Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.2 mar. 2007
Tensor tympani muscle: strange chewing muscle
Luis Miguel Ramírez1, Luis Ernestos Ballesteros2,German Pablo Sandoval3
(1) Doctor of Odontology with a degree in Prosthetic Dentistry and Temporomandibular Disorders in Universidad Javeriana– Santa fe de Bogota - Colombia. Medical Education in Orofacial-Otic referred symptoms. Associate Professor of Morphology in the Department of Basic Sciences of the Medicine Faculty - Universidad Industrial de Santander (UIS) - Bucaramanga - Colombia.
(2) Medical Doctor with Degree in Anatomy. Universidad Industrial de Santander (UIS). Basic Sciences Department Director, Professor of Morphology in the Department of Basic Sciences of the Medicine Faculty - Universidad Industrial de Santander (UIS) - Bucaramanga - Colombia
(3) Medical Doctor with degree in Otolaryngology from Hospital Militar- Santa fe de Bogota - Colombia. Surgery Professor of the Medicine Faculty - Universidad Industrial de Santander (UIS) - Bucaramanga - Colombia. Otolaryngology and head-neck surgerys Chief of Carlos Ardila Lule Clinic
ABSTRACT
This work seeks to alert medical and odontological staff to understanding and using interdisciplinary handling for detecting different pathologies common otic symptoms. It offers better tools for this shared symptomatology during therapys conservative phase. Tensor tympani muscle physiology and function in the middle ear have been veiled, even when their dysfunction and anatomical relationships may explain a group of confused otic symptoms during conventional clinical evaluation. Middle ear muscles share a common embryological and functional origin with chewing and facial muscles. This article emphasizes that these muscles share a functional neurological and anatomical dimension with the stomatognathic system; these muscles increased tonicity ceases to be a phenomenon having no logical connections. It offers functionality and importance in understanding referred otic symptoms in common with other extra-otical symptom pathologies. Tinnitus, vertigo, otic fullness sensation, hyperacusia, hypoacusia and otalgia are not only primary hearing organ symptoms. They should be redefined and related to the neighboring pathologies which can produce them. There is a need to understand temporomandibular disorders and craniofacial referred symptomatology from neurophysiologic and muscle-skeletal angles contained in the stomatognathic system. Common symptomatology is frequently observed in otic symptoms and temporomandibular disorders during daily practice; this should be understood by each discipline from a broad, anatomical and clinical perspective.
Key words: Oscicular chain, temporomandibular disorders, otic symptoms, malleus, tensor veli palatini, tensor tympani.
RESUMEN
Con este trabajo se pretende alertar al medico y al odontólogo en el entendimiento y la integración del manejo interdisciplinario para la detección de síntomas de oído comunes en patologías diferentes, brindando mayores herramientas en la fase conservadora de la terapia para esta sintomatología compartida. La fisiología del músculo tensor del tímpano y su funcionalidad en el oído medio ha sido velada aun cuando su disfunción y relaciones anatómicas están explicando un grupo de síntomas óticos confusos a la evaluación clínica convencional. Los músculos del oído medio comparten un origen embriológico y funcional común con los músculos masticatorios y faciales. En este artículo se pretende hacer énfasis en la dimensión neurológica y anatómica de la funcionalidad (individual y compartida) de estos músculos entre si y el sistema estomatognático. La tonicidad aumentada de este músculo deja de ser un fenómeno sin conexiones lógicas, ofreciendo a su actividad normal o disfuncional el protagonismo que se merece y redefiniendo su funcionalidad e importancia en la comprensión de los síntomas óticos referidos muy en común con síntomas de otras patologías de origen extra-ótico. El tinitus, vértigo, sensación de oído tapado, hipoacusia, hiperacusia y la otalgia son síntomas que al no ser primarios de patologías en oído, deben ser descartados por el medico y relacionados con patologías vecinas que pueden producirlos. Ya existe la necesidad de entender los desordenes temporomandibulares y la sintomatología referida cráneo-facial desde una perspectiva neurofisiológica y músculo-esquelética comprendida en el sistema estomatognático. En la práctica diaria se observa con frecuencia una sintomatología común para los síntomas oticos y los desordenes temporomandibulares que se deben entender bajo una perspectiva amplia, anatómica, neuroanatómica y clínica.
