Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pediatría Atención Primaria
versión impresa ISSN 1139-7632
Rev Pediatr Aten Primaria vol.13 supl.21 Madrid dic. 2011
https://dx.doi.org/10.4321/S1139-76322011000500001
What medical professional is the most adequate, in developed countries, to provide health care to children in primary care? Systematic review
Buñuel Álvarez J.C.a, García Vera C.b, González Rodríguez P.c, Aparicio Rodrigo M.d, Barroso Espadero D.e, Cortés Marina R.B.f, Cuervo Valdés J.J.g, Esparza Olcina M.J.h, Juanes de Toledo B.i, Martín Muñoz P.j, Montón Álvarez J.L.k, Perdikidis Oliveri L.l, Ruiz-Canela Cáceres J.m
aPediatrician. ABS Girona-4. Girona;
bPediatrician. CS Sagasta-Ruiseñores. Instituto Aragonés de Ciencias de la Salud (Aragonese Institute of Health Sciences). Zaragoza;
cPediatrician. CS Manzanares El Real. Madrid;
dPediatrician. CS Entrevías. Madrid;
ePediatrician. CS Don Benito. Badajoz;
fPediatrician. ABS Girona-3. Girona;
gPediatrician. CS Urbano I. Mérida, Badajoz;
hPediatrician. CS Barcelona. Servicio Madrileño de Salud (Health Service of the Autonomous Community of Madrid). Móstoles, Madrid;
iPediatrician. CS El Espinillo. Madrid;
jPediatrician. Unidad de Gestión Clínica La Plata/Palmete. Sevilla;
kPediatrician. CS Mar Báltico. Madrid;
lPediatrician. CS Los Fresnos. Torrejón de Ardoz, Madrid;
mPediatrician. Distrito Sanitario de Sevilla (Sevilla Health District). Sevilla. Spain.
Conflict of Interest: All the authors of this revision are members of the Grupo de Trabajo de Pediatría Basada en la Evidencia (Evindece-based Pediatrics Work Group) that belongs to the Asociación Española de Pediatría de Atención Primaria (AEPap / Primary Care Pediatrics Spanish Association) and to the Asociación Española de Pediatría (AEP / Spanish Association of Pediatrics).
Funding: financial resources provided by the "Pediatría y Salud" Foundation (Madrid / Spain).
ABSTRACT
Introduction: There is controversy about which health professional is the most adequate -pediatricians (PED) or family practitioners/general physicians (FP/GP)- to provide health care services to children and adolescents in Primary Care (PC). There are not previous systematic reviews approaching this subject in the previously published literature. The objective of this study is to compare health care provided between PED and FP/GP in the following aspects of the clinical practice: antibiotic (ATB) prescription; diagnostic test indication; management of acute otitis media (AOM), asthma, febrile syndrome, and several psychopathological conditions, and preventive measures accomplishment.
Material and methods: Study design: Systematic review. Data sources: MEDLINE and CENTRAL databases, TRIP Database and Google Scholar, were searched until December 2008 to retrieve original papers and systematic reviews comparing the clinical practice of both kinds of health professionals. No language restriction was made. Study selection: studies of any kind of design were included (cross-sectional, cohort, case-control and experimental) comparing the clinical practice of PED and FP/GP. The references without original research were excluded (letters to the editor, editorials). The methodological quality of each study was assessed with the tool "OSTEBA; Critical Appraisal Cards". Two reviewers assessed the quality of the studies independently, achieving consensus in case of discrepancy. Seven pairs of reviewers made the data extraction independently. Discrepancies were achieved by consensus.
Results: On average, FP/GP prescribed more ATB than PED in upper respiratory tract infections of probable viral etiology -odds ratio (OR): 1.4; 95% confidence interval (95% CI): 1.1-1.8-; PED were more likely to adhere to clinical guidelines recommendations on febrile syndrome management (OR: 9; 95% CI: 3-25) and on attention deficit disorder with/without hyperactivity (OR: 5; 95% CI: 3-11), and showed more resolution capacity on other highly prevalent conditions in children and adolescents (such as asthma and AOM). PED showed higher vaccination coverage than FP/GP in all the studies assessing this result.
Conclusion: Based on the presented results, it seems reasonable to recommend maintaining the PED figure in PC health centers and reinforcing its specific role as the first point of contact of the child with the health care system.
Key words: Pediatrics. Family practice. Physicians. Family. Interprofessional relations. Primary Health Care.
CS: Centro de Salud (Public Health Center of Primary Care). ABS: Áreas Básicas de Salud (Basic administrative areas of the Public Health Administration in certain places in Spain).
EXTENDED ABSTRACT
Introduction
There is a controversy about which health professional is the most adequate -pediatricians (PED) or family practitioners/general physicians (FP/GP)- to provide health care services to children and adolescents in Primary Care (PC). There are few studies with the purpose of comparing directly the clinical practice of both professionals. Up to now, there are not previous systematic reviews addressing this subject. The question is important because several studies have established some differences in knowledge, as well as in skills and attitudes, among PED and MF/MG in the field of child and adolescent health care.
In the USA, there is a trend towards children being attended by PEDs in Primary Care (the number of children attended by PED in the period between 1980 to 2000 increased from 56.2% to 64.2%, while children attended by GPs decreased from 33.7% to 23.9%). In Europe, it has been suggested that primary health cares for children, provided by PED, is associated with a decrease in mortality.
With the aim of adding insight into this question, and because no systematic review has been published about this issue, we conducted this study, with the goal of comparing the healthcare delivered by PED and FM/GP in the following issues of clinical practice: 1) Antibiotic (ATB) prescription; 2) Adequacy in the ordering of diagnostic tests 3) Management of otitis media; 4) Management of asthma; 5) Fever; 6) Psychological problems; 7) Clinical preventive services.
Material and methods
Study design
Systematic review. Data sources: the following databases were searched: MEDLINE, the Cochrane Central Register of Controlled Trials (CENTRAL), TRIP Database and Google Scholar. They were searched until December 2008 to retrieve original papers and systematic reviews comparing the clinical practice of both types of health professionals. No language restrictions were applied.
Study selection
Studies of any type of design were included (cross-sectional, cohort, case-control and experimental) if they were specifically designed to compare the clinical practice of PED and FP/GP. Those references, which were not original research, were excluded (letters to the editor or editorials).
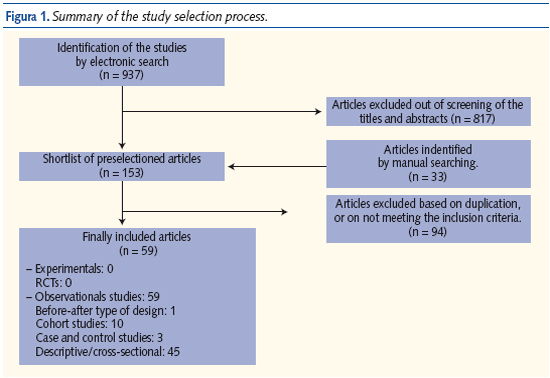
We selected 59 publications (1 investigation with a before-after study design, 10 cohort studies, 3 cases-control studies, and 45 transversal studies).
The methodological quality of each study was assessed with the tool "OSTEBA tool; Critical Appraisal Cards". Two reviewers independently assessed the quality of studies for inclusion, and the discrepancies were resolved by consensus. Seven pairs of reviewers made the data extraction independently, using a form specifically designed for the task. Disagreements were resolved by consensus.
Statistical analysis
We calculated some estimators, whenever it was possible from the results of each study (if they were not already provided by the authors). Those estimators were the following: relative risk, odds ratio, and prevalence ratio (RP/PR), with their respective 95% confidence intervals (95% CI).
When possible, we calculated the global effect size resulting from combining the outcomes by means of using a global combined estimator: the combined OR, estimated by the inverse variance method.
The presence and degree of heterogeneity was assessed by means of the Cochran's Q. Fixed effects model or random effects model were used if the data were homogeneous or heterogeneous, respectively.
Results
On average, FP/GP prescribed more ATB than PED in upper respiratory tract infections of probable viral etiology (OR: 1.4; confidence interval; 95% CI: 1.1-1.8). PEDs were more likely to adhere to clinical guidelines recommendations on febrile syndrome management (OR: 9; 95% CI: 3-25) and on attention deficit disorder with/without hyperactivity (OR: 5; 95% CI: 3-11). Pediatricians showed, as well, more resolution capacity on other highly prevalent conditions in children and adolescents, such as asthma and acute otitis media (AOM). PED showed higher vaccination coverage than FP/GP in all the studies assessing this result.
In cardiovascular prevention the interventions related to prevention of tobacco consumption and to increasing physical exercise were better accomplished by FP/GP. Obesity screening and treatment, hypercholesterolemia screening, and blood pressure measurement were more frequently accomplished by PEDs.
In preventive activities, PEDs were more active than GPs in counselling about preventing accidents, preventing intoxications and preventing rickets, and were less active in preventive activities about toxic consumption.
Finally, the use of a diagnostic test in primary care was better performed by PEDs. They ordered fewer chest X-rays motivated by suspicion of pneumonia [Risk Difference (RD) PED vs. GP: -6.90; 95% CI: -8.80 to -4.90]; more blood test in the young infant with fever (RD PED vs. GP: 12.50; 95% CI: 10.00 to 14.30); and more diagnostic test for streptococcal throat infection in sore throat (OR GP/FP vs. PED: 0.46; 95% CI: 0.32 to 0.66). Furthermore, when an x-ray was carried out, the probability of finding an abnormal result was higher among those ordered by PEDs than among those ordered by GPs (RR: 2.6; 95% CI: 1.1 to 6.6).
Conclusions
This is the first systematic review (SR) comparing clinical practice between PEDs and GPs/FPs in primary health care. The main conclusion is that in developed countries, primary health care delivered by PEDs, result in better immunization practices and better compliance with guidelines of frequent diseases than those delivered by GPs/FPs.
The variables studied (drugs prescription, compliance with guidelines recommendations, vaccination coverage, and a decrease in rates of referral to secondary health care) are also of great importance for doctors, patients and health managers, because small variations in the way in that those cares are delivered can result in a major modification of the health outcomes obtained, with the corresponding important implications of this fact in terms of health or otherwise.
In view of these results, it seems reasonable to keep the PED in the primary health care level and to reinforce it specific role as the first point of contact of the child with the health care system.
Introduction
There is a wide variation between developed countries regarding the care of children and adolescents at the primary care level. Differences in the pattern of pediatric primary care (PPC) have been reported, with three different healthcare delivery systems: pediatrician (PED) based, general practitioner (GP) or family practitioner (FP) based, and combined services. Although it has also been recognized that differences in the financing of health care systems (models based in medical insurance subscription, models consisting in health system funded by taxes, or free market) contribute to these variations. In those countries where patients choose their primary care physician, there is a clear trend over time to choose a PED, especially in urban areas, which could probably be due to the shortage of specialists in rural areas.1-5
In 1981 Fishbane et al.2 described that in the USA, PEDs provided more routine preventive care in all age groups than GPs, and that they made more additional diagnoses in children seen during these latter type of care. In 1985 a study of Starfield,5 described that PEDs saw more very young children and fewer adolescents than did GP. PED did more rapid diagnosis tests of group A streptococcal pharyngitis in children, ordered more diagnostic tests, had better immunization coverage and prescribed fewer drugs, but did less education about sexual health and family problems, and also performed less minor surgery interventions.
A study in 2004 in the USA3 described that the number of patients younger than 18 years visited by a primary care PED increased from 56.2% to 64.2% in the period of 1980 to 2000, while those visited by a FP or GP decreased from 33.7% to 23.9%. The number of adolescents visited by PED increased from 26.3% to 37.4%, and the number of adolescents visited by FP o GP decreased from 51% to 40.4%.
In 2006 a new publication4 confirmed this trend in the USA and stated that children with no insurance or public insurance were significantly more likely to have a not PED provider of health care [Odds ratio (OR): 1.64 and 1.23 respectively] than children with private insurance (OR: 0.76).
In Europe little information has been available on which professional is the most appropriate for delivering health cares to children in primary care. Katz6 found out that infant mortality rate in European countries decreased 5.4/1,000 when pediatric primary care was provided by PED, compared with other systems. Another factor significantly associated with infant mortality rate was the income per capita, being lower in countries with a higher income per capita: for every increase of € 1,000 in income per capita, there was a decrease of 0.711/1,000 in the infant mortality rate.
Surprisingly there are few studies related to this issue, especially in public health and more in those countries, like Spain, where the PPC model is a PED-based system.7 In order to clarify which health professional is the most appropriate to deliver health care to children and adolescents, in developed countries, we designed this systematic review (SR). The aim of this SR is to compare the clinical practice between PED and FP/GP in providing health care to children and adolescents at the primary health-care level.
Material and methods
Selection criteria
Types of studies: Studies of any type of design were considered: (these included cross-sectional, prospective cohort, case-control, and experimental studies) as long as they were specifically designed to compare the clinical practice of PED and FP/GP. Those references found, but not corresponding to original research papers, were excluded (letters to the editor or editorials).
Types of participants: PED, FP and GP who developed their clinical practice in PC and hospital emergency departments.
Types of outcome measures:
1. Antibiotic prescription (ATB) in respiratory tract infections (RI) of probable viral etiology.
2. Otitis media treatment.
3. Management of asthma in children.
4. Management of fever in children.
5. Management of children with psychiatric disorders, like depression, obsessive compulsive disorder (OCD), attention deficit hyperactivity disorder (ADHD).
6. Immunizations: attitudes, beliefs, coverage and implementation of the official immunization schedules.
7. Cardiovascular prevention.
8. Other preventive activities.
9. Use of diagnostic tests.
Search methods for identification of studies
Data sources: MEDLINE, and Cochrane Central Register of Controlled Trials (CENTRAL) databases, TRIP Database and Google Scholar. They were searched until December 2008 to retrieve original papers and systematic reviews comparing the clinical practice of both types of health professionals. No language restrictions were applied. And no restriction, either, was applied to the search by date (other than the limit of the searching date: December 2008).
Subject index terms:
- Related to the health care provider: "pediatrics", "family practice", "physicians, family", "interpersonal relations".
- Related to health policy: "primary health care", "ambulatory care", "health services", "child health services", "emergency services, hospital", "preventive health services", "personal health services", "delivery of health care", "health care sector", "health care surveys", "health care reform", "health care costs", "process assessment (health care)", "outcome assessment (health care)", "quality assurance, health care", "patient acceptance of health care", "health care rationing", "quality of health care", "health care facilities, manpower, and services", "quality indicators, health care", "health care quality, access, and evaluation", "outcome and process assessment (health care)", "united states agency for healthcare research and quality", "health services research", "health services accessibility", "community health services", "urban health services" [MeSH], "rural health services" [MeSH], "maternal-child health centers" [MeSH], "health services administration" [MeSH], "geographic locations" [MeSH], "community health centers", "utilization review", "medical audit", "guideline adherence", "process assessment (health care)", "quality indicators, health care", "physician's practice patterns", "inappropriate", "appropriate", "appropriateness".
