Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.6 nov./dic. 2006
Lepromatous leprosy: A review and case report
Lepra lepromatosa: Revisión y caso clínico
Eduardo Chimenos Küstner 1, Montserrat Pascual Cruz 2, Cristina Piñol Dansis 3, Helena Viñals Iglesias4,
Mª Eugenia Rodríguez de Rivera Campillo 5, José López López 1
(1) Médico estomatólogo. Profesor Titular de Medicina Bucal, Facultad de Odontología, Universidad de Barcelona
(2) Médico estomatóloga. Profesora Asociada de la Facultad de Medicina de la Universidad Autónoma de Barcelona
(3) Diplomada en Trabajo Social, Área Básica de Salud (ABS) de Sant Roc (Badalona, Barcelona)
(4) Médico estomatóloga. Profesora Asociada de Medicina Bucal, Facultad de Odontología, Universidad de Barcelona
(5) Médico dermatóloga y Odontóloga. Profesora Asociada de Medicina Bucal, Facultad de Odontología, Universidad de Barcelona
ABSTRACT
Leprosy is a contagious and chronic systemic granulomatous disease caused by Mycobacterium leprae (Hansens bacillus). It is transmitted from person to person and has a long incubation period (between two and six years). The disease presents polar clinical forms (the "multibacillary" lepromatous leprosy and the "paucibacillary" tuberculoid leprosy), as well as other intermediate forms with hybrid characteristics. Oral manifestations usually appear in lepromatous leprosy and occur in 20-60% of cases. They may take the form of multiple nodules (lepromas) that progress to necrosis and ulceration. The ulcers are slow to heal, and produce atrophic scarring or even tissue destruction. The lesions are usually located on the hard and soft palate, in the uvula, on the underside of the tongue, and on the lips and gums. There may also be destruction of the anterior maxilla and loss of teeth. The diagnosis, based on clinical suspicion, is confirmed through bacteriological and histopathological analyses, as well as by means of the lepromin test (intradermal reaction that is usually negative in lepromatous leprosy form and positive in the tuberculoid form). The differential diagnosis includes systemic lupus erythematosus, sarcoidosis, cutaneous leishmaniasis and other skin diseases, tertiary syphilis, lymphomas, systemic mycosis, traumatic lesions and malignant neoplasias, among other disorders. Treatment is difficult as it must be continued for long periods, requires several drugs with adverse effects and proves very expensive, particularly for less developed countries. The most commonly used drugs are dapsone, rifampicin and clofazimine. Quinolones, such as ofloxacin and pefloxacin, as well as some macrolides, such as clarithromycin and minocyclin, are also effective. The present case report describes a patient with lepromatous leprosy acquired within a contagious family setting during childhood and adolescence.
Key words: Mycobacterium leprae, lepromatous leprosy, tuberculoid leprosy, differential diagnosis.
RESUMEN
La lepra es una enfermedad granulomatosa sistémica crónica y contagiosa, producida por Mycobacterium leprae (bacilo de Hansen). Se transmite de persona a persona y tiene un largo período de incubación (entre 2 y 6 años). Existen dos formas clínicas polares: lepra lepromatosa (multibacilar) y lepra tuberculoide (paucibacilar), con otras formas intermedias de características híbridas. Las manifestaciones orales suelen aparecer en la lepra lepromatosa y se producen en el 20 al 60% de los casos. Pueden tratarse de nódulos múltiples (lepromas), que progresan a necrosis y ulceración. Las úlceras curan con lentitud; forman cicatrices atróficas o pueden causar la destrucción del tejido. Las lesiones suelen localizarse en el paladar duro y blando, en la úvula, en el dorso de la lengua, en los labios y en las encías. También puede producirse destrucción de la parte frontal del maxilar y pérdida de dientes. El diagnóstico, basado en la presunción clínica, se completa con el examen bacteriológico e histopatológico, así como mediante la prueba de la lepromina (intradermorreacción que suele ser negativa en la forma lepromatosa y positiva en la tuberculoide). El diagnóstico diferencial incluye lupus eritematoso sistémico, sarcoidosis, leishmaniasis cutánea y otras enfermedades de la piel, sífilis terciaria, linfomas, micosis sistémicas, lesiones traumáticas y neoplasias malignas, entre otras. El tratamiento es difícil, ya que ha de prolongarse durante mucho tiempo, requiere varios fármacos con efectos adversos y resulta muy caro, sobre todo para los países menos desarrollados. Los de empleo más frecuente son la dapsona, la rifampicina y la clofazimina. También son eficaces las quinolonas, como ofloxacino y pefloxacino, así como algunos macrólidos, como la claritromicina y la minociclina. En el presente trabajo se expone el caso clínico de un paciente afecto de lepra lepromatosa, adquirida en un ambiente familiar de contagio durante la infancia y adolescencia.
