Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.6 nov./dic. 2006
Frontal sinus mucocele with intracranial and intraorbital extension
Mucocele del seno frontal con extensión intraorbitaria e intracraneal
Beatriz Peral Cagigal 1, Javier Barrientos Lezcano1, Raúl Floriano Blanco 1, José Miguel García Cantera 2,
Luis Antonio Sánchez Cuéllar 2, Alberto Verrier Hernández3
(1) Médico Residente
(2) Médico Adjunto
(3) Jefe de Servicio. Servicio Regional de Cirugía Oral y Maxilofacial. Hospital Universitario del Río Hortega. Valladolid
ABSTRACT
Introduction: Frontal sinus mucoceles can present with a multitude of different symptoms including ophthalmic disturbances. Even benign, they have a tendency to expand by eroding the surrounding bony walls that displaces and destroys structures by pressure and bony resorption.
Case report: A 32-year-old man with diplopia, proptosis of the right eye and headache was presented. The diagnosis was frontal sinus mucocele with intracranial and intraorbital extension. Possible clinical manifestations of mucoceles, diagnostic imaging techniques and treatment used are discussed.
Conclusion: Frontal mucoceles are benign and curable, early recognition and management of them is of paramount importance, because they can cause local, orbital or intracranial complications.
Key words: Frontal mucocele, proptosis, open sinus surgery.
RESUMEN
Introducción: Los mucoceles del seno frontal pueden presentarse con multitud de síntomas diferentes, incluyendo alteraciones oftálmicas. Son benignos, aunque tienen tendencia a la expansión mediante erosión de las paredes adyacentes, lo que produce desplazamiento y destrucción de estructuras por presión y resorción ósea.
Caso clínico: Se presenta el caso de un hombre de 32 años con diplopia, proptosis del ojo derecho y cefalea fronto-temporal, cuyo diagnóstico fue de mucocele del seno frontal con extensión intracraneal e intraorbitaria. Discutiremos las posibles manifestaciones clínicas de los mucoceles, las técnicas de imagen empleadas, así como el tratamiento realizado.
Conclusión: Los mucoceles del seno frontal son benignos y curables, aunque un rápido diagnóstico y tratamiento son de vital importancia ya que pueden causar complicaciones locales, orbitarias o intracraneales.
Palabras clave: Mucocele frontal, proptosis, cirugía abierta sinusal.
Introduction
Mucocele is a chronic, expanding, mucosa-lined lesion of the paranasal sinus characterized by mucous retention that can be infected becoming a mucopyocele. They originate from obstruction of the sinus ostium by congenital anomalies, infection, inflammation, allergy, trauma (including surgery) or a benign or malignant tumour (1). Even benign, they have a tendency to expand by eroding the surrounding bony walls that displaces and destroys structures by pressure and bony resorption. The frontal sinuses are most commonly affected, and subsequently ethmoidal sinuses (2).
Symptoms and signs of frontal mucoceles include pain, swelling, exophtalmos, diplopia and loss of vision. An erosive mucocele may lead to meningitis, meningoencephalitis, pneumocephalus, brain abscess, seizures or CSF fistulas.
They are benign lesions that occur with similar frequency in adults of both sexes and rarely in children less of ten years.
A mucocele appears on imaging as an expansive lesion in an airless sinus, with thinning and sometimes erosion of its bony walls.
Computerised tomographic scan (CT) has proven to be an excellent diagnostic tool and is essential in surgical planning. Magnetic resonance imaging (MRI) may provide additional information in the examination of the orbit and may be preferred imaging technique if other soft tissue tumours causing proptosis cannot be excluded.
Differential diagnosis includes paranasal sinus carcinoma, Aspergillus infection, chronic infection or inverting papilloma.
The most common treatment modality is extirpation of the mucocele, cranialization or exclusion of sinus and nasofrontal duct obliteration (3).
Case report
A 32-year-old man with a history of diplopia and proptosis of the right eye for ten days, was referred to the Department of Oral and Maxillofacial Surgery from Emergency Department (Fig. 1). The patient had fronto-temporal right headache too. The ocular motility of the right eye was restricted in up gaze with diplopia in that position. The pupils were equal and reactive, visual acuity and colour vision were normal. Ophtalmologic exploration shows no macular affectation. The patients past medical history included a traffic accident 15 years previously with cranial trauma.
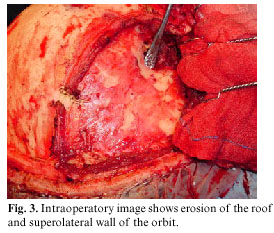
CT scan showed an expansive cystic mass in the right frontal sinus, isodense, non-enhancing, with orbital and anterior cranial fossa extension, causing gross downward and outward displacement of the globe. The mucocele had determined erosion of the roof and superolateral wall of the orbit (Fig. 2).