- Related to the outcomes: "respiratory tract infections", "otitis media", "asthma", "fever", "depression", "attention deficit disorder with hyperactivity", "obsessive-compulsive disorder", "immunization", "vaccination", "primary prevention", "secondary prevention", "tertiary prevention", "obesity", "overweight", "anti-bacterial agents", "depressive disorder", "common cold", "nocturnal enuresis", "child nutrition sciences", "dental caries", "dermatitis, atopic", "breastfeeding", "vaccines", "smoking", "tobacco use cessation", "tobacco", "sudden infant death".
- As subheadings were used the following: "drug therapy", "diet therapy", "therapy", "therapeutic use", "prevention and control", "diagnosis", "mortality", "complications", "drug effects", "economics".
The Spanish equivalents to the search terms were also used to retrieve additional publications in Google Scholar. We reviewed the references of the retrieved publications to obtain additional relevant articles.
Methods of the review
Study selection: Two reviewers (JCB and CGV) independently assessed eligibility of the studies identified by examining titles and abstracts. From those articles found interesting, the full article was obtained. Disagreements were resolved by consensus.
The selection process is shown in Figure 1. Fifty nine studies were included in the review (one before-and-after study, ten cohort studies, three case-control studies and 45 cross-sectional studies).
Data extraction and assessment of the methodological quality: The included studies were distributed to seven pairs or reviewers. Each of them independently extracted the data and assessed the methodological quality of each study.
Disagreements were resolved by consensus among them. If not possible, JCB and CGV resolved it.
The methodological quality of each study was assessed with the tool "OSTEBA; Critical Appraisal Cards" (OSTEBA: Osasun Teknologien Ebakuazioa-Evaluación de Tecnologías Sanitarias del País Vasco = Healthcare Technology Evaluation of the Basque Country): www.osanet.euskadi.net/r85-osteba/es/contenidos/informacion/osteba_formacion/es_osteba/osteba_fichas_critica.html
This program assigns three degrees of quality: low, medium and high. In the couples who assessed the methodological quality, each evaluator extracted the data independently. Any disagreements were resolved by consensus. If this was not possible, JCB and CGV made the final decision.
Extracted data were: first author, year of publication, journal, country, type of design, sample size, type of provider (PED, FP, GP), number of losses across the study and reason for them, main outcome variable (that always included a direct comparison between PED and FP/GP relative to a specific aspect of health care in children and adolescents) and the effect estimators.
Statistical analysis
Whenever this was possible, and based on the results of every individual study, the following estimators of effect were calculated (if they were not already offered by the authors in the papers): relative risk (RR) for cohort studies, OR in case control studies, and prevalence ratio (PR) in cross sectional studies. Confidence intervals (95% CI) were also calculated for each estimator.
Results of the studies were combined when possible by means of a global combined estimator (OR), using the method of the inverse of the variance, and applying either a fixed effects model, or a random effects model, depending on the presence or not of statistical heterogeneity. Statistical heterogeneity was estimated by means of the Cochrane´s Q test (a value of < 0.1 is suggestive of heterogeneity) and by means of the I2. The possibility of publication bias was evaluated by the Begg method.
Results
Antibiotic use in respiratory tract infections of probable viral origin
The most important characteristics of the studies that evaluated these aspects are described in Table 1.
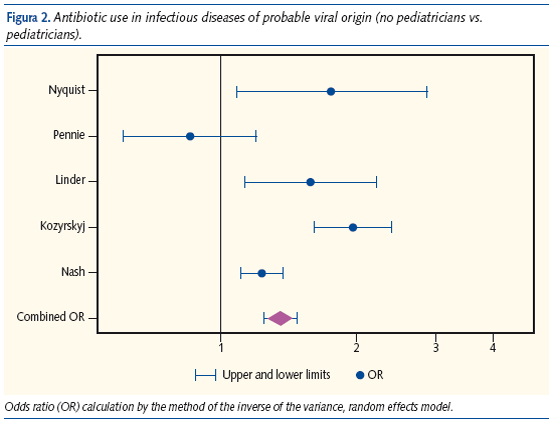
Studies conducted by means of consulting population-based databases
With the purpose of determine the association between type of professional and antibiotic prescription for URI (upper respiratory infection) of probable viral origin, data were combined from those studies which met the following requirements: 1) information extracted from registers of databases for health care in which diagnosis and treatment were indicated; 2) studies with design compatible with historical cohort; 3) studies located in primary care. These criteria were met by seven studies.8-14 One13 of the studies was excluded because the data came from another included study.12 Another one was excluded because it researched antibiotic (ATB) use in a non-infectious disease (asthma).14 For the combination of the results, a random effects model was used, due to the presence of heterogeneity (Q= 25.7, P = 0.00004, I2 = 84.4). Analysis of the publication bias could not be undertaken because the number of the studies in the meta-analysis was small. The combined OR was 1.41 (95% CI: 1.07-1.8) and indicated that those primary care doctors, who were not pediatricians, had a mean of 1.4 times more probability of prescribing ATB for URI of probable viral etiology in comparison to PED (Figure 2). The results of other studies that used population databases could not be combined because of differences in the methodology. These studies and their results are described individually in the following paragraphs:
Mainous et al.15 analyzed the registers from the Medicaid database in Kentucky (USA) between the first of July 1995 and the 30th of June of 1996. There were 34,624 episodes of URIs, (for the definition they used the code 460, and all the codes under stem 465 in the international classification of Diseases, 9th Revision, Clinical Modification/ICD-9-CM) in persons under 18 years of age. To be included in the study doctors had to have treated at least 25 URIs during the study period. For one of the outcome variable, it was established the definition of "high prescription" when the proportion of URIs treated with ATB was greater than the 75th percentile. Fifty-two doctors were considered high prescribers (they had attended 11,899 episodes of URI). Low prescription was considered for doctors who prescribed antibiotics in a proportion inferior to the 25th percentile. This criterion was met by 55 doctors who had attended 5,396 episodes of URIs. Family doctors had a higher probability of being high prescribers of ATB in comparison to pediatricians (OR 409; 95 % CI: 29-7,276).
Kozyrsky et al.14 examined, in the year 2006, trends and determinants in the use of ATB prescription for acute wheezing episodes in a population of children whit asthma. The treatment recommendation, in use at the moment of the study from a CPG, was not to treat with ATB children with acute asthma. The sources for the data for this investigation were obtained from the population-based health care administrative and prescription databases of the Manitoba Health Services Insurance Plan (MHSIP. Manitoba/Canada), which represent all encounters of every Manitoban with the health care system. The consultation targeted data that were available for the following period: fiscal year (FY) 1996 to FY2000.
The primary outcome was dispensing of an antibiotic prescription within two days after an ambulatory physician visit for a wheezing episode in children with asthma. GPs prescribed antibiotics in the 29.3 % of the 20,821 wheezing visits that they attended, versus 15.5 % of PEDs (of a total of 9,855 wheezing visits attended). Therefore GPs prescribed ATB more frequently than PEDs (OR: 2.10; 95% CI: 1.82-2.53).
Hare et al.13 reviewed the data base of the National Ambulatory Medical Care Survey (NAMCS) in USA, between 1993 and 2003, to analyze the patterns of prescription in children < 18 years of age with viral RTI. Non pediatrician doctors prescribed ATB more frequently than PEDs (OR: 1.48; 95% CI: 1.05-2.07).
Boquet et al.16 compared diverse aspects of medical practice of PEDs vs. FPs/GPs during a two year period of time (between January 2001 to December 2002) in the French region of the Franche-Comté. Overall, PEDs prescribed ATB less frequently in comparison to FPs/GPs and, when looking at the type of antibiotic, children seen by pediatricians took: 24.9 % less penicillin, 73.9 % less cephalosporins and 52.9% less macrolides.
Starfield et al.5 and Fishbane et al.2 also studied prescription based on type of professional, researching population-based databases in the USA. They found that PEDs prescribed fewer antibiotics, but did not indicate the numerical data.
Cross sectional studies based on professional surveys
Six studies evaluated the prescription habits by means, in general, of self reported mail surveys.17-22 The fact that there was a big proportion of non-responders (in some cases up to 50%) and the absence of an analysis of the characteristics of these non responders, make it advisable to describe the results of theses studies separately.
Roark et al.17 sent a survey to a random sample of 250 FPs and 175 PEDs in the state of Colorado (USA), on the therapeutic-diagnostic attitude facing two hypothetical case scenarios: a 13 month old child with asymptomatic and persistent otitis media with effusion (OME), and a child of 15 months of age with recurrent otitis media (ROM). 142 FPs answered (57%) and 114 PEDs (65%). In comparison with PEDs, FPs had a greater probability of prescribing high cost ATB [Prevalence ratio (RP): 1.51; 95% CI: 1.14-1.99]. There were no differences between both types of professional in the case of ROM.
Schwartz et al.18 sent a survey to a sample of 450 primary care doctors selected from the registers of five counties in northern Virginia (USA). The study does not indicate whether the sample were randomly selected, but it is possible to deduce that it was sent to all the professionals that were in active and dedicated at least 25% of their working time to visit infants and small children. The purpose of the study was to compare the diagnostic-therapeutic attitude of PEDs and FPs in dealing with children with acute purulent rhinitis. The instrument to assess this question was a questionnaire containing two clinical vignettes, representing two clinical scenarios: a child of 10 months of age and another of 6 years of age. 346 doctors answered the survey (77%): 201 of those responders were PEDs and 145 FPs. In the first scenario (10 month old child), the FPs were more likely to immediately prescribe an ATB than were the PEDs (71.1% vs. 53.5 %; RP: 1.33; 95% CI: 1.12-1.57). PEDs adopted an expectant attitude for 7-10 days without ATB after diagnosis more frequently (22.7%) than FPs (14.8%), even though the results were not statistically significant (RP: 0.65; 95% CI: 0.41-1.04). The decision of not to prescribe ATB in any case was also more frequent for PEDs (11.1% vs. 3.5 %; RP 0.32; 95% CI: 0.12-0.82). In the second scenario FPs prescribed ATB with higher frequency (RP 2.08; 95% CI: 1.54-2.8). The decision to never prescribe ATB was more frequent for PEDs (19.6%) than for FPs (5%) (RP 0.25; 95% CI: 0.12-0.55).
Davy et al.19 sent a survey to a random sample of 181 primary care practitioners (family physicians and pediatricians) in Toronto (Canada) with the purpose of determining the variability of self-reported habits of antibiotics prescription for children with undifferentiated acute respiratory tract infection with cough (UARTIC). 63 out of 98 PEDs answered (64%) and 73 out of 83 FPs (88%). FPs had a higher probability of prescribing ATB in case of a 3-day history of UARTIC (RP 1.38; 95% CI: 1.05-1.81), after three days of evolution and tending to worsen (RP: 2.05; 95 % CI: 1.19-3.53), after two weeks of evolution (RP: 2,29; 95% CI: 0.96-5.44) and after two weeks of evolution an a tendency to worsen (RP: 1.65; 95% CI: 1.12-2.36).
Watson et al.20 sent a survey by mail to find out the attitude of professionals in relation to recently published recommendations on the management of upper respiratory infections (URIs). The sample was obtained by a random method, from the list of PEDs and FPs that worked in Georgia (USA). Of 846 interviews sent, 366 were answered (43.3%): 154 FPs and 212 PEDs. For the treatment of common cold, the probability of receiving ATB was higher when the child was attended by a FP (57.8% vs. 30.2%; RP 1.91; 95% CI: 1.50-2.45).
Arnold et al.21, in the year 2005, sent a mail survey in Ontario (Canada) to a sample of 540 PEDs and FPs selected by means of a quasi random method, using a list of doctors taken from the Southam Medical Lists. The purpose was to determine the influence that the characteristics of disease (URIs), patients, and type of physicians have on the antibiotic prescribing habits of the doctors. 257 doctors answered (48%) of which 119 (47.6%) were FPs and 131 (52.4%) were PED. One of the factors associated with a greater use of ATB in URI in the multivariate analysis was to be a FP (OR for ATB prescribing, PEDs vs. FPs: 0.65; 95% CI: 0.51-0.82).
Vernacchio et al.22 studied the adequateness of Primary Care doctors in following recommendations, from CPG, on the treatment of AOM in USA. A mail survey was sent in March 2006 to 477 FPs and PEDs inquiring about their opinions and practices regarding choices for observation or for antibiotic treatment when facing several common AOM scenarios. 299 answered (62.7%), of which 230 (76.9%) were PEDs. The initial vigilant attitude without ATB treatment was more frequent for PEDs (86.5% vs. 71.2%; RP: 1.21; 95% CI: 1.03-1.43).
Use of second line antibiotics
This result was evaluated in four studies.9-12 The different types of measurement used, and the marked statistical and clinical heterogeneity, did not allow the combination of the results. The characteristics of the studies are described individually.
Pennie et al.9 gathered data of the prescriptions of ten urban primary care offices (five family practices, three pediatric practices and two urgent care centers -UCC-), all of them attending children younger than 16 years of age during a period of three weeks in Ontario (Canada). For this purpose, were considered as reference the recommendations from a Clinical Practice Guideline on ATB treatment, in use in Ontario at the moment of the study. 3 out of 50 treatments prescribed by FPs were second-line ATBs (6%) vs. 36 out of 111 by PEDs (32%). PEDs were therefore, more likely than FPs to prescribe second-line antibiotics for AOM (RR: 5.4; 95% CI: 1.5-16.7)
Nash et al.10 examined the National Ambulatory Medical Care Survey (NAMCS) registers to analyze the antimicrobial prescribing habits of physicians who provide primary care for children during the years 1995-1998 in USA. During the period of time of the study, the PEDs and FPs received 13,078 visits of children, aged from 0 to 18 years. PEDs had a lower probability of prescribing second-line ATB for the treatment of viral URIs and bronchitis (OR: 0.81; 95% CI: 0.73-0.90, calculation based on logistic regression analysis). There were no differences in prescription between professionals (PED and FP) in the treatment of sinusitis and otitis media (OR: 1.03; 95% CI: 0.77-1.48).
Kozyrskyj et al.11 in 2004 analyzed the registers of four population databases of the MHSIP, that covers health care needs of all the population of Manitoba (Canada), during the period 1996-2000. They compared the prescription of ATB of second line in URI of probable viral origin (VURI) taking as a reference the recommendations of a CPG. During the study period 48,421 cases of VURI were attended. In comparison to GPs, PEDs had a lower probability of prescribing inadequately an ATB in VURI (OR: 0.51; 95% CI: 0.42-0.62), but a higher probability of prescribing second line ATB (OR: 1.27; 95% CI: 1.06-1.52).