Palabras clave: Cadena oscicular, desordenes temporomandibulares, síntomas oticos, tensor del tímpano, maleolo, tensor del velo palatino.
Introduction
Most people suffering from temporomandibular disorders (TMD) suffer from local or referred chronic muscular pain. This is found in the orofacial muscles, accompanied by painful and non-painful symptomatology, affecting the cervical musculature and middle ear muscles with varied otic symptoms ranging from vertigo, tinnitus, otic fullness sensation, hyperacusia-hypoacusia to otalgia. Multiple anatomical or neurological possibilities start from muscular or articular dysfunction which can generate otic conditions which do not seem to correspond to clinical discoveries arising from initial evaluation.(1) Such possible inroads have more in common than the purely descriptive focus of anatomical structures. This can be seen in the temporomandibular joint (TMJ), the ear and closeness between muscular structures and the middle ear.(2) This review seeks to develop the connection between the ear and stomatognathic system from a mainly anatomical focus. This work is aimed at understanding otic symptomatology having no otic origin, rationalizing the muscle-skeletal bond from an anatomical perspective and integrating health disciplines.
Review
The tensor tympani muscles normal activity is related to a reflex neurological mechanism known as centrifuge auditory inhibition control (CAIC). This works in sound trauma protection and hearing discrimination of low tones, besides complex co-activation during velopharyngeal movements. The tensor tympani muscles normal physiology becomes changed during abnormal activity (seemingly during TMD) and is associated with otic symptoms expressed as otalgia, otic fullness sensation, tinnitus, vertigo and hyperacusia-hypoacusia, no justified otic pathology being presented such as Menieres syndrome, otitis, pontocerebellar angle neurinoma and/or otosclerosis. TMD is a sub-classification of muscle-skeletal disorders, including a series of craniofacial conditions having multifactor aetiology in adults and children.(3) Simultaneous tension of temporal and tensor tympani muscles has been electromyographically evaluated. This suggests a kindred relationship between orofacial, chewing and middle ear muscle operation due to TMD. Greater sympathetic tonus during emotional stress may be present because they share common pathophysiological scenarios.(4)
Increased emotional tension produces dysfunctional muscular activity and consequently TMD. Lam et al., (5) have stated that otalgia and other non-otological symptom prevalence in TMD patients varies from 3.5% to 42%. Tinnitus prevalence in TMD patients seems to be greater than in the general population.(6) Tinnitus frequency in patients with TMD varies from 33% to 76%.(7,8) There is 40% to 70% dizziness and 5% to 40% vertigo prevalence in patients suffering from TMD. (9,10)
TMD prevalence is twice to nine times greater in women than in men. These are complex pathologies having consequences ranging from difficulty in chewing and other oral functions to acute-chronic pain. TMD aetiology can be summarized as macro trauma and micro trauma (bruxism or pain). Bruxism plays an important role in TMD and referred orofacial symptoms, although many investigations have considered such association inconclusive.(11) The intimate nexus between dysfunctional masticatory activity, such as bruxism, TMD and emotional stress, can lead to the cause-effect relationship between them. TMD aetiology thus has a multifactor origin involving environmental, physiological and behavioural agents.