Posteriorly, MRI of the orbit was suggested to better define the lesion. MRI showed that the mass was a mucocele arising from the frontal sinus causing proptosis.
The patient was operated by a surgical team comprising neurosurgeons and maxillofacial specialists. To reach the mucocele, an external surgical approach was used, through a coronal incision. This approach was used in order to gain better access to the area of the lesion and in order to make reconstruction easier (4). The treatment was fronto-temporal craniotomy, removal of the posterior wall of the frontal sinus and extirpation of mucocele by microsurgical dissection from extradural frontal lobe, and curettage (Fig. 3).
Posteriorly, the reconstruction was made with pericranial flap, but no sinusal exclusion technique was achieved, because the pericranial flap only occluded the frontal sinus foramen and the epithelial sinusal coverture was eliminated by water-refrigerated bur. It procures a "de facto" sinusal exclusion. Next, dural repair, through suture with silk and covered with a physiological hemostatic adhesive (Tissucol®), and remodelling cranioplasty were performed. A postoperative CT scan confirmed the appropiate expansion of the frontal lobe.
The patient was operated and the presumptive preoperative diagnosis of mucocele was confirmed in the histological examination.
Postoperatively at 1 year, there was complete resolution of the proptosis and the patient was asymptomatic (Fig. 4).
Discussion
Mucoceles are mucous-secreting expansive pseudocystic formations, and capable of expansion by virtue of a dynamic process of bone resorption and new bone formation (5). They result from obstruction of a sinus ostium and frequently are related to a previous condition as chronic sinusitis, trauma, surgery or expansible lesion. With continued secretion and accumulation mucus, the increasing pressure causes atrophy or erosion of the bone of the sinus, allowing the mucocele to expand in the path of less resistance. This may be into the orbit, adjacent sinuses, nasal cavity, intracranial or through the skin (6); intracranial and orbital extension were demonstrated in this patient.
Mucoceles are most commonly found in the frontal and ethmoidal sinuses, are infrequent in the sphenoid sinus and occur rarely in the maxillary sinuses.
Proptosis is the most common presenting sign of a frontal mucocele, as in our case. Other clinical features include a mass in the upper medial quadrant of the orbit, pain, vertical diplopia, limited upward gaze, bifrontal headache and increasing tearing (7). Occasionally, an aggressive mucocele will cause bone destruction, especially of the orbital wall and may then simulate a malignant neoplasm. In these cases, CT is particularly helpful to distinguish benign from malignant disease, because an expanding mucocele often preserves a thin fat plane between margins of the mucocele and the muscle cone.
Other known complications of frontal mucoceles include erosion of the anterior wall, resulting in a tender fluctuant mass beneath the periosteum of the frontal bone. Erosion of the posterior wall may produce complications such as epidural abscess, meningitis, subdural empyema and brain abscess. Rarely, cranial nerve palsies may also occur.
When the mucocele produces unilateral proptosis various pathologies must be included in the differential diagnosis,
such as dysthyroid eye disease, retrobulbar orbital tumour, inflammatory pseudo tumour, sinus tumour and metastatic lesion. Progressive unilateral painless proptosis of gradual onset should make one suspicious of a mucocele involving the paranasal sinuses. This is especially so if there is accompanying diplopia, orbital or forehead pain and epiphora, which are frequently the presenting symptoms of mucoceles.
The classic radiographic appearance of a mucocele is generalised thinning and expansion of the sinus walls and there may also be evidence of sinus disease as well as bony erosions. The mucocele usually appears homogenous and airless.
CT scan is much better in delineating the extent of the lesion and its relations to other surrounding structures (8). CT demonstrates an airless, mucoid density filled, expansile, non-enhancing sinus mass with gradual thinning and erosion of the bony margins. The extent of the bone destruction is also better appreciated on CT. Frontal sinus mucoceles tend to erode posterior wall because of its inherent thinness.
MRI exhibits variable signal intensities on both T1- and T2-weighted images, depending on the state of hydration, protein content and viscosity of the contents of the mucocele. Contrast-enhanced MR imaging is useful in differentiating mucoceles from sinonasal tumours. Mucoceles characteristically reveal a thin peripheral linear enhancement with central low-signal intensity on T1 weighted images; and sinonasal tumours demonstrate diffuse enhancement.