Linder et al.12 analyzed the ATB treatment pattern for acute pharyngitis in children of ages 3 to 7 years. They used the registers of the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS). The latter has the registers of primary care visits to hospital Emergency Departments from 1995 to 2003. No differences were found between type of doctor in 4,158 children that were diagnosed of acute pharyngitis, in prescription of non recommended ATB (OR: 1.14; 95% CI: 0.72-1.80). Even so, in the cases diagnosed of sore throat, children were prescribed fewer ATB in visits to PEDs than in visits to other primary care physicians (OR: 1.58; 95% CI: 1.13-2.21).
Otitis media management
Ten studies analyzed the attitude of PED and FP/GP in relation to diagnosis and treatment of AOM (Table 2). Seven were cross-sectional studies and three were historical cohort studies. In five9,20,22-24 studies a comparison between both types of professionals was made in relation to a reference standard, that varied depending on the case, and that could be: a CPG, expert consensus, or a laboratory method that confirmed the diagnosis of the disease. Three were cross-sectional studies20,22,24 and two were historical cohort studies9,23. The heterogeneity due to type of study design, the methods of selection of the sample of participants and the reference standard used, did not permit the pooled analysis to obtain a global combined estimate.
In a study by Vernacchio et al.22 two types of ATB prescription were analyzed: a) the option of immediate prescription or b) the option for observation initially (based on the recommendations of a CPG that recommended the observation option, initially). PEDs adhered with greater frequency to the guidelines than FPs (RP: 1.21; 95% CI: 1.03-1.43).
Quach et al.23 reviewed the diagnosis and treatment of children aged < or = 6 years with diagnosis of AOM, between 1999 and 2002, included in a community database: Régie de l'Assurance Maladie du Quebec (RAMQ) (Canada). During the study period 60,513 children, < or = 6 years of age, experienced their first AOM episode, which were treated by 4,708 physicians [GPs: 87.3%/PED 9.1% and specialists in otorhinolaringology (ENT): 2.5 %]. The authors analyzed, by means of logistic regression, the adherence to the recommendation from the CPG of prescribing amoxicillin as the first-line ATB medication. PEDs were more likely to adhere to the recommendations (OR: 1.23; 95% CI: 1.18-1.28). Furthermore PEDs, in comparison to GPs, had a smaller probability of prescribing azitromicin, (OR: 0.62; 95% CI: 0.58-0.66) and claritromicin (OR: 0.63; 95% CI: 0.59-0.68). Overall, the adherence to consensus guidelines was higher for PEDs (OR 1.28; 95% CI: 1.05-1.57).
Pennie et al.9 observed that pediatricians were more likely to prescribe second-line antibiotics (RR: 5.4, 95% CI: 1.51-16.73). This result was obtained from a subgroup of 111 visits provided by PEDs and from 50 visits provided by FPs (the number of visits for AOM during the study period was 192 for PEDs and 64 for FPs).
Watson et al.20 studied the use of pneumatic otoscopy for the diagnosis of AOM. PEDs were more likely than FPs to perform pneumatic otoscopy, as recommended by a reference guideline (PR 1.39, 95% CI 1.18-1.64).
McIsaac et al.24 surveyed 2,234 FPs and 775 PEDs in Ontario (Canada). They obtained 950 responses (42.5%), with similar response rates for both types of physicians. The authors evaluated the rate of referrals to the otolaryngology service. PEDs referred their patients less frequently in several clinical situations: bilateral AOM (RP: 0.72, 95% CI: 0.61-0.84), nasopharyngeal obstruction (RP: 0.82, 95% CI: 0.72-0.93) or persistent effusion for more than 3 months (RP: 0.95, 95% CI: 0.90-1.01). FPs were more affected by parental concern when deciding to refer a child with AOM and referred more frequently (RP: 0.70, 95% CI: 0.59-0.83) when the parents expressed their preference for the placement of tympanostomy tubes. In the same way, FPs had lower thresholds for referring children when the parents expressed concern about the frequency or the perceived severity of the episodes (RP: 0.65, 95% CI: 0.55-0.76).
Five other studies compared the clinical practice of PEDs and FPs / GPs in the absence of a standard reference.2,17,19,25,26 Except for one case-control study,26 all have a cross-sectional design.
Asher et al.26 conducted a study in a hospital emergency department of a rural area of Israel. They performed tympanocentesis on every child with AOM referred from primary care during one year (590 children) and found no differences between PEDs and FPs / GPs in terms of diagnostic accuracy (OR 0.82, 95% CI: 0.56-1.21, logistic regression analysis).
In the formerly mentioned study of Davy et al.19 found no differences between PEDs and FPs in the number of antibiotic prescription (OR 0.86, 95% CI: 0.05-14.1), although PEDs prescribed fewer antibiotics when there was a previous history of AOM (RP: 0.63, 95% CI: 0.40-0.99).
Boulis et al.25 conducted a one-year telephone survey of 1,735 PEDs and 1,265 FPs in the USA (the response rate was 65.4%) and found that PEDs referred their patients less frequently than FPs to the otolaryngologist (OR 0.71, 95% CI: 0.61-0.82).
Roark et al.17 found no differences between PEDs and FPs in the use of pneumatic otoscopy, although FPs prescribed more second-line and high-cost antibiotics (RP: 1.51, 95% CI: 1.14-1.99) and more decongestants (RP: 2.78, 95% CI: 1.68-4.60) to treat persistent middle ear effusion. FPs also referred patients more often at the 9-week (RP: 2. 95% CI: 1.22-3.26) and 12-week follow-up visits (RP: 1.18, 95% CI: 1.04-1.35).
Fishbane et al.2 found a statistically significant positive trend for GPs to prescribe antibiotics in children with earache (a 35-45% higher for GPs comparing with PEDs).
Bronchial asthma management
Table 3 summarizes the main characteristics of the three reviewed studies.
Finkelstein et al.27 published in the year 2000 the results of a self-reported survey of primary care physicians (all the PEDs and a randomly selected sample of FPs of 3 USA states). The objective was to compare both types of professionals about the degree of adherence to the recommendations of an asthma guideline that was in use at the time of the study (1997). In total, 429 of the 722 mailed questionnaires were returned (64%). Thirteen were excluded for occupying less than 25% of their time or less than 8 hours per week in clinical practice, and 9 more were also excluded for reporting a specialty other than pediatrics or family medicine. The final sample was composed of 407 professionals (56.3%). The percentage by specialty was not reported. There were no differences between PEDs and FPs in the logistic regression analysis about the use of a trial of inhaled beta-2-agonists (OR: 0.8, 95% CI: 0.2-3.9). FPs were less likely to recommend daily home peak flow monitoring in the diagnosis than PEDs (36% vs. 54%, OR: 0.3, 95% CI: 0.1-0.5) but more likely to use office peak flow (96% vs. 68%, OR: 3, 95% CI: 0.8-10.8) and spirometry for the diagnosis of asthma (40% vs. 12%, OR: 5.9, 95% CI: 2.4-14.6). The study did not find differences about the practice of thorax or sinus radiographies although there was a non-significant trend for FPs to ask them more often (thorax X-ray: 38% vs. 24%, OR: 1.7, 95% CI: 0.8-3.5; sinus X-ray: 10% vs. 1%, OR: 5.3, 95% CI: 0.6-44). There were no differences in the practice of prick test or RAST (FPs 8% vs. 3% PEDs, OR: 1.2, 95% CI: 0.3-4.8). FPs referred more frequently in some clinical situations not covered by the guideline: 2-3 previous visits to hospital emergency department (OR: 5.1, 95% CI: 2.5-10.5), and history of hospitalization for acute asthma (OR: 2.8, 95% CI: 1.3-6.3). They also referred more often in two clinical situations included in the guideline as indications for referral: two previous exacerbations requiring treatment with oral steroids (OR: 2.9, 95% CI: 1.4-6.0), and children under 3 years requiring daily medication (OR: 7.8, 95% CI: 2.7-23.1).
Kozyrskyj et al.14 evaluated the use of antibiotic treatment for exacerbations in children with asthma between 1995 and 2000 (records from the MHSIP database). They assessed the adherence to asthma treatment guidelines which did not recommend the routine use of antibiotics for asthma exacerbation in children. In the logistic regression analysis FPs were more likely to prescribe antibiotics than PEDs in the first two days of the asthma exacerbation (OR: 2.15, 95% CI: 1.82-2.53). The authors also reported the percentages of antibiotics dispensed within 7 days of the exacerbation (71.5% FPs vs. 57.2% PEDs) but they did not analyze the data. From this information we have been able to calculate RR (95% CI 1.23-1.27), indicating that FPs were also more likely to prescribe antibiotics within 7 days of the episode of exacerbation.
Sun et al.28 published, in the year 2006, a study carried out in Taiwan with the aim of knowing the prescriptions habits of anti-asthma medications for PEDs and FPs. A nationwide database (National Health Insurance Research Database) was consulted to obtain the data. Drugs were grouped in six categories: inhaled adrenergic agonists, oral beta-2-agonists, inhaled corticosteroids, xanthine derivatives, oral corticosteroids and leukotriene receptor antagonists. During a period of three months 225,537 prescriptions were analyzed. FPs were more likely to prescribe drugs as monotherapy (45.8% vs. 34.6%, PR: 0.76, 95% CI 0.74-0.77) and more often prescribed two drugs simultaneously (43.8% vs. 39.9%, PR: 0.91, 95% CI: 0.89-0.93). The combination of more than two drugs was more common among PEDs (25.6% vs. 10.4%, PR: 2.47, 95% CI: 2.41-2.64). With regard to monotherapy, FPs prescribed more inhaled adrenergic bronchodilators (14.9% vs. 3.1%, RR: 0.21, 95% CI: 0.19-0.23) and more xanthine derivatives (30.1% vs. 16.9%, RR: 0.56, 95% CI: 0.53-0.59). PEDs were more likely to prescribe oral beta-2-agonists (70.4% vs. 46.9%, RR: 1.5, 95% CI: 1.45-1.56) and inhaled steroids (7.8 % vs. 5.6%, RR: 1.39, 95% CI: 1.21-1.6).
Fever management
Table 4 summarizes the main characteristics of the three reviewed studies.
In 1982, Leduc et al.29 conducted a prospective cohort study to assess the health outcomes of children seen at two emergency departments (one in a Children's hospital, where children were cared for pediatricians, and the other in a general hospital, where the attending doctors were FPs). Parents were interviewed by telephone, within two weeks of their emergency room visit, to determine outcomes based on duration of the illness episode and further physician contacts or admissions to hospital. The practice of complementary tests was also evaluated. Children less than 10 years of age with fever > 38 oC, seen at the emergency department, were included in the study. Children with underlying chronic diseases (diabetes, immunodeficiency) and those who had previously consulted for the same process were excluded. During the study period, 148 children were attended at the children's hospital and 111 at the general hospital. 90% and 94% of the parents, respectively, could be contacted. Eleven children (8.3%) seen at the children's hospital had unresolved symptoms at one week compared to 13 children (12.5%) seen at the general hospital (RR: 0.66; 95% CI: 0.31-1.42). In this subgroup of children, one of them needed hospitalization at the children's hospital, and three at the general hospital (RR 0.26, 95% CI 0.03-2.47). The overall frequency of laboratory use was similar in both groups [58 (39.2%) at children's hospital and 45 (40.5%) at general hospital]. However, significant differences were noted in the type of test used. GPs ordered more roentgenograms than PEDs: 36 (32.4%) vs. 16 (14.4%); RR: 1.69 (95% CI: 0.99-2.88). The result of X-rays was more likely to be abnormal when asked by PEDs: 7 cases of 16 (43.8%) vs. 6 of 36 (16.7%); RR: 2.6 (95% CI: 1.1-6.6). PEDs performed more frequently than GPs streptococcal antigen detection (28 vs. 2, RR: 18.7, 95% CI: 4.5-76.7) and obtained more positive results than FPs [9 vs. 0, risk difference (RD): 32.1%, 95% CI: 14.8-49.4]. The same occurred with cultures: PEDs asked more microbiologic cultures (30 vs. 5; RR: 4.5, 95% CI: 1.8-11.2) and obtained more positive tests, even though the results were non-significant (2 vs. 0 cases; DR: 6.7%, 95% CI: -2.3-15.6).
Zerr et al.30 published in 1999 the results of a survey conducted to a random sample of PEDs, FPs and emergency physicians of USA hospitals. The sample was obtained from Medical Marketing Services, a company authorized to provide data of physicians affiliated to the American Medical Association (AMA). The main objective of the study was to investigate differences for these three types of physicians in the degree of compliance with the recommendations of a guideline for the management of fever without source in children. Two theoretical clinical scenarios whit febrile babies (the first one showing a 2-week-old baby and the second case corresponding to an 8-week-old infant) were used to assess the degree of adherence. The study was considered of medium quality. Of the 1,500 mailed surveys, 474 (31.6%) were answered (193 PEDs, 177 emergency physicians and 104 FPs). The response rate by type of physicians was 42%, 41% and 23% respectively. According to the recommendations of the guideline, the 2-week-old newborn should be admitted to hospital and cultures of CSF, blood, and urine should be obtained. PEDs adhered more frequently to the recommendations than FPs (OR: 9.13, 95% CI: 3.4-24.5, as determined by logistic regression analysis).
In the previously cited study of Boulis,25 three of the six vignettes presented clinical scenarios related to febrile illnesses. The case number two: presented an otherwise healthy 10-year-old boy with a 2-day history of fever, nasal stuffiness, sore throat, and no other signs or symptoms. The parents called to the office to report the clinical situation. The authors assessed the percentage of such patients for which the physician would recommend an office visit. FPs more frequently recommended an office visit than PEDs: 69.8% (95% CI: 68.6-71.1) compared to 63.3% (95% CI: 62.3-64.3). DR estimated by multivariate analysis: -7.3%, 95% CI: -9 to -5.6. Case number 3: an otherwise healthy 10-year-old girl with a 3-day history of fever of 38.6 oC, productive cough, tachypnea, and rales at the right base. She was able to take fluids. Physicians were asked for what percentage of such patients would they recommend a chest x-ray. The 51.3% (95% CI: 49.4-53.2) of FPs compared to 47.7% (95% CI: 46.7-48.8) of PEDs said that they would recommend a chest x-ray (DR estimated by multivariate analysis: -6.9%, 95% CI: -8.8 to -4.9). Case number six: an otherwise healthy full-term 6-week-old infant with a temperature of 38.3 oC. Physicians were asked for what percentage of such patients would they recommend sepsis workup (complete blood cell count, urine culture and blood culture). PEDs were more likely to perform tests to rule out sepsis (81.1%; 95% CI: 80.4-81.8) than FPs (66.4%; 95% CI: 65.3-67.5). DR estimated by multivariate analysis: 12.5%, 95% CI: 10.7-14.3.
