Introduction
Chronic lymphocytic leukaemia (CLL) is a lymphoproliferative disorder characterized by the expansion of mature-appearing CD5+ B cells in the peripheral blood, secondary lymphoid tissues, and bone marrow1. CLL is the most common form of leukaemia in adults in Western countries, with an estimated incidence of 4 to 5 cases per 100,000 population-years and a particularly significant prevalence in areas in which the population is older2. More than half of these patients have age-related comorbidities, such as hypertension, diabetes, osteoarthritis, or cardiorespiratory involvement3. The treatment decision is based on the presence or absence of adverse prognostic factors (deletion [17p], deletion [11q], TP53 mutation, IGHV mutational status) and on the functional status of the patient2.
In recent years, significant advances have been made in understanding the pathophysiology of CLL, and substantial progress has been made in the clinical management of the disease due to the identification of poor prognostic genetic variables, particularly those associated with chemoresistance and progression to highly aggressive forms of CLL4,5. Currently, chemoimmunotherapy is being displaced by biologic therapies, such as B-lymphocyte receptor inhibitors and BCL-2 inhibitors6,7.
Overexpression of BCL-2 contributes to the evasion of apoptosis, making tumour cells highly dependent on BCL-2 for their survival8. High expression of BCL-2 is observed uniformly across all CLL subtypes9.
Venetoclax, the first selective BCL-2 inhibitor, restores the ability of tumour cells to initiate the process of apoptosis and, administered together with obinutuzumab, has a complementary and synergistic mechanism of action that provides high efficacy rates and profound responses, with a fixed duration of 1 year of treatment5,10. In the CLL14 trial, 2-year progression-free survival (PFS) was 88.2% (95% confidence interval [CI]: 83.7%-92.6%) in patients treated with venetoclax in combination with obinutuzumab (VenO) vs 64.1% (95% CI: 83.7%-92.6%) in the control group treated with chlorambucil in combination with obinutuzumab (ClbO)5. After a median follow-up of 28.1 months, these results showed a slow-down in the risk of progression or death with VenO (hazard ratio [HR] = 0.35; 95% CI: 0.23-0.53; P < 0.001). At data cutoff, the results of overall survival (OS) were immature, with the median not having been reached in either group (less than 10% of events in each arm)5. These results were confirmed at the subsequent cutoff time, after a median follow-up of 39.6 months, where PFS was 81.9% in the VenO arm and 49.5% in the ClbO arm. These results showed a slow-down in the risk of progression or death with VenO (HR = 0.31; 95% CI: 0.22-0.44; P < 0.001)11.
The aim of this study was to conduct a cost-utility analysis to determine whether VenO, which is a therapy indicated for previously untreated patients with CLL, would be an efficient intervention within the Spanish National Health System (NHS) compared to the therapeutic alternatives available in Spain.
Methods
Study participants and comparators
The characteristics of the study population were matched to those of the patients included in the CLL14 Phase 3 clinical trial5 (i.e., patients with CLL who had not received prior treatment, 33% female, and a median age of 71.1 years).
At the time of study design, VenO was also compared to the most commonly used first-line alternative treatments in CLL patients: ClbO, fludarabine in combination with cyclophosphamide and rituximab (FCR), bendamustine in combination with rituximab (BR), and ibrutinib.
Type of análisis
It was estimated the mean cost and effectiveness per patient associated with each therapeutic alternative and calculated the incremental cost-utility ratio of VenO vs the other comparators to determine the additional cost of VenO to obtain 1 quality-adjusted life year (QALY).
The analysis was conducted from the perspective of the Spanish NHS, and included direct health care costs (updated to 2020 euros using the historical year-on-year consumer price index). The time horizon was extended to the patient's lifetime. An annual discount rate of 3% was applied to costs and clinical results12. The cost-effectiveness threshold was considered to be €25,000/QALY13.
The adaptation to the Spanish context was facilitated after consultation with an expert group selected based on their experience and knowledge of clinical practice. (i.e. the co-authors of the present study). After completing individual questionnaires, a base case was proposed for validation.