Palabras clave: Mycobacterium leprae, lepra lepromatosa, lepra tuberculoide, diagnóstico diferencial.
Introduction
Leprosy is a contagious and chronic systemic granulomatous disease caused by Mycobacterium leprae (Hansens bacillus). It is transmitted from person to person and has a long incubation period (between two and six years). The mycobacterium has a preference for peripheral tissue, as it appears to survive better at a temperature close to 30ºC rather than 37ºC. Hence it affects the skin, peripheral nerves, the mucosa of the upper airways and other tissues such as bone and some viscera (1-3). The disease presents polar clinical forms (the "multibacillary" lepromatous leprosy and the "paucibacillary" tuberculoid leprosy), as well as other intermediate forms with hybrid characteristics (Table 1). Oral manifestations usually appear in lepromatous leprosy and occur in 20-60% of cases. They may take the form of multiple nodules (lepromas) that progress to necrosis and ulceration.
The ulcers are slow to heal, and produce atrophic scarring or even tissue destruction. The lesions are usually located on the hard and soft palate, in the uvula, on the underside of the tongue, and on the lips and gums. There may also be destruction of the anterior maxilla and loss of teeth (1,2,4,5). The diagnosis, based on clinical suspicion, is confirmed through bacteriological and histopathological analyses (in which non-caseating granulomas are observed), as well as by means of the lepromin test (intradermal reaction that is usually negative in lepromatous leprosy form and positive in the tuberculoid form) (6). The differential diagnosis includes systemic lupus erythematosus, sarcoidosis, cutaneous leishmaniasis and other skin diseases, tertiary syphilis, cicatricial pemphigoid, lethal midline granuloma, lymphomas, systemic mycosis, traumatic lesions and malignant neoplasias, as well as peripheral nerve pathology such as syringomyelia, among other disorders (2,6).
Treatment is difficult as it must be continued for long periods, requires several drugs with adverse effects and proves very expensive, particularly for less developed countries. The most commonly used drugs are dapsone, rifampicin and clofazimine. Quinolones, such as ofloxacin and pefloxacin, as well as some macrolides, such as clarithromycin and minocyclin are also effective (6).
Evolution of the disease: Patients with lepromatous leprosy are highly infectious, although most exposed immunocompetent individuals do not contract the disease. Around one-third of people with leprosy present the first clinical manifestations during childhood. The incubation period of the disease may last up to six years. Once signs have appeared the disease will generally progress slowly unless treated. Its preference for cooler anatomical regions means that vital organs are usually preserved, but also makes leprosy a disease that slowly destroys the distal areas of fingers and toes and causes nasal and facial deformities that lead to social marginalization. Local pyogenic infections, secondary to skin ulcers, complicate and exaggerate these alterations. Despite these problems the tendency of the disease to preserve the main viscera means that life expectancy is barely reduced. Certain complications, such as pyogenic infection with abscess formation and sepsis, may produce an abrupt and fatal change in the disease course.
Although the disease is uncommon in our milieu the rising immigration of recent years is good reason to take it into consideration. Therefore, it seemed of interest to review the topic by means of a highly representative clinical case.
Case report
Male patient aged 65 with no known allergies; he smokes twenty cigarettes a day and has a history of moderate alcohol abuse. He attended a long-stay unit during the summer of 2005 for a limited period (two months) in order to provide family respite.
Family history:
Leprous family environment, in which the patients mother and three older siblings suffered from lepromatous leprosy, of similar presentation to that in the present report; all these relatives are now dead. This history does not seem to have affected the father or the patients younger sister, who are still alive.
Pathological history:
- Lepromatous leprosy diagnosed forty years previously. Multiple amputations (bilateral metacarpophalangeal, left metatarsophalangeal and nose due to relapsing infection of the septum, performed during the active phase of the disease) (Figure 1) secondary to the leprous infection. Without anti-leprosy treatment since 1994 (due to negativization).
- Type II diabetes mellitus, which debuted in 1994. This is treated with NPH insulin. Presence of retinopathy, nephropathy and dysautonomia.
- He presented a secondary bilateral amaurosis (leukocoria).