Psychiatric conditions' management
The main characteristics of the three selected studies are summarized in Table 5.
Rushton et al.31-33 studied the different attitudes of different types of medical professionals for the treatment of depression, in terms of patterns of prescription of selective serotonin reuptake inhibitors (SSRIs) and in terms of the adherence to the recommendations from a practice guideline, about treatment of the attention-deficit/hyperactivity disorder (ADHD).
In the year 2000 Rushton et al.31 published the results from a mail survey carried out among PEDs and FPs in North Carolina (USA). The objective was to compare self-described PEDs' and FPs' attitudes in the diagnostic assessment and in the therapeutic management of childhood depression. The sample of the study was formed by all pediatricians (PEDs) aged less than 65 years old (595) practicing in a primary care setting and by a similar number (557) of family physicians (FPs), also less than 65 year of age and actively practicing in the moment of conducting the survey. The self-assessed questionnaire was sent to 1,016 doctors (505 PEDs and 511 FPs). The sample was extracted from a data base of graduated professionals in North Carolina. The questionnaires were answered by 591 doctors (349 PEDs and 242 FPs).
Results of the bivariate analysis: 48% of the FPs and 78% of PEDs used referral to the specialized level (RP: 1.63; 95% CI: 1.41-1.88, taking FPs as the reference category); prescribed medications 18% of the FPs and 9% of PEDs (RP: 2; 95% CI: 1.33-3.14, taking PEDs as the category of reference in the comparison); provided counseling in their offices 61% of the FPs vs. a 59% of the PEDs (RP: 1.04; 95% CI: 0,91-1,18, taking PEDs as the category of reference in the comparison); and initially maintained an expectant behavior 22% of the FPs vs. a 20% of the PEDs (RP: 1.09; 95% CI: 0.80-1.50). Regarding to the variable "counseling", PEDs used referral with that purpose to the specialist more frequently that the FPs did it: 86% vs. 63% (RP: 1.37; 95% CI: 1.23-1.52, taking FPs as the category of reference in the comparison).
Regarding the degree of agreement with a set of presented statements (possible answers were: "yes"/"do not"; results calculated from data available of the 236 respondent FPs and the 332 respondent PEDs), FPs agreed more frequently than PEDs with the following statement: "I feel comfortable with the management of child depression": 22% vs. 11% (RP: 1.98; 95% CI: 1.34-2.91, taking PEDs as the category of reference in the comparison); FPs shown a higher degree of agreement than PEDs with this statement: "SSRIs are safer than other antidepressant medications in children and adolescents", 63% vs. 48% (RP: 1.3; 95% CI: 1.12-1.51, taking PEDs as the category of reference in the comparison); FPs agreed more frequently than PEDs with the following assertion: "the lack of specialist available for referral forces me to arrange treatment of child depression on my own", 20% vs. 12% (RP: 1.65; 95% CI: 1.12-2.43, taking PEDs as the category of reference in the comparison). Regarding to the variable "prescription", FPs started treatment with an antidepressant medication, before referral, more frequently than PEDs: 28% vs. 6% (RP: 4.67; 95% CI: 2.94-7.4, taking PEDs as the category acting as point of reference in the comparison). In logistic regression analysis, being a FP was associated with a higher likelihood of prescribing medications for childhood depression: OR 4.9 (95% CI: 2.8-8.7).
In the year 2000, the same authors, using the same sample of the previously commented study, published the results of the survey, related this time to the prescription of SSRIs antidepressants and their indications for several psychiatrics disorders.32 In the bivariate analysis FPs were more likely than pediatricians to use SSRIs for any of the psychiatric conditions considered in the study: 91% vs. 58% (RP: 1.57; 95% CI: 1.42-1.73); FPs were more likely than PEDs to prescribe SSRIs in association with other psychotropic medications: 54% vs. 31% (RP: 1.75; 95% CI: 1.44-2.13). In the separate analysis for every diagnosis, FPs prescribed SSRIs for depression more frequently than PEDs: 88% vs. 51% (RP: 1.73; 95% CI: 1.54-1.93); FPs used SSRIs for the attention-deficit/hyperactivity disorder (ADHD) more frequently than PEDs: 45% vs. 30% (RP: 1.5; 95% CI: 1.21-1.85); the FPs used SSRIs for the obsessive-compulsive disorder more frequently than the PEDs: 38% vs. 28% (RP: 1,35; 95% CI: 1.07-1.71). There were no differences found between FPs and PEDs in the likelihood of prescription of SSRIs for the treatment of "aggressive behavior", 26% vs. 20% (RP: 1.3; 95% CI: 0.96-1.75). FPs were more likely to use SSRIs for the treatment of eating disorders than PEDs: 32% vs. 9% (RP: 3.58; 95% CI: 2.44-5.26). FPs were more likely to prescribe SSRIs for enuresis than PEDs: 12% vs. 7% (RP: 1.74; 95% CI: 1.04-2.92). Other results of interest: 41% of the respondent FPs reported the prescription of SSRIs in at least one adolescent, in the six months period of time before the survey, versus a 26% of the respondent PEDs (RP: 1.57; 95% CI: 1.24-1.98); PFs were less likely to use referrals to the specialist in mental health: 48% vs. 77% for PEDs (RP: 0.62; 95% CI: 0.54-0.72). It was found, in the logistic regression analysis, that being a FP was associated with a higher likelihood of prescription of an SSRI for any of the considered diagnosis (OR: 6.5; 95% CI: 3.7-11.4).
The same authors published in the year 2004 the results of a mail survey carried out in the year 2002 and targeted to PEDs and FPs of the state of Michigan (USA).33 The objective of the study was to evaluate the degree of adherence of primary care physicians to the recommendations of a practice guideline about diagnosis and management of the ADHD, as well as determine which factors influenced those different degrees of concordance with the recommendations. A mailed self-reported questionnaire was sent to all the PEDs in the state of Michigan (687) and to a randomly selected sample of 687 FPs (of a total amount of 1,547). Data of both types of medical professional were obtained from the American Medical Association Master File. The sampling strategy rendered a total number of 1,347 after application of the following exclusion criteria: physicians who were younger than 30 years or older than 65 years, retirees, Veterans Administration employees, physicians with nongeneralist board or subboard certification, and those having non-Michigan-based office practices. Of the 1,374 physicians in the sample, 166 were found to be ineligible (retired, did not see children, not in primary care, or moved). For the remaining 1,208, the overall response rate was 60% (723 of 1,208), with 67% for PEDs (405 of 608) and 53% for FPs (318 of 600).
Results of the bivariate analysis: 91.5% of the PEDs were familiar with the practice guideline, versus the 59.8% of the FPs (RP: 1.31; 95% CI: 1.18-1.46); reported incorporation of the guidelines into their practice 78.1% of the PEDs and 39% of the FPs (RP: 2; 95% CI: 1.73-2.32). With regard to recommendations on diagnosis (percentage of respondents that follow each recommendation, indicated as "routinely" versus "never, rarely or sometimes"): 77% of PEDs reported routine use of parents rating scales of symptoms in diagnosing ADHD (vs. a 61.6% FPs; RP: 1.25; 95 CI%: 1.13-1.38); 84.4% of PEDs reported routine use of teacher rating scales in diagnosing ADHD (vs. a 70.8% of the FPs; RP: 1.19; 95% CI: 1.10-1.30); a 70.4% of PEDs reported assessment for comorbidity (vs. a 68.5% of FPs; RP: 1.03; 95% CI: 0.93-1.14), and 55.4% of the PEDs reported routine use of the Diagnostic and Statistical Manual of Mental Disorders criteria for diagnosis of ADHD (vs. a 30% of FPs; RP: 1.85; 95% CI: 1.53-2.24).
With regard to recommendations about treatment (percentage of respondents that follow each recommendation, indicated as "routinely" versus "never, rarely or sometimes"), 72.2% of the PEDs (vs. a 59.2% of the FPs) used the recommended medications in the practice guideline (RP: 1.22; 95% CI: 1.09-1.36); 80.9% of PEDs monitored medications in the reevaluation, a month after prescription, also titrating when needed, vs. a 81.7% of FPs (RP: 0.99; 95% CI: 0.92-1.06); 41.6% of PEDs reported follow-up evaluations, 3-4 times a year, for children who receive medications to evaluate response, vs. a 67.5% of FPs (RP: 0.62; 95% CI: 0.54-0.71); 56.4% of the PEDs reconsidered diagnosis in the patient when two or more medications were unsuccessful, vs. the 46.3% of the FPs (RP: 1.22; 95% CI: 1.05-1.41); 56.3% of PEDs and 53.2% of PFs made recommendations for behavioral therapy (RP: 1.01; 95 CI %: 0.88-1.16); 18.1% of PEDs ordered laboratory tests not recommended in the guideline (thyroid, lead, or iron testing), vs. a 39.6% of FPs (RP: 0.45; 95% CI: 0.35-0.58). In the logistic regression analysis, the likelihood of incorporating the recommendations of the practice guideline was higher among PEDs (OR: 5.4; 95% CI: 2.6-11).
Immunizations
The main characteristics of the selected studies are summarized in Table 6.
This topic was reviewed in 16 studies: 14 cross-sectional descriptive studies and two historical cohort studies.
In the study of Starfield et al.5 published in 1985, 429 PEDs and 611 PFs/GPs were interviewed by means of a national survey. The percentage of respondents by type of professionals were: 50% for PEDs, 44% for FPs and 36% for GPs. Pediatricians, in comparison with the others types o professionals, were more likely to administer immunizations to the following groups of population: aged between 15 and 19 years, and aged between 10 and 14 years, when they consulted for a preventive check-up visit. The authors did not offer numerical results.
Freed et al.34 developed in 1994 a study, with a cohort survey-over-time kind of design, and performed through successive mail surveys to a sample of 591 physicians of primary care (438 PEDs and 153 FPs) in North Carolina (USA). The objective was to determine the degree of adoption, by both types of professionals, of the official recommendation about the universal hepatitis B immunization of infants released by the American Academy of Pediatrics, the American Academy of Family Physicians and the Advisory Committee on Immunization Practices (AAP, AAFP, and the ACIP). The survey was responded by 363 PEDs (82.9%) and 110 FPs (71.9%). 66 % of PEDs (vs. a 32% of FPs) agreed that universal immunization was warranted (RP: 2.1; 95% CI: 1.6-2.8); 53% of pediatricians had actually adopted the immunization of all newborns into practice, vs. a 23% of family physicians (RP: 2.3; 95% CI: 1.6-3.3).
Szylagyi et al.35 carried out, in 1994, a cross-sectional descriptive study by means of a self-reported survey sent to a randomly selected sample of 1,310 PEDs and 954 FPs in the USA. It was responded by 1,075 PEDs (82%) and 490 FPs (51%). The objectives of the study were to compare, in the first place, the differences in attitudes and beliefs regarding immunizations among PEDs and FPs, and secondly, the differences that these two types of medical professionals showed in their respective current practices. The differences were investigated in terms of adherence to current immunization recommendations and standards from guidelines. The guidelines and standards considered of reference were those issued by the AAP, AAFP and the ACIP (American Academy of Pediatrics, the American Academy of Family Physicians and the Advisory Committee on Immunization Practices), and published after the performance of the survey. Bivariate analysis: with regard to the kind of visit in which they would administer vaccinations (check-up, acute illness visits, follow-up visits, or chronic illness visits). There was no difference found between PEDs and PFs for the first two types of visit -check-up (100% vs. 99%) and acute illness (29% vs. 28%)-. Pediatricians, in comparison with PFs, were more likely also to immunize children using the follow-up visits (92% vs. 86%; RP: 1.07; 95% CI: 1.02-1.12) and using the chronic illness visits (81% vs. 70%; RP: 1.16; 95% CI: 1.08-1.24). Regarding mechanisms to identify undervaccinated children, there was no arrangement at all with this purpose for a 48%, in the case of the PEDs, vs. a 68% for the PFs (RP: 0.71; 95% CI: 0.64-0.78); in addition, a 43% of PEDs systematically registered vaccinations vs. a 35% of FPs (RP: 1.23; 95% CI: 1.06-1.43).
In the logistic regression analysis the likelihood of keeping a tracking system, with records, able to identify children with incomplete immunization, was higher for pediatricians (OR: 2; 95% CI: 1.6-2.7).
Freed et al.36 in 1998, conducted a cross-sectional descriptive study (cross-sectional mail survey, by means of a self-reported questionnaire) to PEDs and FPs, from nine states of the USA, included in the American Medical Association Masterfile database. The objective of the study was to explore the effect of concern about vaccine-associated malpractice litigation, on the practice from both types of medical care providers. The study examined, through a logistic regression analysis, the perceptions of PEDs and FPs regarding the safety of giving immunizations to children with a minor respiratory tract illness, without a fever (or only with low-grade fever); the perception on the safety of administering the diphtheria, tetanus, and pertussis vaccine to children with a family history of seizures; the perceptions of the safety of using DTP vaccine in children with a local reaction and a fever (temperature < 40.5 oC) after a previous administration of the DTP vaccine; and whether physicians reported giving immunizations at acute care visits, when not specifically contraindicated.
From the 3,014 physicians in the total sample selected to be mailed (1,165 pediatricians and 1,849 family physicians) 1,863 responded (66%); from this number, the 442 respondents who did not give immunizations and who did not provide well-child care, were excluded. This subtraction left a final sample of 1,421 for subsequent analysis (47.1% of the initial sample), which, with further application of rescaled weights, yielded effective sample sizes of 704 PEDs (60.4%) and 679 FPs (39.1%)
Bivariate analysis: in the comparison, PEDs were more likely than FPs to believe that the diphtheria, tetanus, and pertussis vaccine could be administered safely to children with a family history of seizures: 84% of PEDs vs. a 66% of FPs (RP: 1.27; 95% CI: 1.2-1.35). Pediatricians were more likely than FPs to report their perceptions that the administration of vaccines to children with a minor respiratory tract illness was a safe and effective procedure: 95% vs. 86% (RP: 1.1: 95% CI: 1.07-1.14); and PEDs were also more likely than FPs to report perceptions of the safety of DTP vaccine use in children with a fever after a previous DTP vaccine (temperature < 40 oC): 73% vs. 57% (RP: 1.28; 95% CI: 1.18-1.39). Pediatricians were more likely than family physicians to record immunizations on a special page in the patient's medical record (96% vs. 86%; RP: 1.12; 95% CI: 1.08-1.15) and to register immunizations in some type of computer-based system (23% vs. 7%; RP: 3.3; 95% CI: 2.4-4.4). In the logistic regression analysis, FPs were more likely than PEDs to defer immunization: a) because of a mild respiratory illness (OR: 0.29; p < 0.001), b) because a fever reactions to previous doses of the same vaccine (OR: 0.39; p < 0.001), or c) because of a family history of seizures (OR: 0.33; p < 0.001)
Ipp et al.37 conducted in Canada a cross-sectional study consisting in a survey carried out by sending a self-administered questionnaire to a random sample of 100 family physicians, 100 pediatricians and all the 130 subspecialists at The Hospital for Sick Children, Toronto. Of the 315 eligible physicians, 247(77%) responded, including 76 FP (78%) and 72 Community Pediatricians (83%). The objective was to determine the variability in physician knowledge, attitudes, and behaviours in relation to influenza vaccination of high-risk children.