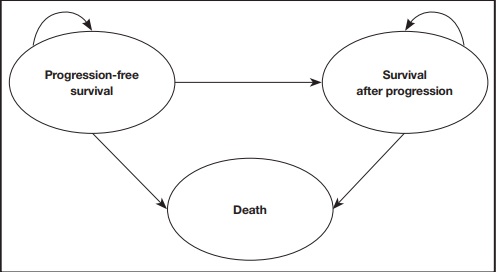
Structure of the model
A partitioned survival model14,15 was adapted to the Spanish setting. A model previously presented at the National Institute for Health and Clinical Excellence (NICE), and that simulated the evolution of patients with CLL who have not received previous treatment across different clinical situations (health states). Figure 1 shows a simplified schematic of the model, with three mutually exclusive health states: progression-free state, state after progression, and death. The proportion of patients who were alive for each cycle of the model (28-day cycles) was estimated from the area under the OS curve, and the proportion of patients who were alive free of progression was estimated from the area under the PFS curve. The proportion of patients who were alive after progression was estimated by the difference between the OS and PFS curves. The OS and PFS curves were estimated using parametric curves based on clinical evidence. To obtain the best estimate of the pharmacological cost, the model considered time-on-treatment information to measure discontinuation, which can occur due to adverse events (AEs) or disease progression. It should be noted that treatments with VenO, ClbO, FCR, and BR have a fixed duration, whereas the duration of treatment with ibrutinib is indefinite until disease progression or unacceptable toxicity. After discontinuation, patients were assumed to be able to receive subsequent treatments.
Clinical data
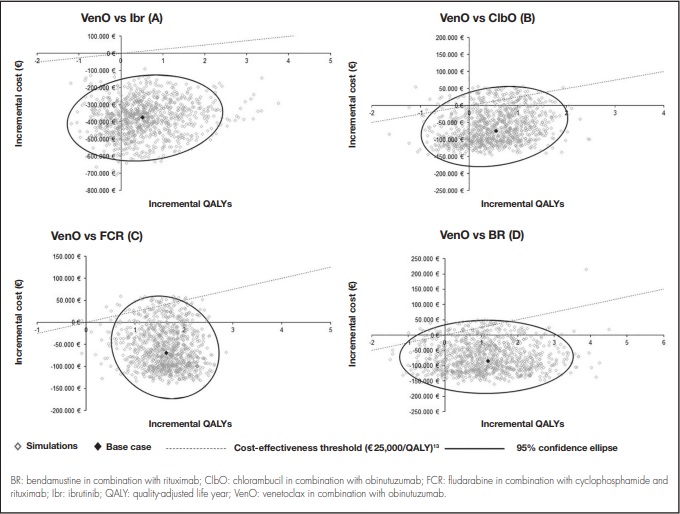
The efficacy data used in the VenO and ClbO model were derived from the CLL14 trial5. Because the study follow-up period was shorter than the horizon used in the economic studies (i.e. the recommended horizon being the patient's lifetime), the PFS, OS, and time-on-treatment curves had to be extrapolated using parametric distribution functions fitted to Kaplan-Meier (KM) curves. A goodness-of-fit criteria was followed in order to decide which parametric distribution was the best fit. This criteria described how well a given distribution fits a set of observations (KM curves). Specifically, the Akaike and Bayesian information criteria15 were followed (Appendix 1). The parameterized curves were adjusted according to the overall mortality of the Spanish population16, thus preventing the survival curves estimated in the model from being above the survival of the general population.
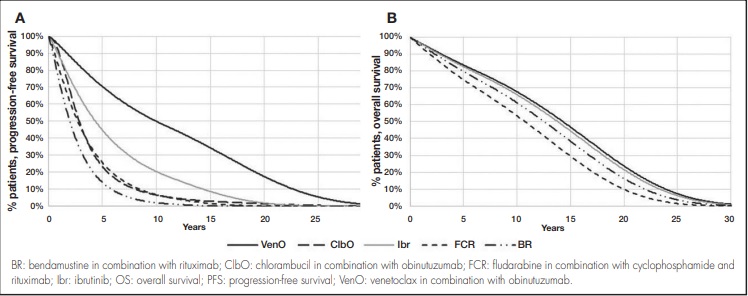
In the absence of direct evidence on ibrutinib, FCR, and BR as comparators compared to VenO, the parametric curves were estimated using HRs vs VenO (reference treatment). These were obtained from a Bayesian fixed-effect network meta-analysis17. This approach allowed an indirect comparison of VenO vs ibrutinib, FCR, or BR. To derive the PFS curve for ibrutinib, FCR and BR, it was assumed the corresponding HRs relative to VenO derived from the network meta-analysis. A log-logistic distribution for the PFS curve for VenO and ClbO was used (Figure 2A).