TMD produces contraction and tension of the masticatory muscles and reflex contraction in tensor veli palatini and tensor tympani muscles due to common motor innervation from the trigeminal mandibular branch (V3) (12-17) Schames et al., (18) have stated that the dysfunction of these muscles (accessory mastication muscles) plays an important role in otic symptoms. Otalgia can be felt by tympanic membrane tension due to constant tensor tympani muscle contracture. Such tension can produce dysacusia (a more general tinnitus symptom) accompanied by strange or hallucinatory acoustic sensations perceived as rings, clicks, pops, whispers or friction noises. Middle ear muscular tension can also be associated with hyperacusia and hypoacusia from a conductive origin and subjective presentation (even with normal audiometric values). The physical tension increased by emotional stress and headaches concomitantly accompanies such otic symptomatology.
The complex neuromuscular interaction between the muscles of mastication and the ear was referred to as otognatic syndrome by Myrhaug (13) in 1964 and otomandibular syndrome by Bernstein in 1969 (14) and by Arlen in 1977.(19) Patients suffering from otomandibular syndrome present one or more otic symptoms without ear, nose or throat pathology, but have one or more mastication muscles in a state of constant spasm.
Ogutcen-Toller and Juniper (20) noticed that the structures driving sound in the middle ear can be affected by reflex tensor tympani contraction in TMD patients. They evaluated hearing status in TMD-otic symptom patients without finding clear middle ear or Eustachian tube dysfunction. This suggested tensor tympani conductive modulation with subjective hearing loss. Travell and Simons (21) explained tinnitus as being a referred sensitive phenomenon, starting as reflex muscular spasm from middle ear stapedial and tensor tympani muscles.
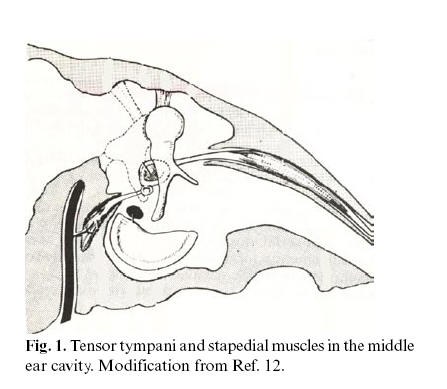
Myrhaug (13) agreed that there is reflex contraction of the tensor tympani in subjective tinnitus and rhythmic opening and closing of the Eustachian tube (palatine mioclonus) in objective tinnitus (externally perceived). Reflex muscular contraction is present in tensor tympani and tensor veli palatini muscles.(22) Objective tinnitus is much less common than subjective tinnitus. Zipfel et al., (23) supported the above and explained that the more common mechanical causes of objective tinnitus were palatine mioclonus and middle ear mioclonus producing tympanic membrane rhythmic movement secondary to repetitive stapedial and tensor tympani muscle contraction. (Figure 1) This muscular behaviour may correspond to a reflex pattern due to constant fatigue originating in these muscles abnormal somatomotor function during increased emotional tension and bruxism.
Shapiro and Truex (24) suggested these middle ear muscles possible tonic spasm and reflex due to the V and VII pairs being peripherally irritated (TMD); this could lead to impaired hearing of low tones. The balance of the oscicular chain and the functioning of structures driving sound in the middle ear normally depend on the stapedial and tensor tympani (antagonistic muscles). Sustained contraction of these muscles in TMD may alter inner ear perilymphatic and endolymphatic pressure through changes transmitted from the oval window toward the walls of the labyrinth and semicircular canals. This may lead to vestibular and cochlear impulse imbalance and similar symptomatic reaction to Menieres syndrome.
It is imperative that the middle ear oscicular chain (malleus, incus and stapes) be seen from an efficient but fragile biomechanical viewpoint. They are practically sustained by weak structures such as the tympanic membrane, some ligaments and stapedial and tensor tympani muscle tendons maintaining these bones in an articulation adapted to sound energy.