Of the three groups, community PEDs were more likely than, either family physicians or subspecialists, to recommend vaccination for all the high-risk conditions: heart diseases (70% vs. 60%; RP: 1.23; 95 % CI: 1.09-1.39), asthma (94% vs. 74%; RP: 1.28; 95% CI: 1.11-1.48), bronchopulmonary dysplasia/cystic fibrosis (96% vs. 76%; RP:1.26; 95% CI: 1.10-1.44) and acetylsalicylic acid long-term treatment (71% vs. 41%; RP: 1.74; 95% CI: 1.28-2.36). There was also a nonsignificant trend for pediatricians to vaccinate more often institutionalized patients (74% vs. 61%; RP: 1.22; 95% CI: 0.97-1.53) and children receiving immunosuppressive therapy (71% vs. 62%; RP: 1.15; 95% CI: 0.91-1.44).
Ewing et al.38 published in 1999 a cross-sectional study performed by a mail survey using a self-completed questionnaire sent to a randomly selected sample of physicians of different medical specialties in the USA, who provided primary care (PC) at least 50% of their working time. The aim of this study was to compare the provision of clinical preventive services delivered by different type of primary caregivers. Of 1,629 PEDs, 1,303 (80%) answered the questionnaire. After applying the criterion "work in PC more than 50% of the working hours", the sample was reduced to 788 (61%). In relation to FPs, from an initial sample of 5,000, 2,511 answered the survey (50%). After applying the criterion "work in PC more than 50% of the working hours", the sample was reduced to 2,117 (84%). Among the preventive activities evaluated, the authors studied the degree of adherence to the recommendation of influenza vaccination. PEDs were more likely to recommend influenza vaccination than FPs (85.3% vs. 31.3%; RP: 2.7; 95% CI: 2.5-2.9; bivariate analysis).
In 1999, Santoli et al.39 published the results of a telephone survey conducted to a sample of parents of 28,298 children in the USA (50 states, the District of Columbia and 27 selected urban areas). The objective was to compare the immunization status in non institutionalized healthy children, aged 19 to 35 months, verifying their vaccination status, checking up the provider record, and examining the relationship between the characteristics of the providers enrolled in the Vaccines For Children program and the immunization status. Data were available for 21,522 children (76%). Children were considered to be properly immunized when they had received > 4 doses of DTP or DTaP, > 3 doses of oral polio, > 1 dose of measles-mumps-rubella (MMR) and > 3 doses of Hib ( = 4:3:1:3), before the survey began. Children vaccinated solely by pediatricians were more likely to have received the complete 4:3:1:3 course than those vaccinated only by family physicians (80% vs. 71%, p <0.05 on bivariate analysis) (OR: 1.63, 95% CI: 1.46-1.82 in the logistic regression analysis).
Takayama et al.40 published in 1999 a cross-sectional study based in a mailed self-administered survey sent to physicians. This study was conducted in the counties of Sacramento and San Francisco (USA). The survey was mailed to 855 PEDs and FPs in both counties. The number of respondents was 533 (62%). Of these, 211 were excluded as they did not provide primary care to children. The final sample consisted of 322 physicians (37.7%): 155 in San Francisco and 167 in Sacramento. Of the 322 participants, 110 were PEDs and 86 GPs/FPs. The rest (5) belonged to other specialties. The aim was to compare the percentage of children vaccinated against hepatitis B in these two counties. An intervention was made in San Francisco (the Universal Infant Hepatitis B Immunization Demonstration Project), while none was undertaken in Sacramento. Comparing primary care physician immunization practices, by logistic regression analysis, they found that being PED was a predictive factor for presenting a proper immunization status against hepatitis B in both, the San Francisco (OR: 2,0; 95% CI:1.7-2.4), and the Sacramento (OR: 2.13; 95% CI not offered) counties.
Ehresmann et al.41 sought to determine PEDs and FPs' attitudes and practices regarding varicella vaccine in a study published in 2000. A random sample of 420 physicians (319 FPs and 101 PEDs) was selected to fill in a mailed questionnaire. Ninety-one, who were not providing primary care services (including immunization), were excluded. Among the remaining 327 physicians, 255 completed the survey (78%), including 190 (77%) of 248 family physicians and 65 (82%) of 79 pediatricians. There were no differences in the logistic regression analysis (OR: 1.2; 95% CI: 0.5-2.8) between the two types of specialist to actively offer the immunization. Regarding the statement "All infants and children (from 12 months to 18 years) should be vaccinated", 60% of PEDs agreed vs. 40% of FPs (RP: 1.64; 95% CI: 1.22-2.21; bivariate analysis). Concerning to the statement "all children of any age should be vaccinated, unless good documented personal history of previously passed chickenpox", 61% of PEDs agreed vs. a 42% of FPs (RP: 1.55; 95% CI: 1.16-2.07; bivariate analysis). There were no differences between both groups regarding the statement "varicella vaccine is safe" (98% of physicians from both specialties agreed). Concerning to the statement "children already receive too many injections to add varicella vaccine", 27% of FPs agreed (vs. a 10% of PEDs) (RP: 0.39; 95% CI: 0.17-0.87; bivariate analysis). Finally, regarding the statement "I prefer to wait until a new combined vaccine (including varicella as one of its components) is available", 22% of the FPs agreed (vs. a 6% of PEDs) (RP: 0.35; 95% CI: 0.13-0.96; bivariate analysis).
Kahane et al.42 published in 2000 a cross-sectional study, by site-surveying physicians and nurses at private medical practices, in three counties in California (USA). Of the 72 eligible practices that were contacted, 45 participated in the study, yielding a participation rate of 62%. The immunization charts of children aged 12 to 35 months were examined (1,719 of 2,325 eligible, 78%). The probability of incomplete vaccination at 24 months of age was higher in children visiting FPs than visiting PEDs: OR: 2.79 (95% CI: 1.54-5.07). This association was not significant after applying the logistic regression analysis (numeric data not shown by authors).
LeBaron et al.43 published in 2001 the results of an ecological study, conducted in all USA states, which approached the relationship between the distribution of each type of professional in each state (PEDs, FPs, GPs) with the percentage of properly immunized children at a mean age of 27 months - children were considered as properly immunized when they had received > 4 doses of DTP or DTaP, > 3 doses of oral polio, > 1 dose of measles-mumps-rubella (MMR) and > 3 doses of Hib (4:3:1:3). As a final number there were 96,689 physicians (PEDs: 37%, FPs: 49% and GPs: 14%) who provided routine care to children. Higher rates of vaccination were associated with a higher concentration of PEDs in the geographical areas studied (coefficient b: 0.006, p = 0.001 in multiple regression analysis).
Schaffer et al.44 studied the physicians' attitudes and practices on adolescent immunization. A self-administered survey was mailed to a randomly selected sample of PEDs and FPs in USA (using the AMA Masterfile database). Of the 1,480 questionnaires mailed, 1,110 were answered (75%); 536 were PEDs (response rate 81%) and 582 were FPs (response rate 71%). Of the physicians who responded, 761 (69%) met the inclusion criteria established by the authors (seeing > 4 adolescents per month in PC).The study sample consisted of 761 physicians (406 PED and 335 FP). Logistic regression analysis results showed that PEDs were more likely to have protocols for adolescent immunization (OR: 1.47; 95% CI: 1.22-1.78), to check more frequently the immunization status taking advantage of an illness consultation (OR: 1.42; 95 % CI : 1.22-1.65) and at follow-up visits (OR: 1.43; 95% CI: 1.23-1.67) than FPs; PEDs also were more likely to routinely immunize at illness-related visits (OR: 1.31; 95%: CI: 1.09-1.58) and at follow-up visits (OR: 1.49; 95%: CI: 1.46-1.51), to administer immunization to eligible adolescents more frequently against tetanus (OR: 3.31; 95% CI: 1.73-6.63), to administer a second dose of MMR (OR: 3.01; 95% CI: 1.77-5.12), to vaccinate against hepatitis B (OR: 2.09; 95% CI: 1.64-2.65) and against varicella (OR: 2.28; 95% CI: 1.90-2.72), and to use tracking and recall systems of adolescents who were behind on vaccines, comparing with official immunization schedules and expected standards of proper vaccination for their age (OR: 1.29; 95%: CI: 1.06-1.57).
Cohen et al.45 published in 2003 a cross-sectional study conducted by a survey completed by physicians. The objective was to determine physician success at designing catch-up regimens for children delayed according to standard immunization schedule.The study was conducted in a county of Illinois (USA). A sample of 1,513 physicians was randomly selected from the AMA medical register. Surveys included 6 open-ended vignettes describing hypothetical children delayed in immunization for which participants were asked to design catch-up regimens. In each vignette the following questions were proposed to the physician: "What would you give now?; When would you schedule the next visit?; What would you give at that time?" In the scoring system used, one point was added up for every correctly responded scenario. Participants were then divided according to whether they scored > 2 or < 1 than the mean score. Furthermore, five theoretical scenarios were presented, and, in each one of them, whether the MMR and/or the haemophillus influenzae type b (Hib) vaccines should be administrated was asked. The measured result was the percentage of professionals who do not administer MMR or Hib vaccinations. The survey was answered by 550 (36.4%) physicians. The demographic and practice characteristics of responders and non-responders were compared and it was noteworthy that, among the survey respondents, 55% were PEDs and 45% were FPs/GPs, whereas among non-respondents, the proportions were reversed: 34% of PEDs and 66% of FPs/GPs. PEDs were 4.3 (95% CI: 2.6-7.1) times more likely than FPs and 2.9 times more likely than GPs (95% CI: 1.04-7.7) to score over the average (1.83 points), in the clinical scenarios, in the logistic regression analysis. The authors did not assess the results, by type of professional, of the five additional scenarios in where possible contraindications for MMR and Hib vaccines were inquired.
Davis et al.46 in 2003 published the results of a survey made to physicians of 24 states in USA (AMA Masterfile database). The aim was to compare PEDs and FPs in adopting the immunization schedule of the pneumococcal conjugate vaccine, once its inclusion had been approved for all children younger than two years and for children aged 24-59 months at increased risk for developing pneumococcal diseases or complications. The survey was mailed to a sample of 788 FPs and 833 PEDs. Finally 259 FPs (32.9%) and 435 PEDs (52.2%) were eligible. Ninety-nine percent of PEDs and 68% of FPs adopted the recommendation (RP: 1.46; 95% CI: 1.34-1.59, bivariate analysis).
Bocquet et al.16 conducted a retrospective cohort study analyzing information from an automated medical database in a region of France (Franche-Comté). The percentage of vaccination coverage was higher among PEDs, compared to FPs. More specifically, authors provide numerical data on the hepatitis B vaccine (31% more than the FPs) and MMR vaccine (7% more).
Posfay-Barbe et al.47 (Switzerland) published in 2005 a cross-sectional study using an Internet-based survey. The aim was to measure various vaccination attitudes in PEDs and other no PEDs health professionals. Specifically, they were inquired about the attitude to take over their own children. The survey was sent to 2,070 physicians (860 of them were PEDs) being subscribers to the newsletter subscriber list InfoVac (www.infovac.ch) The survey consisted of 11 questions with 102 possible responses. There were 1,017 respondents (PED: 53.3%). The sample was reduced to 915 (PED: 392; 42.8%) due to defects on some of the questionnaire forms. PEDs mothers and fathers were more likely to follow the official immunization recommendations than non-PEDs physicians parents (91.6% vs. 85.1%; OR: 2.19; 95% CI: 1.37-3.49; logistic regression).
Cardiovascular risk
Ten studies have assessed PEDs and FPs/GPs attitudes towards health education activities (healthy habits promotion) and toward the realization of diagnosis and prevention activities on overweight-obesity and on toxic habits (tobacco and alcohol consumption). All studies were cross-sectional design, using surveys, except one, which was based on computerized register data. They are described in Table 7 in more detail.
Franzgrote et al.48 published in 1997 a survey, for primary care physicians working in California (USA), carried out to determine how frequently they asked adolescents about tobacco consumption. A self-administered questionnaire was mailed to a randomly selected sample of PEDs, FPs, internists and adolescent medicine specialists. The final sample consisted of physicians who spent at least 50% of their patient care time in primary care and who had graduated between 1970 and 1985. The survey was sent to 754 physicians and 77% responded. By specialty, the response rate was 77% of FPs and 78% of PEDs. The main results were: a) Percentage of adolescents, aged 11-14 years old, screened for regular smoking during routine health control visits: 61.3% PEDs (95% CI: 53.7%-66.8%) vs. 69.2% FPs (95% CI: 63.8-74.6), RP: 0.89 (95% CI: 0.72-1.09); b) Percentage of adolescents, aged 15-18 years old, screened for regular smoking during such visits: 74.4% PEDs (95% CI: 67.2%-81.7%) vs. 85.2% FPs (95% CI: 81.1-89.4), RP: 0.87 (95 % CI: 0.76-1.01); c) Percentage of 11-14 years old adolescents screened for regular smoking during spontaneous acute-care visits: 9.6% PEDs (95% CI: 6-13.3) vs. 29.1% FPs (95% CI: 22.6-35.7), RP: 0.33 (95% CI: 0.17-0.65); d) Percentage of 15-18 years old adolescents screened for regular smoking during spontaneous visits: 16% PEDs (95% CI: 11.7-20.4) vs. 50.1% FPs (95% CI: 43.5-56.6), RP: 0.32 (95% CI: 0.20-0.52).
Kimm et al.49 published in 1998 the results of a telephone survey, conducted with primary care physicians in the US, in order to study their attitude on cardiovascular risk factors identification in primary care. The sample was randomly selected from professional association records. Three practice categories were differentiated: FP, GP and PED, who should meet two eligibility criteria: to have at least five pediatric patient contacts per week and to dedicate more than 20 hours per week of direct patient care. 1,036 professionals, who met those criteria, answered the survey (52.5% response rate). The response rate varied significantly among specialties (63.6% PEDs vs. 50.7% FPs and 40.3 % GPs; p < 0.001). FPs and GPs categories were grouped to calculate the RP and its 95% CI. PEDs were more likely to make a cholesterol routine screening in the general population (RP: 1.56; 95% CI: 1.19-2.04) and in children with a positive cardiovascular disease family history (RP: 1.26; 95% CI: 1.11-1.39). PEDs screened hypercholesterolemia at an earlier age when family history was positive: 4.7 years old (versus 8.7 years old for GPs and 8.5 years old for FPs; p < 0.001). In relation to initiate hypercholesterolemia treatment, it cannot be estimated by specialties; overall, 70.8% of all physicians prescribed diet and 17.4% prescribed more physical exercising in addition to diet. Regarding to pharmacologic therapy, PEDs prescribed fewer drugs than GPs and FPs (RP: 0.65; 95% CI: 0.48-0.89). Regarding the screening of arterial hypertension, 99% of all the physicians performed it; PEDs performed it at a lower age: 2.9 years old versus 5.4 years old (FPs) and 6.9 years old (GPs). The differences were not statistically significant, due to the low number of responses on this item. Regarding hypertension treatment, the method most frequently used by the physicians was the combination of diet and exercise (60%). A rate of 25.5% used drugs, but there were no differences between PEDs and FPs/GPs (RP: 0.95; 95% CI: 0.7-1.28).