Regarding OS, it was assumed that there were no differences between VenO and ClbO based on the results of the CLL14 trial and corroborated by expert opinion. Thus, an exponential distribution was assumed for the purposes of extrapolation. To derive the OS curve for ibrutinib, FCR and BR, it was used the HRs relative to VenO derived from network meta-analyses (Figure 2B).
The analysis used time-on-treatment information to measure discontinuation. VenO, ClbO, FCR, and BR treatments have a fixed time duration (12 cycles for VenO and ClbO, 6 cycles for FCR and BR), whereas the duration of treatment with ibrutinib is considered to be indefinite until disease progression or unacceptable toxicity (a median of 60 months was assumed based on longer-term follow-up in the RESONATE-2 study, in which the median PFS was not reached4). After discontinuation, it was assumed that patients were able to receive subsequent treatments. For this purpose, a log-logistic distribution was assumed for VenO and ClbO, whereas the PFS curve was assumed for ibrutinib, FCR, and BR.
Quality of life
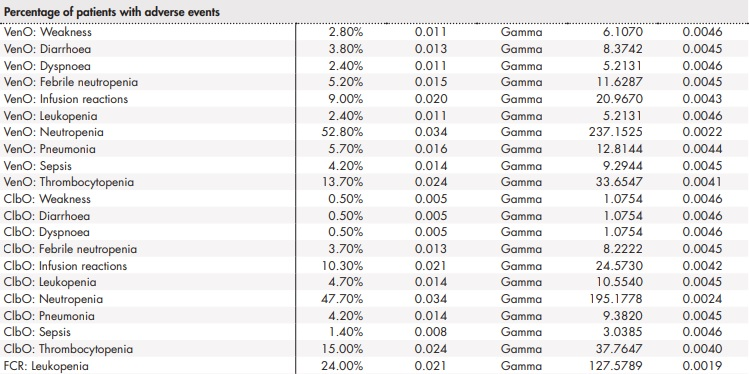
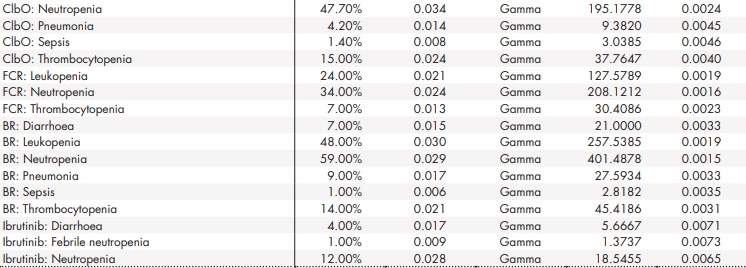
For the estimation of QALYs, different utility values were assumed depending on the health status of the patients. The utility values were used to represent the quality of life associated with a particular health status on a scale from 0 (death) to 1 (perfect health). Specifically, a utility of 0.80 was used for PFS health status (NICE TA174) and 0.68 for survival-after-progression status18,19. To represent the loss of utility (disutility) associated with increasing patient age, the defined utilities were adjusted by the utility according to the age of the general Spanish population derived from the Spanish National Health Survey (available from the Spanish National Institute of Statistics for 2011/12)20. The model also addressed disutility due to treatment-associated AEs. It was assumed that AEs, as well as their effects on quality of life and economic effects, occur in the first cycle of the analysis.