Auditory muscle (tensor tympani, tensor veli palatini and stapedial) functions are shown in Table 1. Stapedial muscle contraction happens with strong sounds and immediately before speaking. This improves auditory discrimination ability, external vocalization and reduces the masking effect of autogenous sound.(25,26) The tensor tympani muscle (in spite of common belief) is not an inoperative muscle due to it responding electromyographycally to strong sounds and vocalization, chewing, swallowing and facial muscle external stimulation.(27) If tensor tympani and veli palatini muscles share movements in common (velopharyngeal and facial) and tensor tympani and stapedial muscles together are neurologically activated (hearing protection reflexes and auditory discrimination) by the centrifuge reflex then it may be stated that facial and velopharyngeal movements shared by both tensile muscles have important influence on otic-TMD symptomatology.
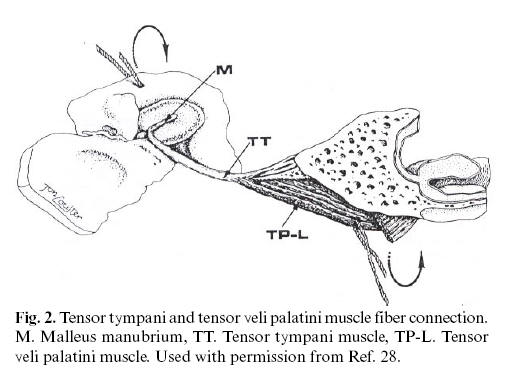
Rood and Doyle (28) found from dissecting adult and foetal cadavers that tensor veli palatini anatomy consisted of a medial portion or dilatator tubae (described by Gray in 1918), an external portion consisting of the tensor veli palatini muscle and an intratympanic consisting of the tensor tympani muscle intermingling its fibres with the tensor veli palatinis external area.(29) The tensor veli palatinis lateral area originates in the sphenoid spine, scaphoid fossa, lateral bony edge of the sphenoid fissure and tensor tympani muscle. The tensor veli palatinis medial area originates in the lateral membranous wall of the Eustachian tubes posterior and middle third. These muscles descend and converge on the pterygoid hamulus in a strong tendon curving around this hook-shaped osseous process to be inserted into the soft palate in a horizontal direction (palatine aponeurosis). Yawning, laughing, swallowing and coughing involve pharyngeal and laryngeal muscles activating the tensor tympani muscle.
Kamerer (26) expressed his astonishment in 1978 that no unified theory had been created for these muscles sharing such close anatomical relationship. Tensor tympani and tensor veli palatini muscles work simultaneously (electromyographically proved) during swallowing, thereby producing a Djupesland air bomb in the middle ear assisting with Eustachian tube ventilation. Tensor tympani and tensor veli palatini muscles together produce tympanic membrane internal deflection breaking the Eustachian tubes mucous membrane isthmus seal (expelled air), thereby contributing to middle ear ventilation (30). Barsoumian, Kuehn et al., (31) corroborated Lupin and Rood-Doyles findings. (Figure 2) The middle ears tendinous part, between tensor tympani and tensor veli palatini muscles, shows an anatomical connection between these muscle functions. These synergistic muscles may temporarily raise intratympanic pressure when they contract together.
It should not be said that the tensor veli palatini has an additional bony origin in the malleus manubrium. Tensor veli palatini dysfunction (TMD or bruxism) may modify malleus and tympanic membrane medial position due to anatomic anchorage with the tensor tympani. Kierner et al., (32) found such connection (histological study) in human cadavers. They stated that this represents an important step in understanding the functional unit between these two muscles in humans. Schames et al., (18) suggested that tensor tympani and tensor veli palatini secondary myofibrotic contracture (adhesions and trigger points) complicates their anatomical relationship and otic symptomatology due to their reduced muscular fibre length.