Ewing's 1999 study approached the attitudes, in the medical office, about dietetic habits and tobacco consumption.38 PEDs asked more often than FPs on dietetic habits (53.3% vs. 18.6%; OR in multivariate analysis: 3.96; p < 0.05) and were more likely to counsel about this subject (31.5% vs. 24%; OR: 1.27; p < 0.05). Regarding the tobacco consumption, PEDs asked less about it (8.4% vs. 58.6%; OR: 0.28; p < 0.05) and counselled less frequently (18.7% vs. 43.5%; OR: 0.29; p < 0.05).
Klein et al.50 published in 2001 the results of a self-reported survey mailed to primary care physicians in three metropolitan areas of New York (USA). The objectives were to describe the delivery of preventive practices about the smoking habit to adolescents (counseling, screening cessation...) and to examine the effect on it, among other characteristics, of the physician specialty. The survey was sent to 661 physicians who had seen 1 or more adolescents for well care within the past 6 months. Of the 551 eligible physicians, 156 did not respond, 24 refused to participate and 371 returned completed surveys (67%). Respondents included 192 PEDs and 179 FPs. In the multivariate regression analysis, being FP was associated with a greater probability of offering an adequate tobacco cessation counselling (beta coefficient: 13.8; 95% CI: 9.1-18.6; p < 0.001).
Pérez-Stable et al.51 published in 2001 the results of a self administered survey mailed to physicians practicing in California (USA). The objective was to evaluate primary care physicians in their knowledge and practice of smoking cessation counselling with patents. To be eligible, pediatricians and family physicians had to visit patients aged 18 years or younger, and to practice in an ambulatory setting. They were randomly selected from the American Medical Association Physician Masterfile. Of the 1,000 mailed surveys, 899 were eligible and 499 (56% response rate) were returned and completed. The questionnaire posed queries to physician about if they asked the parents of children, aged 5 years or younger, about smoking. The question "if parents smoked regularly" was asked by 62% of PEDs and 65% of FPs (RP: 0.95; 95% CI: 0.83-1.09); the question "if parents smoked at home" was asked by 73% of PEDs and 64% of FPs (RP: 1.14; 95% CI: 1.01-1.29). Referring to the smoking cessation counseling to parents, 79% of PEDs (69% of FPs) informed on passive smoking risk to children (RP: 1.14; 95% CI: 1.02-1.27); PEDs were more likely to report that they registered in the medical record, as a medical problem for the children, their parents smoking habit (65% vs. 48%; RP: 1.36; 95% CI 1.16-1.6); 77% of PEDs and 78% of FPs reported smoking cessation counseling to parents (RP: 0.99; 95% CI: 0.9-1.09); PEDs compared with FPs were less likely to report referring a parent to a smoking cessation program (30% vs. 41%; RP: 0.73; 95% CI: 0.58-0.94), giving pamphlets on smoking cessation (28% vs. 40%; RP: 0.7; 95% CI: 0.55-0.9), and asking for a quit date (18% vs. 41%; RP: 0.44; 95% CI: 0.33-0.6).
Kaplan et al.52 published in 2004 the results of a self-administered survey mailed to primary care physicians practicing in California (USA). The research team was the same that conducted the formerly mentioned study of Pérez-Stable.51 The objective was to compare the clinical practice of FPs and PEDs, relating to smoking cessation counseling in adolescents, as well as to determine the perceived barriers for this preventive activity in both types of professionals.
To be eligible, the physicians had to take care of patients under 18 years of age, to practice in primary care 10% of their working time, and to refer that at least 10% of their patients were children and adolescents. The sample was randomly selected from medical associations' registries. Of the original sample of 1,000 mailed surveys, 899 were eligible. 499 physicians (56%) returned completed questionnaires. The sample was further reduced to include only those physicians that have in their practices at least a 10% of patients aged 18 years and younger. This resulted in a final sample of 429 physicians for this report (187 FPs and 242 PEDs). In the multivariate logistic regression model analysis, FPs reported (more often than did it PEDs) setting a quit date (OR: 2.41; 95% CI: 1.08-5.4), scheduling a follow-up appointment to discuss quitting (OR: 3.07; 95% CI: 1.22-7.73), and directing the nursing staff to counsel the patient about quitting (OR: 3.7; 95% CI: 1.3-10.6). The authors did not found differences in other seven aspects related to tobacco cessation counseling.
Kolagotla et al.53 published in 2004 the results of a self administered survey mailed to primary care physicians practicing in USA. The aims of this study were to describe the ambulatory management of childhood obesity by pediatricians and family physicians, and to evaluate knowledge of published recommendations and the adherence to them. A random sample from the registries of professional associations was selected. Respondents self-identified as specialists, or physicians who spent less than 8 hours, or less than 25% of their working time in direct patient care, were excluded. Relating to the diagnosis, FPs were more likely to use body mass index (BMI) to identify obesity than PEDs (49% vs. 30%; p = 0.002). PEDs were significantly more likely than FPs to ask, in obese children, about a family history of dyslipidemia (76% vs. 62%; RP: 1.23; 95% CI: 1.01-1.51), to check blood pressure (99% vs. 93%; RP: 1.1; 95% CI: 1.01-1.19), to perform funduscopy (62% vs. 35%; RP: 1.85; 95% CI: 1.32-2.59) and to assess for dysmorphisms (66% vs. 33%; RP: 2.08; 95% CI: 1.46-2.97) and hirsutism (72% vs. 57%; RP: 1.3; 95% CI: 1.04-1.62).
PEDs were significantly more likely to report obtaining a dietary recall (71% vs. 56%; RP: 1.32; 95% CI: 1.05-1.66); obtaining records of television viewing and time spend playing video games (79% vs. 54%; RP: 1.51; 95% CI: 1.2-1.89), and requesting, as well, information about exercise and sports activity (98% vs. 88%; RP: 1.16; 95% CI: 1.05-1.29).
Cook et al.54 published in 2005 a study with the objective of examining clinician-reported diagnosis of obesity, as well as frequency of blood pressure assessment and diet and exercise counselling, during ambulatory visits made by children and adolescents in primary care offices of the USA. Whit this purpose the authors used the computerized registries of NAMCS and NHAMCS conducted in the years 1997 to 2000. Visits of patients, who were 2 to 18 years of age, were included and classified as having a diagnosis of obesity and other similar diagnosis, according to the international classification of diseases ICD-9. There were 32,930 total visits, 281 of them (0.78%) carried these diagnosis. Among well-child visits, the frequency of obesity diagnosis was 0.9%. Ninety-six point eight percent (96.8%) of well-child visits were provided by PEDs (vs. a 3.2% of FPs; RP: 8.49; 95% CI: 2.1-34.9). In the regression logistic analysis, PEDs provided diet counselling (OR: 2.5; 95% CI: 1.6-3.9) and exercise counselling (OR: 1.6; 95% CI: 1.0-2.7) more frequently than FPs.
Spurrier et al.55, in a study made in Australia, (survey mailed to family physicians and PEDs), approached the ability to recognize overweight and obese patients using the viewing of a series of body images and a questionnaire about them, as a tool to evaluate the criterion of the professional in rating the size of children ("acceptable weight", "overweight" and "obese"). The ability to rate this three situations correctly was similar (72% vs. 68%), for GPs and PEDs. The respondents were 44 out of 245 FPs and all the 29 PEDs surveyed. There were statistically significant differences in management, with PEDs performing closer to a local Clinical Practice Guideline on obesity.
Garg et al.56 published in 2007 a study with the objective to know and to compare the self-efficacy between PEDs and FPs in smoking cessation counselling. This study was considered of low quality. It was addressed in Pennsylvania (USA). Other objective was to evaluate whether an educational intervention, conducted at an office visit, can increase self-efficacy of both professionals. A convenience sample of primary care physicians were enrolled and received a one-time training session, which lasted 60 to 90 minutes, in order to improve the clinicians´ self-efficacy in smoking cessation counselling. A 4-point Likert scale was used to rate the level of self-confidence of the participants in the ability that they had acquired to provide this counseling. There were no differences between PEDs and FPs (3.54 vs. 3.38 points). The comparison of other items about post-educative intervention showed similar self-efficacy improvement in both professionals.
Other preventive activities
The delivery of other clinical preventive services, besides vaccination, as well as other health education activities, was assessed in six studies. Additional information on these services is shown in Table 8.
Lévêque et al.57 addressed a cross-sectional study in France (1995), conducting phone surveys among the three main groups of physicians who provide primary care to children: private practice PEDs, well-child clinic PEDs, and GPs. The objective of this study was to determine the level of counselling, in the subject of injury control, currently carried out by physicians. Three hundred private PEDs and 125 well-child clinic PEDs were randomly selected (French Committee on Health Education - FCHE); the sample size for GPs was not reported. The rate of non-responders varied in all three groups (17%, 11% and 40%, respectively). It is not possible to calculate some estimates that would allow the comparison among the three groups, due to the lack of general practitioners´ sample size. 97% of private practice PEDs, and 99% of well child clinic PEDs, answered that, providing counselling on injury prevention, was part of their professional duties. No GP answered this question. Fifty-seven percent of PEDs provided printed educational material on injury prevention in their offices vs. a 2% of GPs.
Steckler et al.58 performed a cross-sectional study implementing a survey to PEDs and FPs working in the influence area of three USA hospitals (New Jersey, Portland and Washington). They don´t describe the method used for the selection of the professionals. The objectives of the study were to compare the timing of orchidopexy in children with cryptorchidism in the three areas, as well as determine the attitudes and beliefs of 506 PEDs and 271 FPs on cryptorchidism. The rate of nonresponders was not reported. The mean age at orchidopexy was 4.2 years; there were no significative differences among the three centers. Relating to the adequate age to perform this intervention, 30% of PEDs (vs. a 14% of FPs) considered it to be recommendable between 6 and 12 months of age (p < 0.05). Ten percent of PEDs (vs. a 30% of FPs) considered waiting until 3-10 years. PEDs recommended orchidopexy at an earlier age than FPs (p < 0.05).
In the formerly mentioned study of Ewing38, in the multivariate analysis (reference category: FP), PEDs asked less frequently about exercise habits (OR: 0.62; p < 0.05) and also recommended physical exercise less frequently (OR: 0.71; p < 0.05). Relating to diet habits, PEDs asked usually about them more often than FPs (OR: 3.96; p < 0.05) and made recommendations more frequently (OR: 1.27; p < 0.05). FPs asked more about smoking (OR: 0.28; p < 0.05), and about alcohol and drugs use (OR: 0.49; p < 0.05) than PEDs did it. PEDs were more likely to report about seatbelt use (OR: 4.09; p < 0.05) and recommended it more frequently (OR: 3.24; p < 0.05). PEDs asked more about sexual activity (OR: 1.89; p < 0.05) and provided more counseling (OR: 1.77; p < 0.05).
FPs were more likely to ask about family planning (OR: 0.62; p < 0.05) and to deliver counsel in this field than PEDs (OR: 0.68; p < 0.05)
Gerard et al.59 compared the opinions and practices of FPs with those of PEDs regarding poison prevention. With this purpose a self-administered questionnaire was mailed to 500 PEDs and 500 FPs of 45 states of USA, randomly selected from AMA registries. Five hundred professionals answered (227 FPs and 273 PEDs). PEDs provided more printed material for unintentional poisoning prevention than GPs: pamphlets (56.8% vs. 32.2%; RP: 1.77; 95% CI: 1.42-2.19), warning stickers (34.1% vs. 20.7%; OR: 1.65; 95% CI: 1.21-2.23), posters in the office (27.5% vs. 11.5%; RP: 2.4; 95% CI: 1.59-3.61) and poison control center telephone numbers (68.5% vs. 38.3%; RP: 1.79; 95% CI: 1.49-2.15). The reason cited for not providing poison prevention anticipatory guidance was lack of training, and this was more likely in FPs (46.1% vs. 18.2%; p = 0.02). In the multivariate analysis, GPs were 5.4 times less likely to provide anticipatory guidance on unintentional poison prevention to parents than PEDs (OR: 0.19; 95% CI: 0.09-0.37).
Bocquet et al.16, in their already described study, stated that PEDs performed prevention against rickets with vitamin D more frequently than GPs (225% more), as well as more frequent fluoride teeth cavities prevention (261.7% more).
Horowitz et al.60 performed a study in New England (USA) (of low methodological quality) to assess the practices of PEDs and FPs on testicular self-examination recommendation. They mailed 458 questionnaires to PEDs and FPs. Two hundred and nine responded (45.6%), 141 PEDs and 68 FPs. There were no significant differences between both professionals on providing education about testicular cancer (RD: 0.6%; 95% CI: -12.5-13.8), on teaching testicular self-examination (RD: -3.97%; 95% CI: -17.3%-9.4%), or on making routine questions about testicular exploration in adolescents (RD: 4.3%; 95% CI: -9.8-18.5%).
Diagnostic tests
DTen studies performed some kind of comparison in this field of the clinical practice. Six had a cross-sectional design2,5,18,20,25,27 and four were cohort studies (one prospective29 and three historical cohort studies9,12,16). Further details of these studies are provided in Table 9.
In the paper of Fishbane2 the performance of both types of physicians was compared in some issues like the number of well-child visits made, the pathologies detected in them and the laboratory tests ordered. From more than 100,000 registered visits, PEDs labeled as well-child visits 31% of them, vs. a 18% of MFs/GPs (p < 0.05). The diagnosis made were similar for both types of professionals, although PEDs were more likely to make additional diagnosis in the well-child visits in all the ages groups (3-5 years: 26% vs. 0%, p < 0.01; 6-10 years: 27% vs. 0%, p < 0.05). There were no differences between both types of physicians regarding the percentage of radiograms ordered. When the causes of consultation were fever and sore-throat, PEDs ordered more laboratory tests (60% in sore-throat and 40% in presence of fever).