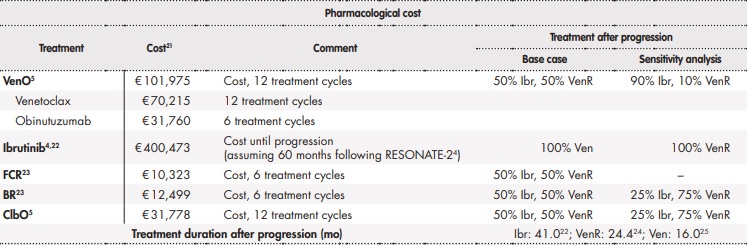
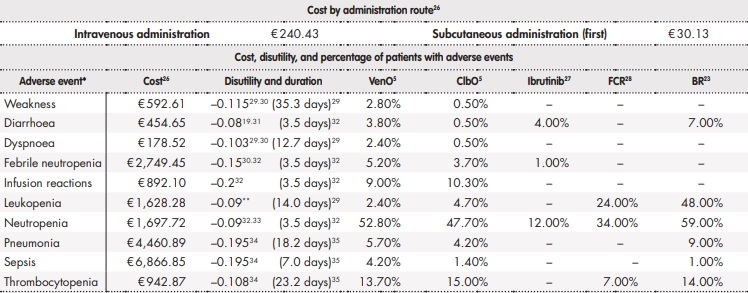
Resource use and costs
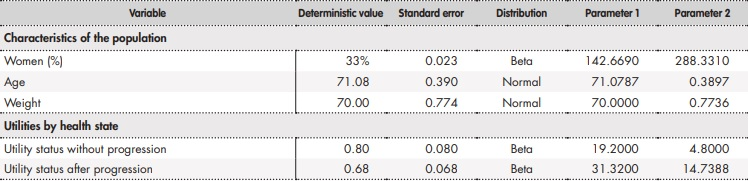
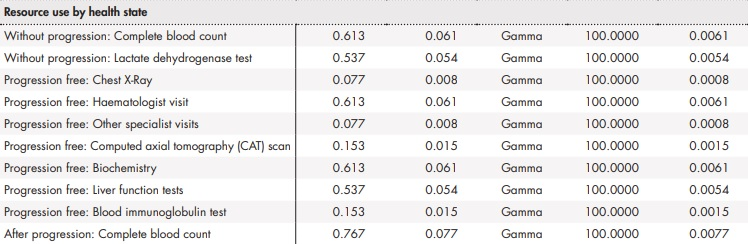
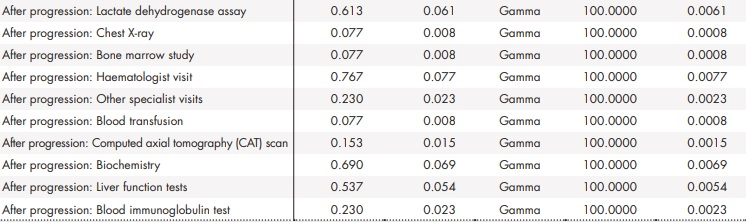
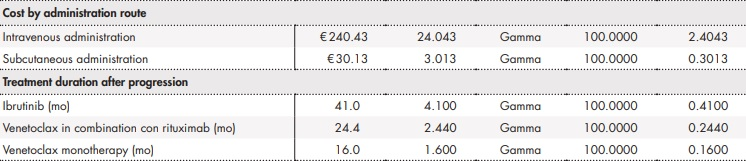
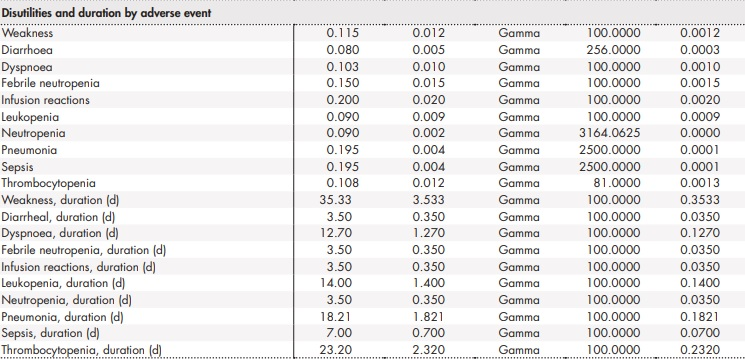
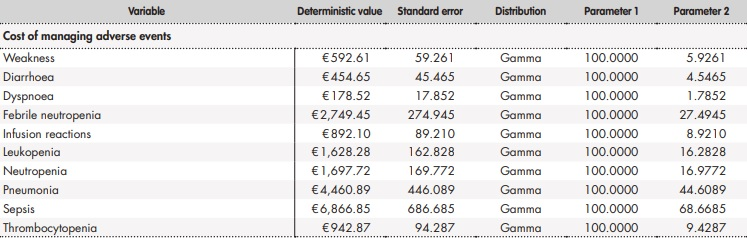
The analysis addressed the direct healthcare costs associated with the management of CLL (Table 1). The pharmacological cost, including treatments after progression, was calculated based on the laboratory selling price21. The use of resources and assumptions made were validated by clinical expert opinion.