It should be stressed that understanding middle ear ventilation physiology through the Eustachian tube involves neurological territories referred from the masticatory system. In 1987, Malkin (33) stated that the tensor tympani serves as a barometric pressure receiver. Its propioceptive afference signals (starting from their muscular length) can be triggered in a hypotonic situation caused by low tympanic cavity pressure (due to mucosal air exchange). Such low-pressure medially retracts the tympanic membrane and tensor tympani tendon due to great external environmental pressure accompanied by no resistance to force; such new muscle elongation is perceived by its muscular spindles. The trigeminal motor nucleus produces a reflex mechanism in a polysynaptic central arrangement, beginning tensor muscle contraction involving opening the Eustachian tube, middle ear ventilation and pressure equilibration; such normal physiological mechanisms may be blocked by the tensortympani hypertonic scenario during TMD.
These would be expressed via tube dysfunction and accompanying otic symptomatology, such as hypoacusia, tinnitus, vertigo, otalgia, otic fullness and even otitis media.
For almost one hundred years several investigators have tried to outline possible cause-effect relationship between otic symptoms and TMD from mechanical, vascular, neurological, muscular and embryological viewpoints. As medicine and dentistry became more specialised the hearing organ and stomatognathic systems were abruptly separated; this situation has been discreetly corrected via specialization in otolaryngology and craniofacial pain which has attempted to close the breach in such thematic discussion which had been gaining the stigma of being a no mans land.
Conclusion
This article has concerned itself with the need for understanding the presence of a masticatory muscle in the middle ear which can complicate TMD otic symptomatology. This idea will be developed in articles to follow, as well as other stomatognathic neurological and mechanical causes. This muscles anatomy, neuroanatomy and physiology (besides being interesting in itself) is related to intratympanic hearing activity which may be externally modulated by the masticatory system in the presence of muscle skeletal disorder.
It is imperative that the need for a medical and odontological interdisciplinary patient management system be understood. Specialists in a single discipline are not always able to solve a patients heterogeneous symptoms without the invaluable support of a multidisciplinary approach. Each specialty contributes its specific knowledge to differential diagnosis aimed at a more assertive treatment plan. Clinical success therefore depends on each specialists ability to analyse different aspects of the same problem. Team work can thus be best used for obtaining the best functional state in a particular patients stomatognathic system.
References
1. Ramirez LM, Sandoval GP, Ballesteros LE. Theories on otic symptoms in temporomandibular disorders: Past and Present. Int J Morphol 2005;23:141-56. [ Links ]
2. Ramirez LM, Sandoval GP, Ballesteros LE. Temporomandibular disorders: referred cranio-cervico-facial clinic. Med Oral Patol Oral Cir Bucal. 2005;10:E18-26.
3. Youniss S. The relationship between craniomandibular disorders and otitis media in children. Cranio 1991;9:169-73
4. Klockhoff I, Lindholm L, Westerberg CE. Spontaneous impedance fluctuation--a "tensor tympani syndrome" with special reference to tension headache. Nord Med 1971;85:577.
5. Lam DK, Lawrence HP, Tenenbaum HC. Aural symptoms in temporomandibular disorder patients attending a orofacial pain unit. J Orofac Pain 2001;15:146-57.
6. Cooper BC, Cooper DL. Recognizing otolaryngologic symptoms in patients with temporomandibular disorders. Cranio 1993;11:260-7
7. Parker WS, Chole RA. Tinnitus, vertigo and temporomandibular disorders. Am J Orthod Dentofacial Orthop 1995;107:153-8
8. Rubinstein B. Tinnitus and craniomandibular disorders-- Is there a link?. Swed Dent J Suppl 1993;95:1-46
9. Chole RA, Parker WS. Tinnitus and vertigo in patients with temporomandibular disorders. Arch Otolaryngol Head Neck Surg 1992;118:817-21.
10. Bush FM. Tinnitus and Otalgia in temporomandibular disorders. J Prosthet Dent 1987;58:495-8
11. Pergamalian A, Rudy TE, Zaki HS, Greco CM. The association between wear facets, bruxism, and severity of facial pain in patients with temporomandibular disorders. J Prosthet Dent 2003;90:194-200.