The study of Leduc et al.29 approaches the relative competence of PEDs and GPs in managing fever > 38 oC in children 0-10 years of age. PEDs ordered fewer roentgenograms than GPs (16 vs. 36; ARR: -9.9%; 95% CI: -9.4% to -0.4%). In children undergoing a roentgenogram, the probability of finding some pathology was superior among PEDs (7 out of 16 vs. 6 out of 36; RR: 2.6; 95% CI: 1.1-6.6). PEDs ordered a rapid strep test more frequently (28 vs. 2; RR: 18.7; 95% CI: 4.5-76.7), and it was positive more often if a PED ordered it (9 out of 28 vs. 0 out of 2; RD: 32.1%; 95% CI: 14.8-49.4). The results of cultures for pharyngeal streptococcus proved positive in 2 out of 28 ordered by PEDs vs. 0 out of 5 ordered by FPs/GPs (RD: 6.7%; 95% CI: -2.3%-15.6%).
In the study by Starfield,5 the authors stated that PEDs ordered more pharyngeal cultures for bacterial pharyngitis. Likewise, they ordered more audiometries than FPs and GPs.
In the already commented study by Schwartz et al.,18 FPs performed anterior rynoscopy more frequently than PEDs, without significant difference (RP: 1.1; 95% CI: 0.9-1.3), as well as more frequent leukocyte count in mucus extension (50 out of 138 vs. 42 out of 197; RP: 1.7; 95% CI: 1.2-2.4).
In the also mentioned study by Pennie et al.,9 there were no differences between FPs and PEDs in the rate of roentgenograms ordered in "RI" (Respiratory tract infections) (3%). FPs performed more diagnostic tests (not specified) than PEDs: 19% vs. 13% (RR: 1.48; 95% CI: 1.02-2.15).
In the study by Watson et al.20 FPs were significantly more likely than PEDs to omit pneumatic otoscopy (46% vs. 25%, RP: 0.4; 95% CI: 0.3-0.6) for the diagnosis of AOM and less likely to perform microbiological testing in acute pharyngitis (RP: 2.3, 95% CI: 1.4-3.8).
Finkelstein et al.27 compared in 1997 the degree of adherence, according to physician speciality, to the recommendations of the current, at that time, CPG of reference on asthma. They found no differences in the use of beta-2 inhaled-agonists trials (OR: 0.8, 95% CI: 0.2-3.9). FPs were less likely than PEDs to recommend daily peak flow measurement (36% vs. 54%, OR: 0.3; 95% CI: 0.1-0.5) or doctor´s office peak flow measurement (96% vs. 68%, OR: 3.95% CI: 0.8 to 10.8) and more likely to use spirometry in diagnosis (40% vs. 12%, OR: 5.9, 95% CI: 2.4 to 14.6). There were no differences between both groups according to the performance of chest or sinus x-ray, although there was a tendency for FPs to order them more frequently (thorax x-ray: 38% vs. 24%, OR: 1.7, 95% CI: 0.8 to 3.5, sinus x-ray: 10% vs. 1%, OR: 5.3, 95% CI: 0.6-44). There were no differences in the ordering of prick test or RAST (FPs 8% vs. 3% PEDs, OR: 1.2, 95% CI: 0.3-4.8).
In the survey by Boulis et al.,25 the authors used self-describing model patients with clinical presentations contrived to have multiple possible appropriate treatment plans. The first vignnete was a 10-year-old girl with a 3-day history of a temperature of 38.6 oC, productive cough, tachypnea, and rales at the right base. Physicians were asked for what percentage of such patients would they recommend a chest x-ray; PEDs would recommend it for 47.7% of the patients and FPs for 51.3% (mean percentage difference: -3.6%, 95% CI: -5.4 to -1.8). The second scenario was an otherwise healthy full-term 6-week-old infant with a temperature of 38 oC. Physicians were asked for what percentage of such patients would they recommend a sepsis workup, including at least a complete blood cell count, sterile urine, and blood cultures; 81.1% of PEDs compared with 66.4% of FPs would have recommended it (mean percentage difference: 14.7%, 95% CI: 13.2-16.1).
In the study by Bocquet et al.,16 the PEDs wrote fewer laboratory tests prescriptions (700 vs. 839, 16.6% less), including 53.0% less serum iron levels requests.
In Linder et al.12 Group A beta-haemolytic streptococcal (GABHS) testing was less used by non-pediatrician medical professionals, compared to PEDs (OR 0.46, 95% CI: 0.32-0.66).
Discussion
The results of this SR, despite the wide variety in terms of type of design and provenance between the included studies, show a common trend for supporting the presence of PEDs in primary care. It should be highlighted some specially important facts: a better pattern of drug prescription (less overall prescriptions and better adapted to the disease being treated, in regard to ATB prescription and to the use of other medications like psychotropic drugs); a more rational use of ancillary testing (e.g. chest x-ray, GABHS testing or oropharyngeal culture) and more abnormal results found in the test ordered; better and greater compliance with the main primary prevention activity (vaccination); and finally, a higher degree of compliance with the recommendations proposed by CPGs about diseases with high incidence and prevalence in children and adolescents.
The Pediatric Primary Care (PPC) is an essential public health issue. Therefore, the professionals chosen to perform it out should be those most qualified and trained to provide care to children and adolescents. Some factors to take into account when planning the PPC are the characteristics of each National Health System and the training received by the different medical specialists in each country. Although the characteristics, which in origin defined the new model of PC in Spain, converted the GP in a cornerstone for the entire health system, some other issues must be taken into account. In Spain, PEDs have been performing their professional work, both at hospital and in PC, prior to the1984 Health Reform, which introduced a new model of PC. When the reform was carried out, PC PEDs were integrated without any problem into the new PC teams. In Spain, therefore, the PC PED is a well appreciated and known professional.61 The figure of the general PED (PC PED or community PED) gives the possibility to the pediatric population to receive a specialized attention in the primary care health level, with important health benefits, as it has been shown in this study.
A study of Katz about PPC in the European Union6 provides food for thought. With the inherent methodological limitations of ecological studies, the author concluded that lower infant mortality is found when the PC PEDs are the professionals responsible of the children care in the community setting. Previously published studies on this subject in the eighties of the past century2,5 drew comparisons between physicians trained for assistance to the general population (FPs or GPs) and pediatric specialists, who at that time only received hospital training and worked at private consulting practices (PEDs of the years 1960-1980). Not surprising therefore that, in general, there were differences in drug prescription (such as a worse second line ATB use by PEDs, or an excessive use of ancillary testing). But it is no longer the same today, and there are countries where there are PEDS who work exclusively in PC and who receive specific training to do so. In Spain, the pediatric Speciality Training Program includes a 3-6 months rotation period in PPC. Moreover, most pediatric training programs in developed countries include aspects related to community and primary care practice.62-64
Among the different aspects analyzed by this SR, it should be stressed that the likelihood of prescribing ATBs, in probably viral respiratory tract infections (RI), was 1.1 to 1.8 times higher among non-PED PC physicians, compared to PEDs. Given the high incidence of these diseases in children, this finding may have significant impact on the pharmaceutical budget, on the generation of antimicrobial resistances and also in becoming a potential iatrogenic factor. Other publications which studied this aspect, and that have not been included in the meta-analysis (mostly self-completed surveys sent to professionals), give results pointing in the same direction. Of note is, that in the Bouquet et al. study,16 which compares various aspects of clinical practice between PEDs and FPs/GPs in France, geographically and culturally close to Spain: the PEDs prescribed 25% fewer ATBs than GPs.
Given the wide disparity in designs and locations of origin of the different studies, it is difficult to reach any conclusion on the use of second-line agents. Four studies were found (three conducted in the USA9,10,12 and one in Canada11), in two of them there was a better use by FPs9,11, in one by PEDs10 and not differences were found in the other one12. The variability in the design and characteristics of each country's health system could partially explain this finding.
CPGs are systematically developing statements to assist practitioner and patient in the decision making about appropriate health care for specific clinical circumstances65. Importantly, PEDs had better adherence to the recommendations of CPG for the treatment of high incidence acute conditions and high prevalence chronic diseases: RI, AOM, OME, fever, bronchial asthma, ADHD and overweight-obesity.11,14,22,23,30,33,53,55 Compliance with properly designed, updated and implemented GPCs, reduces unjustified heterogeneity in clinical practice among professionals. Specifically, PEDs have better compliance with AOM CPG recommendations about prescribing ATBs in a deferred way, instead of prescribe them immediately, as well as a better compliance with those other recommendations that advise to perform pneumatic otoscopy for the diagnosis of OME. They also refer less frequently these patients to the otorhinolaryngologist and prescribe fewer second-line agents and oral decongestants than GPs. In diseases with high incidence and prevalence, such as AOM and bronchial asthma, PEDs refer patients to the specialized attention level less frequently. These data suggest a higher resolution capacity of PEDs for diseases that pose a major economic and care burden for health systems.
Regarding the management of various psychiatric disorders, GPs were more likely to prescribe SSRIs for all the diseases studied. For some of them, these drugs are not indicated at all (enuresis, ADHD). The potential consequences of this pattern of prescription were not studied. In the case of ADHD, if the diagnosis is made correctly, it should be expected a lack of response to SSRI medication (being the first choice treatment for this disease, when indicated, central nervous system stimulants, specifically methylphenidate), resulting that, consequently, in harm to the child. Moreover, adverse effects of these drugs cannot be ruled out in children for whom they were not indicated in any way. A high degree of awareness of the recommendations of a CPG about the ADHD, and a better compliance with them by PEDs, reduce the possibility of inappropriate prescriptions to the patients affected by this disease, for which the prevalence in our area is estimated in the range between 5% and 8%.66
The attitudes among both types of professionals regarding immunizations deserve special consideration. Regardless the design of different studies, and whether those interviewed were doctors or parents, PEDs had higher rates of adherence with the official immunization calendars. They took advantage more frequently of acute illness visits for administering vaccines, had fewer assumptions about false hypothetical contraindications for immunization, were more likely to have a specific section at the medical record for registering immunization information and use more frequently systems to track undervaccinated children and adolescents. This is of paramount importance because immunization is the most effective primary prevention activity. Adequate implementation has achieved the global eradication of smallpox and the disappearance, in developed countries, of diseases like polio. There is agreement among the different identified studies that, if PEDs are responsible for this activity, it is carried out in a more complete way.
For other preventive activities, included under the term "cardiovascular risk", greater heterogeneity was found due to the different diseases and / or different unhealthy habits (smoking, inadequate diet) analyzed. The FPs/GPs had generally higher diet, smoking cessation and exercise counselling rates. Regarding the smoking cessation counselling, PEDs were more likely to record smoking by a parent, as a problem for the child but, then, they provided adequate alternatives for smoking cessation less frequently than the FPs/GPs did it. PEDs were more likely to order a cholesterol screening test when positive family history of hypercholesterolemia was noticed. In regard to overweight and obesity, PEDs, on average, performed closer to the CPG of reference at that time, and gave more frequently diet and exercise counselling. It could be concluded that FPs were more likely to perform preventive activities in the absence of overweight and obesity, but PEDs were more likely to detect obesity/overweight when present and to act with more determination to solve them. This should be taken with caution due to the wide heterogeneity found in the studies reviewed.
Regarding the provision of preventive services, it could also be concluded (with some exceptions) that there was an inverse relationship with age, giving that, the younger the patients, the greater the difference in favor of PEDs, by means of a better performance of this type of professional in providing more preventive services than GPs/FPs. For example, compared with the GPs/FPs, PEDs were more likely to asses seatbelt use, and to prescribe more vitamin D and dietary fluoride supplements for rickets and teeth cavities prevention in small children, but provided fewer preventive services involving family planning among adolescents.
Finally, among the studies that addressed the application of diagnostic tests, and going into specifics, PEDs performed fewer chest x-rays for children with fever, and when they ordered them, they were more likely to find pathology than FPs/GPs. The PEDs prescribed more GABHS testing, finding proportionally more positive results than FPs. The same happened with oropharyngeal culture results. In France, Bocquet16 observed that PEDs wrote fewer orders for laboratory tests in children.
This SR has several limitations. Perhaps the main one stems in the type of design of the studies recovered, mostly cross-sectional and carried out using self-administered questionnaires. A further limitation is the low response rates obtained in the surveys, a common bias in studies with this methodology. Noteworthy is that percentages of responders usually were not distributed equally between PEDs and FPs/GPs: happening in fact that PEDs responded more often. This may indicate a greater interest in the issues raised by this letters for this type of physicians (PED), but it may also indicate that those FPs/GPs who did respond, although they did it in a lower percentage in relation with PEDs, could be a subset of these professionals more interested in pediatric and adolescent health care. There are few analytical design studies, and no clinical trial, comparing the clinical practice of PEDs and FPs/GPs.
There is no tool to evaluate quality for cross-sectional studies, so in this SR it has been used for this purpose a critical appraisal tool for case series studies, adapted from the OSTEBA software (Basque Office for Health Technology Assessment, Department of Health and Consumer Affairs of the Basque Government) designed for analysing the quality of epidemiological studies (Ost FLC). We tried to minimize this problem by the commented adaptation. Each study was assessed independently by two reviewers. Disagreements were resolved by consensus. Finally, the meta-analysis results should be taken with caution because of the high degree of statistical heterogeneity (and, probably also, a high degree of clinical heterogeneity) between the studies included (variability in clinical practice between different countries, identification in every study of PED as the reference category, but heterogeneity in the definitions non-PED physician: GP, FP or other professionals), although most studies showed a statistically significant trend toward a higher likelihood to prescribe non indicated ATB treatment by GPs/FPs.
An additional limitation may have been that, in most of the included studies, the comparison between the clinical practice of PEDs and FPs/GPs was not the main outcome variable sought. In return, this could also be considered as strength, because in most studies the concern to the researchers was not to determine what type of professional provided better clinical services to children and adolescents. The objective of most of the studies was to assess the management of different health problems in primary care, by finding out how they were addressed. It is unlikely, therefore, the existence of conflicts of interest in favour of one or another specialty by the authors of the studies included in the review, who, besides, belonged to different categories: PEDs, FPs/GPs and, in many cases, public health professionals. This scenario, with a more than possible absence of conflicts of interest on the part of the authors, provides more strength to the results of this review.
No cost analysis study was identified in the conducted search, comparing the clinical practice between PEDs and FPs/GPs. However, the assessed data suggest that the health care provided by PEDs in PC could be cost saving for those health systems which have PEDs in their primary care settings.
This one is the first SR that compares clinical practice between PEDs and FPs/GPs in PPC (Pediatric Primary Care). As the main conclusion of this study, evidence seems to show that in developed countries, the PPC provided by PEDs, has better rates of adherence to the established immunization programs and better observance of the recommendations from the CPGs of reference about diseases of high incidence and high prevalence, being all that this way, always in comparison with FPs/GPs. Most of the results obtained (proper use of medications, better compliance with recommendations of the CPGs, better fulfilment of the official immunization calendars and lower percentages of referrals to the specialist level) were studied in outcome variables of great importance for physicians, patients and health service managers, since small variations in the provision of those care services can have enormous impact. With these findings in mind, it seems to be recommendable to maintain the PED in the PC teams, and to strengthen their specific role as the children´s first contact point with the health system.