Table 1 (cont.). Resource use and costs of analysis
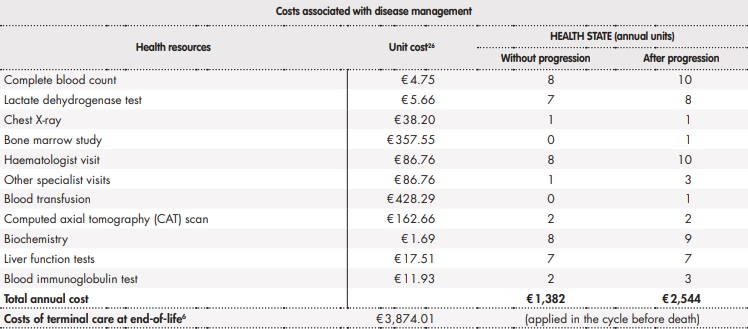
*Considered to be serious adverse events (neutropenia, febrile neutropenia, pneumonia, sepsis, and thrombocytopenia) and grade 3-4 with at least 2% difference between VenO and ClbO identified in the CLL14 study. Assumed to occur in the first cycle of the model.**Assumed neutropenia.BR: bendamustine in combination with rituximab; ClbO: chlorambucil in combination with obinutuzumab; FCR: fludarabine in combination with cyclophosphamide and rituximab; Ibr: ibrutinib; Ven: venetoclax; VenO: venetoclax in combination with obinutuzumab; VenR: venetoclax in combination rituximab.
Sensitivity analysis
Several sensitivity analyses were performed to assess the uncertainty of the variables used in the model and to determine the robustness of the base case results.
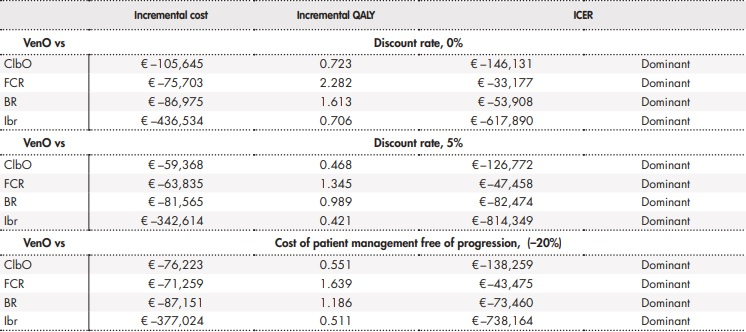
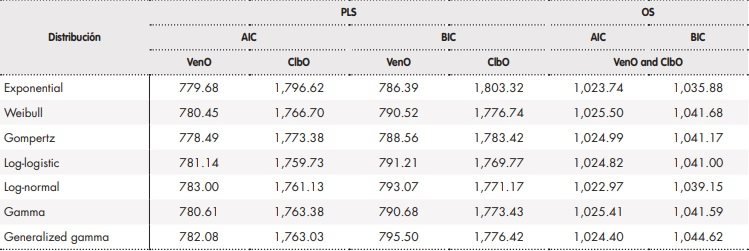
Firstly, results were obtained by varying the base case discount rate (0% and 5%).
Given the differences in resource use in patient management indicated by the clinical experts, the annual cost of patient management in both the progression-free state and after progression was varied by ±20%. Discrepancies were also noted regarding the distribution of subsequent treatments after disease progression for each alternative treatment, except in the case of FCR, where it remained the same (Table 1).