12. Anatomía de Bouchet y Guilleret. Editorial Panamericana.
13. Myrhaug H. The incidence of the ear symptoms in cases of malocclusion and temporomandibular joint disturbances. Br J Oral Maxillofac Surg 1964;2:28-32
14. Bernstein JM, Mohl ND, Spiller H. Temporomandibular joint dysfunction masquerading as disease of ear, nose and throat. Trans Am Acad Ophthalmol Otolaryngol 1969;73:1208-17.
15. Manni A, Brunori P, Giuliani M, Modoni M, Bizzi G. Oto-vestibular symptoms in patients with temporomandibular joint dysfunction. Electromyographic study. Minerva Stomatol 1996;45:1-7
16. Ciancaglini R, Loreti P, Radaelli G. Ear, nose and throat symptoms in patients with TMD: The association of symptoms according to severity of arthropathy. J Orofac Pain 1994;8:293-7.
17. Eckerdal O. The petrotynpanic Fissure: A link connecting the tympanic cavity and the temporomandibular joint. Cranio 1991;9:15-21.
18. Schames J, Schames M, King E, Ulansey S, Boyd J, Schames E. Trigeminal Pharyngioplasty: Treatment of the forgotten accessory muscles of mastication which are associated with orofacial pain and ear symptomatology. AJPM 2002;12:102-12.
19. Arlen H. The otomandibular syndrome: A new concept. Ear Nose Throat J 1977;56:60-2.
20. Ogutcen-Toller M, Juniper RP. Audiological evaluation of the aural symptoms in temporomandibular joint dysfunction. J Craniomaxillofac Surg 1993;21:2-8.
21. Travell JG, Simons DG, eds. Dolor y disfunción miofascial. El manual de los puntos gatillo, Mitad superior del cuerpo. Madrid: Editorial Panamericana; 2002. p. 419,476.
22. Virtanen H. Objective tubal tinnitus: a report of two cases. J Laryngol Otol 1983;97:857-62.
23. Zipfel TE, Kaza SR, Greene JS. Middle-ear myoclonus. J Laryngol Otol 2000;114:207-9.
24. Shapiro HH, Truex RC. The temporomandibular joint and the auditory function. J Am Dent Assoc 1943;30:1147-68.
25. Klockhoff I, Anderson H. Reflex activity in the tensor tympani muscle recorded in man; preliminary report. Acta Otolaryngol 1960 ;51:184-8.
26. Kamerer DB. Electromyographic correlation of tensor tympani and tensor veli palatini muscles in man. Laryngoscope 1978;88:651-62.
27. Gray LP. The relationship between the "superior constrictor swallow" clicking of the ears and ear disease. J Laryngol Otol 1983;97:1121-8.
28. Rood SR, Doyle WJ. Morphology of the tensor veli palatiny, tensor tympani and dilatator tubae muscles. Ann Otol Rhinol Laryngol 1978;87:202-10.
29. Rood SR. The morphology of muscle tensor veli palatini in the five month human fetus. Am J Anat 1973;138:191-5.
30. Salen B, Zakrisson JE. Electromyogram of the tensor tympani muscle in man during swallowing. Acta Otolaryngol 1978;85:453-5.
31. Barsoumian R, Kuehn DP, Moon JB, Canady JW. An anatomic study of the tensor veli palatini and dilatator tubae muscles in relation to eustachian tube and velar function. Cleft Palate Craniofac J 1998;35:101-10.
32. Kierner AC, Mayer R, v Kirschhofer K. Do the tensor tympani and tensor veli palatini muscles of man form a functional unit? A histochemical investigation of their putative connections. Hear Res 2002;165:48-52.
33. Malkin DP. The role of TMD dysfunction in the etiology of middle ear diseases. Int J Orthod 1987;25:20-1.
![]() Correspondence:
Correspondence:
Dr. Luis Miguel Ramirez
E-mail: lmra3@yahoo.com
Received: 2-10-2005
Accepted: 17-12-2006