The definitive treatment of mucoceles is primarily surgical, but the mucoceles of the frontal sinus that extend into the orbits and the anterior cranial fossa can, in certain cases, be difficult to manage therapeutically and may lead to lethal complications (9). Traditionally, frontal mucoceles were treated with external open obliterative procedure (10). Alternatively, functional endoscopic sinus surgery can be used to evacuate the mucocele, but this procedure become difficult if there is intracranial expansion (11), as in our case. An external approach, combined with endoscopic surgery, is suitable in frontal mucoceles, especially in distal sites and in case of recurrence.
Pericranial flaps are reliable, thin, and supple and have a good arc of rotation and minimal donor site morbidity (12). The pericranium frontal flap obliterates the dead space and isolates the extradural space from contaminated facial cavities, diminishing the risk of infection of the anterior fossa (13).
The external open approach has the advantages of: being a direct approach, with allows exposure of the entire sinus, provides complete obliteration of the sinus to prevent recurrence of the sinus disease, and prevents blind curettage of any exposed duramater (14).
The prognosis for frontal sinus mucoceles is good with likelihood of cure, and a low incidence of recurrence. Although, for control of recurrences long-term follow-up is recommended (3).
Conclusion
Mucoceles arising in the frontal sinus frequently are clinically silent for a lot of time and often involve both the orbit and the anterior cranial fossa extensively. Frontal mucoceles are bening and curable, but early diagnosis and treatment of them is important.
Open surgery remains a valid procedure in frontal mucoceles with orbital and/or intracranial extension and in cases where the district anatomy is unfavourable for a purely endonasal approach.
Acknowledgements: We thank to Dr. Campos and Dr. Dusuky, from the Department of Neurosurgery, for their collaboration in this case.
References
1. Yap SK, Aung T, Yap EY. Frontal sinus mucoceles causing proptosis. Two case reports. Ann Acad Med Singapore 1998;27:744-7. [ Links ]
2. Veltrini V, Ferreira Junior O, Oliveira DT. Quistes mucosos del seno maxilar: una revisión de la literatura. Med Oral 2001;6:180-8. [ Links ]
3. Weitzel EK, Hollier LH, Calzada G, Manolidis S. Single stage management of complex fronto-orbital mucoceles. J Craniofac Surg 2002;13:739-45. [ Links ]
4. Molteni G, Spinelli R, Panigatti S, Colombo L, Ronchi P. Voluminous frontoethmoidal mucocele with epidural involvement. Surgical treatment by coronal approach. Acta Otorhinolaryngol Ital 2003;23:185-90. [ Links ]
5. Gavioli C, Grasso DL, Carinci F, Amoroso C, Pastore A. Mucoceles of the frontal sinus: Clinical and therapeutical considerations. Minerva Stomatol 2002;51:385-90. [ Links ]
6. Suri A, Mahapatra AK, Gaikwad S, Sarkar C. Giant mucoceles of the frontal sinus: a series and review. J Clin Neurosci 2004;11:214-8. [ Links ]
7. Avery G, Tang RA, Close LG. Ophthalmic manifestations of mucoceles. Ann Ophthalmol 1983;15:734-7. [ Links ]
8. Bilaniuk LT, Zimmerman RA. Computer-assisted tomography: sinus lesions with orbital involvement. Head Neck Surg 1980;2:293-301. [ Links ]
9. Constantinidis J, Steinhart H, Schwerdtfeger K, Zenk J, Iro H. Therapy of invasive mucoceles of the frontal sinus. Rhinology 2001;39:33-8. [ Links ]
10. Har-el G. Telescopic extracranial approach to frontal mucoceles with intracranial extension. J Otolaryngol 1995;24:98-101. [ Links ]
11. Pia F, Aluffi P, Borello G. Frontal mucocele: open surgery. Acta Otorhinolaryngol Ital 1999;19:155-9. [ Links ]
12. Horowitz JH, Persing JA, Nichter LS, Morgan RF, Edgerton MT. Galeal-pericranial flaps in head and neck reconstruction. Anatomy and application. Am J Surg 1984;148:489-97. [ Links ]
13. Rinehart GC, Jackson IT, Potparic Z, Tan RG, Chambers PA. Management of locally aggressive sinus disease using craniofacial exposure and the galeal frontalis fascia-muscle flap. Plast Reconstr Surg 1993;92:1219-26. [ Links ]
14. Haug GA, Dortzbach RK, Brandenburg J. Treatment of frontal sinus mucoceles with the osteoplastic flap technique. Ophthalmic Surg 1978;9:40-66. [ Links ]
![]() Correspondence:
Correspondence:
Dra. B. Peral Cagigal
Servicio Regional de Cirugía Oral y Maxilofacial,
Hospital Universitario del Río Hortega,
C/ Cardenal Torquemada s/n, 47010 Valladolid, España
E-mail: beaperal77@yahoo.es
Received: 31-03-2005
Accepted: 1-08-2006