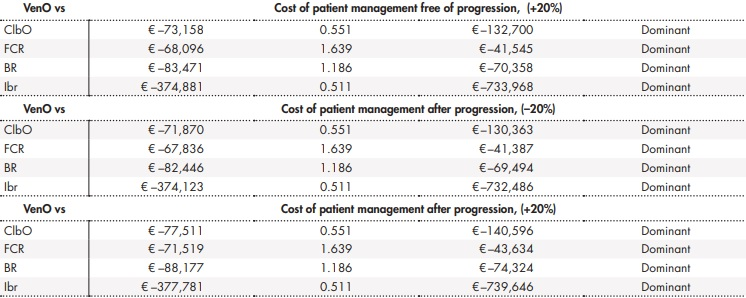
A probabilistic sensitivity analysis was also performed by simultaneously modifying the model parameters according to an established distribution (Appendix 2). Specifically, 1000 simulations were performed using the Monte-Carlo method36.
Results
The base case results showed that the costs per patient were lower and the gains in QALYs were greater with VenO than with other treatment alternatives (Table 2). In terms of economic assessment, VenO was the dominant alternative.
Table 2. Base case results
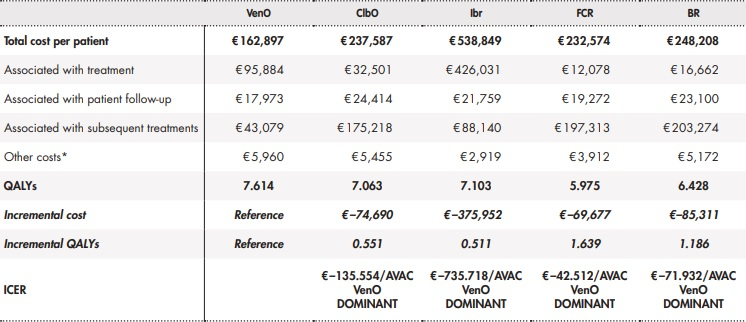
*Adverse events, end-of-life cost, tumour lysis syndrome prophylaxis.BR: bendamustine in combination with rituximab; ClbO: chlorambucil in combination with obinutuzumab; FCR: fludarabine in combination with cyclophosphamide and rituximab; Ibr: ibrutinib; ICER: incremental cost-effectiveness ratio; QALY: quality-adjusted life year; VenO: venetoclax in combination with obinutuzumab.
The lower cost of VenO vs ClbO, FCR, and BR was mainly due to a lower pharmacological cost of the subsequent treatments administered after progression. The lower cost of VenO vs ibrutinib as a comparator was mainly due to the shorter duration of time on treatment with VenO. The sensitivity analyses supported these results. Table 3 shows the results of the deterministic sensitivity analyses. The probabilistic sensitivity analysis showed that 68% to 85% of the simulations performed identified VenO as the dominant alternative, with lower costs and more QALYs gained (Figure 3).
Table 3 (cont.). Results of the deterministic sensitivity analysis
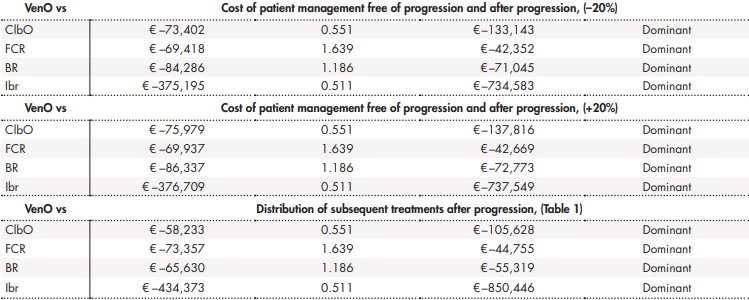
BR: bendamustine in combination with rituximab; ClbO: chlorambucil in combination with obinutuzumab; FCR: fludarabine in combination with cyclophosphamide and rituximab; Ibr: ibrutinib; ICER: incremental cost-effectiveness ratio; QALY: quality-adjusted life year; VenO: venetoclax in combination with obinutuzumab.
Discussion
This study assessed the efficiency of VenO in the Spanish setting as a treatment for CLL in previously untreated patients against comparators that are commonly used in clinical practice and are indicated for such pathology. The results of this analysis were presented at the LXII National Congress of the Spanish Society of Haematology and Chemotherapy (SEHH) and at the XXXVI National Congress of the Spanish Society of Thrombosis and Haemostasis (SETH)37.
