likewise, this study does not include an assessment of health outcomes derived of lack of adherence at medium-long term in this type of patients; this is an aspect that will be necessary to find out in future research.
In conclusion, overall pharmacotherapy complexity increased after hospital admission, and there was a parallel reduction in adherence to ART. Chronic treatment prescribed before admission was the only factor associated with an increase in complexity after admission.











 texto en
texto en