- In 2001 he suffered an important dysphagia, which was diagnosed as oesophageal stenosis, possibly due to gastroesophageal regurgitation (of peptic origin).
- GGT and AP enzyme levels were elevated on the usual tests, which also revealed a microcytic anaemia. He was a carrier of the hepatitis C virus (HCV).
Current disease status:
General physical examination showed the patient to be conscious and oriented. His skin was dry, pale and sclerotic. No adenopathies were palpated. The bilateral amaurosis and hypoacusia were noted. He also had problems swallowing and presented solid and liquid dysphagia. He had spontaneous mobility of the extremities, where examination revealed the amputation of fingers and toes of the left foot, as well as the supracondylar amputation of the right lower extremity. There were suppurating ulcers on the right trochanter and at the head of the left fibula. He suffered from protein-energy malnutrition. He lives with his wife, a daughter and five grandchildren. He is being monitored by his general practitioner and receives domiciliary care for his left knee lesions and diabetes.
Facial and oral examination:
- Total facial deformation as a result of the lepromatous lesions and amputation of the nose: leonine facies (Figure 1).
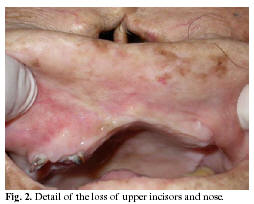
- Numerous smooth perioral, hyperpigmented, polymorphous and poorly defined skin lesions were observed, and these invaded the lip vermillion and disappeared at the intraoral mucosa. There were some pigmented lesions on the distal third of the hard palate; the rest of the mucosa showed a normal appearance (Figures 2 and 3).
- The patient was sensitive to touch on all the mucosa and no subcutaneous granulomas were noted.
- The nasal septum was perforated, but there was no palate perforation or destruction of the soft parts (uvula, tongue, etc.).
- His dental health was very poor and revealed multiple caries and root remains, missing teeth (upper arcade practically edentulous) and gingivitis due to accumulation of bacterial plaque secondary to poor hygiene, which was partly determined by the amputations of the extremities.
The patients quality of life was determined by his domiciliary situation and low socioeconomic status. This presented an obstacle in terms of following an adequate dental treatment.
Laboratory tests:
Blood tests upon admission corroborated the anaemic state and the hepatic and renal alterations indicated previously. Secretion cultures from the ulcers on the lower extremities (right trochanter and head of the left fibula) were positive for Staphylococcus aureus.
Treatment plan upon discharge:
Administration of paracetamol, haloperidol, NPH insulin and rohypnol. Diet to include carbohydrate monitoring and dietary supplements. The diabetes and anaemia to be monitored by the general practitioner, and the hepatopathy by a digestive specialist. Domiciliary care to be arranged for treating the ulcers. He was advised to see a dental specialist in order to have the root remains removed, and it was explained to him that having full dental prostheses (upper and lower) fitted would help restore his masticatory function.
Discussion
- Facial alterations: Lepromatous leprosy usually begins in the form of chronic rhinitis. The symptoms are often so non-specific that the disease is not suspected prior to the appearance of skin lesions. The nasal mucosa become ulcerated and form scabs. These lesions sometimes bleed to the extent that medical attention is required. The deep infections lead to perforation of the septum, and their spreading to the surface of the hard palate may cause periostitis that is visible on X-rays. From the clinical point of view the greater evidence of pathology appears when the nasal bones, the nasal spine and even the midline maxillary region become affected; the erosion or complete destruction of the latter leads to tissue collapse, with sinking and spreading of the overlying skin and other soft tissues (saddle nose). This external soft tissue deformity constitutes one of the main facial alterations seen in patients with leprosy (1). The nasal secretions are literally teeming with leprous bacilli, and hence airborne dissemination, via sneezing, would seem to be the most likely way for leprosy to be spread nowadays. This rhinomaxillary syndrome only corresponds to the lepromatous form of leprosy (7), which is that suffered by the patient described here (Figure 1) and, most likely, was what affected his close relatives. At some undetermined point the patient suffers an initial bacillaemia, which may be repeated through recurrent episodes or progress toward a continuous bacteraemia. Multiple organs are exposed to the bacilli during these episodes. The circulating bacteria are so abundant that they can be detected in peripheral blood samples. However, those which settle in the internal organs are usually effectively eliminated by macrophages. As these bacteria multiply more in cooler areas the pattern of infection is usually focussed on the skin, superficial cutaneous structures (especially peripheral nerves), the eyes and the testicles. The facial skin shows areas of localized swelling, with deep furrows between them. The resulting nodules may become ulcerated. The swollen upper eyelids create a sleepy appearance and the repercussions in the supraorbital tissues usually lead to the loss of eyebrow hair, particularly in lateral areas. The subsequent damage to the sclera and iris may produce blindness. This nodular dermal appearance, often referred to as leonine facies, is another facial deformity characteristic of leprosy (1,8). The patient reported here suffered both bilateral blindness and leonine facies (Figure 1). Lepromatous rhinitis may spread to the maxilla and be complicated by secondary pyogenic infections. Beginning at the midline, the maxillary bone begins to erode to the extent that the palate becomes perforated. This leads to loss of periodontal support for the upper middle incisors, which eventually fall out. In very advanced cases this process may spread to the sides and even reach the canine teeth. This loss of maxillary bone structures and teeth constitutes another characteristic facial alteration in leprosy (4), which in the case of our patient contributed to the leonine appearance of the lip (Figure 2).