The modelled population was based on the CLL14 trial population, which included patients with unfavourable cytogenetic prognosis (including patients with 17p deletion and TP53 mutation). It is noteworthy that these patients were not excluded from the baseline study population, what can make the study population more representative of the real clinical practice. The pivotal ibrutinib trial, RESONATE-24, excluded patients with 17p deletion, which was thus a methodological limitation of the study design.
In the present study, VenO was considered to be the dominant alternative to all comparators because of the increased number of QALYs obtained and lower cost per patient. These results are mainly due to VenO achieving greater PFS due to its increased effectiveness and its lower pharmacological costs. The cost of using VenO was substantially lower than that of ibrutinib because VenO has a fixed treatment duration of 1 year, whereas ibrutinib has an indefinite treatment duration until disease progression or unacceptable toxicity (a median treatment duration of 60 months was assumed based on the RESONATE-24 study, in which the median PFS was not reached). This is also particularly relevant from a budgetary point of view because, in addition to being efficient, the VenO combination can generate savings in pharmaceutical expenditures (the pharmacological cost of treatment per patient is €101,975 with VenO compared to €400,473 with ibrutinib)38, while providing budgetary predictability due to the fixed duration of treatment. Compared to the other comparators, VenO has lower treatment costs after disease progression. This lower cost is due to the high rates of deep response achieved with VenO. Deep response is understood as the achievement of complete remission and undetectable minimal residual disease, which avoids or delays the initiation of a second line of treatment11. Costs related to patient follow-up are also lower with VenO tan with the other alternatives because the patient remains longer in progression-free and treatment-free states.
Several cost-effectiveness studies on CLL in previously untreated patients have been conducted in other countries, but most of these studies were conducted prior to the approval of VenO and none have used this therapy as a comparator.
Soini et al. (2016) studied the cost-effectiveness of first-line treatments for CLL in patients ineligible for full-dose fludarabine39. The most cost-effective treatment was ClbO vs the other alternatives studied, such as chlorambucil in combination with ofatumumab, chlorambucil in combination with rituximab, and BR.
Furthermore, after the approval of ibrutinib, several studies conducted in other countries conducted economic analyses on its efficiency as first-line treatment for CLL40-42. Although the results of these studies are not directly applicable to Spain, all of them seem to agree that ibrutinib offers reasonable results in terms of PFS and QALYs, but it is not considered to be cost-effective.
Due to the type of analysis, the present study is limited by the need to extrapolate survival data to a longer-term horizon than the trial follow-up period. However, the extrapolation was based on the distributions with the best goodness-of-fit to the KM curves in the CLL study14. It would be relevant to perform additional analyses when longer-term CLL14 study follow-up data are obtained or to conduct real-world evidence studies.
On the other hand, in the absence of direct evidence related to the other comparators, except for ClbO5, an indirect comparison was performed by means of a network meta-analysis. This type of analysis is not free of limitations, which are mainly at the level of methodological similarity (i.e. heterogeneity between studies). Nevertheless, it is the only possible alternative in order to be able to compare treatments that have not been directly compared in clinical trials. Other limitations are the differences in methodology and the patient selection procedure between the clinical trials chosen for each treatment. To increase the external validity of this type of analysis, all pivotal clinical trials for CLL treatments should include the same type of patients (not excluding those with unfavourable prognosis) and demonstrate efficacy and safety data over the same time horizon. At the time the CLL14 study was designed, ClbO was the standard treatment for this type of patient, although currently ibrutinib is considered to be the standard treatment for previously untreated CLL patients with the 17p deletion or TP53 mutation.
In conclusion, this study shows that VenO is emerging as an efficient and dominant alternative for the treatment of CLL in previously untreated patients in Spain. According to our analysis, the introduction of VenO in the Spanish NHS could reduce treatment costs, costs associated with patient follow-up, and the costs of subsequent treatments after progression, as well as improve the life expectancy and quality of life of Spanish patients with CLL.











 texto en
texto en