Several implications for further research can be drawn from this review. There is a need for observational studies (cohort or case control) in which differences in clinical practice between PEDs and GPs should be compared in specific areas such as drug prescription, institutional CPG implementation, and the percentage of referrals to emergency department or specialized attention.
Bibliografía
1. Ferris TG, Saglam D, Stafford RS, Causino N, Starfield B, Culpepper L et al. Changes in the daily practice of primary care for children. Arch Pediatr Adolesc Med. 1998;152:227-33. [ Links ]
2. Fishbane M, Starfield B. Child health care in the United States: a comparison of pediatricians and general practitioners. N Engl J Med. 1981;305: 552-6. [ Links ]
3. Freed GL, Nahra TA, Wheeler JR. Which physicians are providing health care to America´s children? Trends and changes during the past 20 years. Arch Pediatr Adolesc Med. 2004;158:22-6. [ Links ]
4. Phillips Jr RL, Bazemore AW, Dodoo MS, Shipman SA, Green LA. Family physicians in the child health care workforce: opportunities for collaboration in improving the health of children. Pediatrics. 2006;118:1200-6. [ Links ]
5. Starfield B, Hoekelman RA, McCormick M, Mendenhall RD, Moynihan C, Benson P et al. Styles of care provided to children in the United States: a comparison by physician specialty. J Fam Pract. 1985;21:133-8. [ Links ]
6. Katz M, Rubino A, Collier J, Rosen J, Ehrich JH. Demography of pediatric primary care in Europe: delivery of care and training. Pediatrics. 2002; 109:788-96. [ Links ]
7. Rotaeche del Campo R, Vicente Anza D, Mozo Avellaneda C, Etxeberria Agirre A, López Navares L, Olasagasti Caballero C et al. Idoneidad de la prescripción antibiótica en atención primaria en la Comunidad Autónoma Vasca. Aten Primaria. 2001;27:642-8. [ Links ]
8. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875-7. [ Links ]
9. Pennie RA. Prospective study of antibiotic prescribing for children. Can Fam Physician. 1998; 44:1850-6. [ Links ]
10. Nash DR, Harman J, Wald ER, Kelleher KJ. Antibiotic prescribing by primary care physicians for children with upper respiratory tract infections. Arch Pediatr Adolesc Med. 2002;156: 1114-9. [ Links ]
11. Kozyrskyj AL, Dahl ME, Chateau DG, Mazowita GB, Klassen TP, Law BJ. Evidence-based prescribing of antibiotics for children: role of socioeconomic status and physician characteristics. CMAJ. 2004;171:139-45. [ Links ]
12. Linder JA, Bates DW, Lee GM, Finkelstein JA. Antibiotic treatment of children with sore throat. JAMA. 2005;294:2315-22. [ Links ]
13. Hare ME, Gaur AH, Somes GW, Arnold SR, Shorr RI. Does it really take longer not to prescribe antibiotics for viral respiratory tract infections in children? Ambul Pediatr. 2006;6:152-6. [ Links ]
14. Kozyrskyj AL, Dahl ME, Ungar WJ, Becker AB, Law BJ. Antibiotic treatment of wheezing in children with asthma: what is the practice? Pediatrics. 2006;117:e1104-10. [ Links ]
15. Mainous 3rd AG, Hueston WJ, Love MM. Antibiotics for colds in children: who are the high prescribers? Arch Pediatr Adolesc Med. 1998;152: 349-52. [ Links ]
16. Bocquet A, Chalumeau M, Bollotte D, Escano G, Langue J, Virey B. Comparison of prescriptions by pediatricians and general practitioners: a population-based study in Franche-Comté from the database of Regional Health Insurance Fund. Arch Pediatr. 2005;12:1688-96. [ Links ]
17. Roark R, Petrofski J, Berson E, Berman S. Practice variations among pediatricians and family physicians in the management of otitis media. Arch Pediatr Adolesc Med. 1995;149:839-44. [ Links ]
18. Schwartz RH, Freij BJ, Ziai M, Sheridan MJ. Antimicrobial prescribing for acute purulent rhinitis in children: a survey of pediatricians and family practitioners. Pediatr Infect Dis J. 1997;16:185-90. [ Links ]
19. Davy T, Dick PT, Munk P. Self-reported prescribing of antibiotics for children with undifferentiated acute respiratory tract infections with cough. Pediatr Infect Dis J. 1998;17:457-62. [ Links ]
20. Watson RL, Dowell SF, Jayaraman M, Keyserling H, Kolczak M, Schwartz B. Antimicrobial use for pediatric upper respiratory infections: reported practice, actual practice, and parent beliefs. Pediatrics. 1999;104:1251-7. [ Links ]
21. Arnold SR, To T, McIsaac WJ, Wang EE. Antibiotic prescribing for upper respiratory tract infection: the importance of diagnostic uncertainty. J Pediatr. 2005;146:222-6. [ Links ]
22. Vernacchio L, Vezina RM, Mitchell AA. Management of acute otitis media by primary care physicians: trends since the release of the 2004 American Academy of Pediatrics/American Academy of Family Physicians clinical practice guideline. Pediatrics. 2007;120:281-7. [ Links ]
23. Quach C, Collet JP, Le Lorier J. Acute otitis media in children: a retrospective analysis of physician prescribing patterns. Br J Clin Pharmacol. 2004;57:500-5. [ Links ]
24. McIsaac WJ, Coyte P, Croxford R, Harji S, Feldman W. Referral of children with otitis media. Do family physicians and pediatricians agree? Can Fam Physician. 2000;46:1780-2. [ Links ]
25. Boulis AK, Long J. Variation in the treatment of children by primary care physician specialty. Arch Pediatr Adolesc Med. 2002;156:1210-5. [ Links ]
26. Asher E, Leibovitz E, Press J, Greenberg D, Bilenko N, Reuveni H. Accuracy of acute otitis media diagnosis in community and hospital settings. Acta Paediatr. 2005;94:423-8. [ Links ]
27. Finkelstein JA, Lozano P, Shulruff R, Inui TS, Soumerai SB, Ng M et al. Self-reported physician practices for children with asthma: are national guidelines followed? Pediatrics. 2000;106:886-96. [ Links ]
28. Sun HL, Kao YH, Chou MC, Lu TH, Lue KH. Differences in the prescription patterns of anti-asthmatic medications for children by pediatricians, family physicians and physicians of other specialties. J Formos Med Assoc. 2006;105:277-83. [ Links ]
29. Leduc DG, Pless IB. Pediatricians and general practitioners: a comparison of the management of children with febrile illness. Pediatrics. 1982;70: 511-5. [ Links ]
30. Zerr DM, Del Beccaro MA, Cummings P. Predictors of physician compliance with a published guideline on management of febrile infants. Pediatr Infect Dis J. 1999;18:232-8. [ Links ]
31. Rushton JL, Clark SJ, Freed GL. Primary care role in the management of childhood depression: a comparison of pediatricians and family physicians. Pediatrics. 2000;105:957-62. [ Links ]
32. Rushton JL, Clark SJ, Freed GL. Pediatrician and family physician prescription of selective serotonin reuptake inhibitors. Pediatrics. 2000;105:e82. [ Links ]
33. Rushton JL, Fant KE, Clark SJ. Use of practice guidelines in the primary care of children with attention-deficit/hyperactivity disorder. Pediatrics. 2004;114:e23-8. [ Links ]
34. Freed GL, Bordley WC, Clark SJ, Konrad TR. Universal hepatitis B immunization of infants: reactions of pediatricians and family physicians over time. Pediatrics. 1994;93:747-51. [ Links ]
35. Szilagyi PG, Rodewald LE, Humiston SG, Hager J, Roghmann KJ, Doane C et al. Immunization practices of pediatricians and family physicians in the United States. Pediatrics. 1994;94:517-23. [ Links ]
36. Freed GL, Kauf T, Freeman VA, Pathman DE, Konrad TR. Vaccine-associated liability risk and provider immunization practices. Arch Pediatr Adolesc Med. 1998;152:285-9. [ Links ]
37. Ipp M, Macarthur C, Winders P, Gold R. Influenza vaccination of high-risk children: a survey of three physician groups. Can J Public Health. 1998;89:415-8. [ Links ]
38. Ewing GB, Selassie AW, López CH, McCutcheon EP. Self-report of delivery of clinical preventive services by U.S. physicians. Comparing specialty, gender, age, setting of practice, and area of practice. Am J Prev Med. 1999;17:62-72. [ Links ]
39. Santoli JM, Rodewald LE, Maes EF, Battaglia MP, Coronado VG. Vaccines for Children program, United States, 1997. Pediatrics. 1999;104: e15. [ Links ]
40. Takayama JI, Iser JP, Gandelman A. Regional differences in infant immunization against hepatitis B: did intervention work? Prev Med. 1999;28:160-6. [ Links ]
41. Ehresmann KR, Mills WA, Loewenson PR, Moore KA. Attitudes and practices regarding varicella vaccination among physicians in Minnesota: implications for public health and provider education. Am J Public Health. 2000;90:1917-20. [ Links ]
42. Kahane SM, Watt JP, Newell K, Kellam S, Wight S, Smith NJ et al. Immunization levels and risk factors for low immunization coverage among private practices. Pediatrics. 2000;105:e73. [ Links ]
43. LeBaron CW, Massoudi M, Stevenson J, Lyons B. Vaccination coverage and physician distribution in the United States, 1997. Pediatrics. 2001; 107:e31-9. [ Links ]
44. Schaffer SJ, Humiston SG, Shone LP, Averhoff FM, Szilagyi PG. Adolescent immunization practices: a national survey of US physicians. Arch Pediatr Adolesc Med. 2001;155:566-71. [ Links ]
45. Cohen NJ, Lauderdale DS, Shete PB, Seal JB, Daum RS. Physician knowledge of catch-up regimens and contraindications for childhood immunizations. Pediatrics. 2003;111:925-32. [ Links ]
46. Davis MM, Ndiaye SM, Freed GL, Kim CS, Clark SJ. Influence of insurance status and vaccine cost on physicians´ administration of pneumococcal conjugate vaccine. Pediatrics. 2003;112:521-6. [ Links ]
47. Posfay-Barbe KM, Heininger U, Aebi C, Desgrandchamps D, Vaudaux B, Siegrist CA. How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics. 2005;116:e623-33. [ Links ]
48. Franzgrote M, Ellen JM, Millstein SG, Irwin Jr CE. Screening for adolescent smoking among primary care physicians in California. Am J Public Health. 1997;87:1341-5. [ Links ]
49. Kimm SY, Payne GH, Stylianou MP, Waclawiw MA, Lichtenstein C. National trends in the management of cardiovascular disease risk factors in children: second NHLBI survey of primary care physicians. Pediatrics. 1998;102:e50. [ Links ]
50. Klein JD, Levine LJ, Allan MJ. Delivery of smoking prevention and cessation services to adolescents. Arch Pediatr Adolesc Med. 2001;155: 597-602. [ Links ]
51. Pérez-Stable EJ, Juárez-Reyes M, Kaplan C, Fuentes-Afflick E, Gildengorin V, Millstein S. Counseling smoking parents of young children: comparison of pediatricians and family physicians. Arch Pediatr Adolesc Med. 2001;155:25-31. [ Links ]
52. Kaplan CP, Pérez-Stable EJ, Fuentes-Afflick E, Gildengorin V, Millstein S, Juárez-Reyes M. Smoking cessation counseling with young patients: the practices of family physicians and pediatricians. Arch Pediatr Adolesc Med. 2004;158:83-90. [ Links ]
53. Kolagotla L, Adams W. Ambulatory management of childhood obesity. Obes Res. 2004; 12:275-83. [ Links ]
54. Cook S, Weitzman M, Auinger P, Barlow SE. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116:112-6. [ Links ]
55. Spurrier NJ, Magarey A, Wong C. Recognition and management of childhood overweight and obesity by clinicians. J Paediatr Child Health. 2006;42:411-8. [ Links ]
56. Garg A, Serwint JR, Higman S, Kanof A, Schell D, Colon I, et al. Self-efficacy for smoking cessation counseling parents in primary care: an office-based intervention for pediatricians and family physicians. Clin Pediatr. 2007;46:252-7. [ Links ]
57. Lévêque B, Baudier F, Janvrin MP. The contribution of physicians to childhood injury prevention in France. Inj Prev. 1995;1:155-8. [ Links ]
58. Steckler RE, Zaontz MR, Skoog SJ, Rushton Jr HG. Cryptorchidism, pediatricians, and family practitioners: patterns of practice and referral. J Pediatr. 1995;127:948-51. [ Links ]
59. Gerard JM, Klasner AE, Madhok M, Scalzo AJ, Barry RC, Laffey SP. Poison prevention counseling: a comparison between family practitioners and pediatricians. Arch Pediatr Adolesc Med. 2000;154:65-70. [ Links ]
60. Horowitz AL, Reinert S, Caldamone AA. Teaching testicular self-examination in the pediatric outpatient setting: a survey of pediatricians and family doctors. Med Health R I. 2006;89:370-1, 375-6. [ Links ]
61. AEPap. El modelo de atención al niño. Rev Pediatr Aten Primaria. 2005;7:549-56. [ Links ]
62. Crouchman M, Pechevis M, Sandler B. Social paediatrics and child public health: a European perspective. Arch Dis Child. 2001;84:299-301. [ Links ]
63. Domínguez Aurrecoechea B, Orejón de Luna G, Martín Muñoz P, García Puga JM, Grupo Docencia MIR de la AEPap. La formación MIR de Pediatría también desde la Atención Primaria. Rev Pediatr Aten Primaria. 2005;7 (Supl 1):s97-s134. [ Links ]
64. Future of pediatric education II (fope II) project members. The Future of Pediatric Education II: Organizing Pediatric Education to Meet the Needs of Infants, Children, Adolescents, and Young Adults in the 21st Century. Pediatrics. 2000;105:163-212. [ Links ]
65. Field MJ, Lohr KN, editors. Institute of Medicine Committee to Advise the Public Health Service on Clinical Practice Guidelines. Clinical Practice Guidelines: directions for a new program. Washington, DC: National Academy Press; 1990. [ Links ]
66. Rodríguez Molinero L, López Villalobos JA, Garrido Redondo M, Sacristán Martín AM, Martínez Rivera MT, Ruiz Sanz F. Estudio psicométrico-clínico de prevalencia y comorbilidad del trastorno por déficit de atención con hiperactividad en Castilla y León (España). Rev Pediatr Aten Primaria. 2009;11:251-70. [ Links ]
![]() Correspondence:
Correspondence:
J.C Buñuel,
jcbunuel@gmail.com