- Nerve lesions: The peripheral nerves are usually affected by the bacillus in lepromatous leprosy. A hard and rigid irregular nerve trunk is sometimes observed in the more superficial areas of the elbow (cubital nerve) or at the head of the fibula (peroneal nerve). However, the absence of a granulomatous form or inflammatory response reduces the tissue destruction characteristic of the tuberculoid form. Hence the leprous bacilli may form large clusters in the nerve sheath, and in some patients this may at first lead to hyperaesthesia. The persistence of the bacteria and the subsequent destruction of nerve fibres are the cause of anaesthesia in hands and feet (1,9). This was not the case of the patient reported here, who maintained sensitivity.
- Skin lesions: In addition to the facial lesions described above it is common to find multiple skin macules in cooler areas of the body (extremities, buttocks). These are hypopigmented in dark-skinned people and erythematous in those with light skin. Their border is much less defined than in the tuberculoid form of leprosy. Although the trunk may be affected, few lesions are generally observed in this region (1). Our patient showed generalized changes in pigmentation, as can be seen in the figures.
- Bone lesions: In only 5% of hospitalized patients are the bones directly invaded by the bacilli. This invasion usually occurs indirectly, via lesions in the surrounding soft tissues or, less often, via the blood. In other cases the bone involvement is secondary to peripheral neuropathy. The skin areas anaesthetised by the nerve infection are susceptible to tissue infection. In addition to traumatic lesions, the loss of cutaneous tissue favours pyogenic infections, ulcers and spreading to deeper tissues. This leads to arthritis and septic osteomyelitis of non-leprous origin, accompanied by bone destruction and compromised movement due to muscular paralysis (also secondary to nerve the damage), which results in osteoporosis and bone atrophy. The phalanx and metacarpal or metatarsal bones are often affected, with marked shortening that may leave only a stump (1).
- Immunology: The clinical forms of leprosy depend heavily on the patients immunological state, which can be determined by the lepromin test (Mitsuda and Hayashi test). This consists in the intradermal injection of lepromin (extract of the leprous bacillus taken from sick patients). It is usually negative in lepromatous leprosy and positive in the tuberculoid form. However, as positive results are also obtained in patients without leprosy this test only serves to assess the immunological state in already-diagnosed patients (1,6). Leprous patients with a positive Mitsuda reaction usually present a histological tissue reaction similar to that found in tuberculosis, and hence the name give to this clinical form is tuberculoid leprosy. The lepromin reaction and histology indicate that these patients show a cell-mediated immune response, or delayed hypersensitivity, as occurs in tuberculosis. As few bacilli are found in the lesions of this clinical form it is known as paucibacillary. It is believed that these patients are much less contagious than those with lepromatous leprosy (1,6). In contrast, patients with a negative Mitsuda reaction show minimal resistance to the action of mycobacteria, which grow in a relatively unrestricted fashion and form large bacterial clusters that prove to be highly infectious. This multibacillary clinical form is known as lepromatous leprosy. Laboratory studies suggest there to be a defective T-cell response to the antigens of M. leprae (10) and other micro-organisms (11). The reason for the different immune response of the two clinical forms remains unclear. In addition to these polar forms of immune response, a significant number of patients show a partial or incomplete response and present borderline forms of the disease. In 1980, the WHO attempted to describe these degrees of semi-quantitative response, designating them as borderline tuberculoid (BT) and borderline lepromatous (BL) (12). Although the position of a given patient on this spectrum is relatively stable the immune response which characterises tuberculoid leprosy may deteriorate in untreated patients, especially in those who suffer malnutrition or other infections (13). Under these circumstances the clinical form begins to acquire certain lepromatous characteristics, with aspects of BL, the intermediate form or, more rarely, BT. It is very rare for the reverse trend to be observed spontaneously, and it is only seen in treated patients (1).
- Interactions between leprosy and tuberculosis: The antibodies produced by a given bacterial species may be capable of combining with membrane receptors of other species. This notion of cross reactions is not unique, although it is better documented in examples of humoral rather than cell immunity. It is clear that the patients immune state is of key importance as regards the clinical manifestations of leprous infection and plays a role in the relationship between leprosy and tuberculosis. Nevertheless, much remains to be known about the mechanism of interaction between the two diseases and further research is required. Although both leprosy and tuberculosis were more common in the past they have never completely disappeared, as is illustrated by numerous publications throughout history. In many places (where poverty abounds) they continue to be endemic (14), although isolated (in the case of leprosy) or not-so-isolated cases may still appear in developed countries, as has occurred with tuberculosis in the context of the Aids pandemic.
It should also be borne in mind that the characteristics of leprous lesions are not always as evident as those described here. Depending on the stage at which they are diagnosed, the appearance of these lesions may be similar to those of other conditions and this makes the differential diagnosis difficult (2,6,14). Hopefully the present report will serve to remind us that this stigmatized pathology should not be forgotten.
References
1. Aufderheide AC, Rodríguez-Martín C. eds. The Cambridge Encyclopedia of Human Paleopathology. Cambridge: Cambridge University Press; 1998. p. 141-54. [ Links ]
2. Laskaris G. Lepra. En: Atlas de enfermedades orales. Barcelona: Masson; 2005. p. 196-8. [ Links ]
3. Scheepers A. Correlation of oral surface temperatures and the lesions of leprosy. Int J Lepr Other Mycobact Dis 1998;66:214-7. [ Links ]
4. Fucci da Costa AP, Da Costa Nery JA, Wan-del-Rey de Oliveira ML, Cuzzi T, Ramos-e-Silva M. Oral lesions in leprosy. Indian J Dermatol Venereol Leprol 2003;69:381-5. [ Links ]
5. Núñez-Martí JM, Bagán JV, Scully C, Peñarrocha M. Leprosy: dental and periodontal status of the anterior maxilla in 76 patients. Oral Diseases 2004;10:19-21. [ Links ]
6. Aguado García JM. Tuberculosis y otras infecciones por micobacterias. Lepra. En: Rodés Teixidor J, Guardia Massó J, eds. Medicina Interna, Tomo I. Barcelona: Masson; 1997. p. 1800-2. [ Links ]
7. Andersen JG, Manchester K. The rhinomaxillary syndrome in leprosy: a clinical, radiological and paleopathological study. International Journal of Osteoarchaelogy 1992; 2:211-9. [ Links ]
8. Pavithran K. Histoid nodules of leprosy on the lip. Int J Leprosy and Other Mycobact Dis 1997;65:374-5. [ Links ]
9. Jopling WH. Clinical aspects of leprosy. Tubercle 1982; 63:295-305. [ Links ]
10. Shepard CC. Leprosy today. N Engl J Med 1982; 307:1640-1. [ Links ]
11. Reichart PA, Samaranayake LP, Samaranayake YH, Grote M, Pow E, Cheung B. High oral prevalence of Candida krusei in leprosy patients in Northern Thailand. J Clin Microbiol 2002;40:4479-85. [ Links ]
12. WHO (World Health Organization). Leprosy situation in the world and multidrug therapy coverage. Weekly Epidemiological Record 1992, 22 May. Geneva: World Health Organization. [ Links ]
13. Manchester K. Tuberculosis and leprosy: Evidence for interaction of disease. En: Ortner D, Aufderheide AC, eds. Human Paleopathology. Current Syntheses and Future Options. Washington DC: Smithsonian Institution Press; 1991. p. 23-35. [ Links ]
14. Gómez Echevarría JR, Hernández Ramos JM. Diagnóstico y tratamiento de la lepra. Experiencia en Brasil. Piel 2001;16:238-47. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Eduardo Chimenos-Küstner
Vía Augusta 124, 1º 3ª
08006 – Barcelona
E-mail: 13598eck@comb.es
Received: 11-03-2006
Accepted: 3-06-2006