Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.8 dic. 2007
The post-endodontic periapical lesion: Histologic and etiopathogenic aspects
Celia Carrillo García1, Francisco Vera Sempere2, Miguel Peñarrocha Diago3, Eva Martí Bowen4
(1) Student of Master of Oral Surgery and Implantology. Valencia University Medical and Dental School
(2) Professor of Anatomic Pathology. Valencia University Medical and Dental School
(3) Professor of Oral Surgery. Director of the Master of Oral Surgery and Implantology. Valencia University Medical and Dental School
(4) Doctor in Dental Surgery. Private Practice
ABSTRACT
Apical periodontitis is produced in the majority of cases by intraradicular infection. Treatment consists in the elimination of the infectious agents by endodontia. Even when carrying out a correct cleansing and filling of canals, it is possible that periapical periodontitis will persist in the form of an asymptomatic radiolucency, giving rise to the post-endodontic periapical lesion.
The chronic inflammatory periapical lesion is the most common pathology found in relation to alveolar bone of the jaw. From the histological point of view, it can be classified as chronic periapical periodontitis (periapical granuloma), radicular cyst, and as scar tissue. The most frequent is the periapical granuloma, constituted by a mass of chronic inflammatory tissue, in which isolated nests of epithelium can be found. The radicular cyst is characterized by the presence of a cavity, partially or wholly lined by epithelium. Scar tissue is a reparative response by the body, producing fibrous connective tissue.
The aim of this study is to review and update the etiopathogenic and histological aspects of chronic post-endodontic periapical lesions.
Key words: Periapical lesion, chronic periapical periodontitis (periapical granuloma), radicular cyst, scar tissue.
Introduction
Periapical lesions resulting from necrotic dental pulp are among the most frequently occurring pathologies found in alveolar bone. Exposure of the dental pulp to bacteria and their by-products, acting as antigens, may elicit nonspecific inflammatory responses as well as specific immunological reactions in the periradicular tissues, and cause the periapical lesion (1,2).
Apical periodontitis is usually produced by an intraradicular infection. Treatment consists of the elimination of the infectious agents by root canal treatment, allowing healing of the lesion (3). However, when the infection is not completely eliminated, the periapical lesion remains, being considered a treatment failure (4). Even when the canal is correctly cleaned and filled, it is possible that the periapical periodontitis will persist, observing a radiotransparent image which may be asymptomatic. This is due to the complex root canal system, with accessory canals, ramifications and anastomoses, which cannot be accessed, cleaned or filled by conventional techniques (5). Furthermore, extraradicular factors such as periapical actinomycosis, foreign body reaction to extruded root canal filling, other foreign materials or endogenous cholesterol crystals can interfere with post-treatment healing of apical periodontitis (6). When faced with a periapical lesion that persists after root canal treatment, even when asymptomatic, the dental surgeon should consider either retreatment of the canal, periapical surgery or extraction of the affected tooth.
A histological study of the periapical lesion can be used to weigh the clinical symptoms and the radiographic signs against the nature of the possible periradicular tissue alterations; and to confirm the diagnosis of periapical periodontitis and distinguish it from a non-inflammatory lesion (7).
A Medline search was made for articles published between August 1973 and April 2006, using the following key words: periapical lesion, radicular cyst, chronic periapical periodontitis (periapical granuloma) and scar tissue. Articles which studied periapical lesions from the histological point of view, and likewise those that carried out differential diagnosis against non inflammatory periapical lesions were selected.
This article aims to review and update the etiopathogenic and histological aspects of post-endodontic chronic periapical lesions: chronic periapical periodontitis (periapical granuloma), radicular cysts and scar tissue.
General Concepts
Six possible biological factors have been described as causing asymptomatic apical periodontitis following root-canal treatment: persistent intraradicular infection, extraradicular infection (principally actinomycosis), foreign body reaction related to the root filling material, the accumulation of endogenous cholesterol crystals that irritate the periapical tissue, true cystic lesions, and scar tissue (8).
The principal cause of apical periodontitis is the persistence of microorganisms in the root canal system. The microorganisms found in these cases are predominantly Gram-positive (cocos, bacillus and filaments, such as Actinomyces, Enterococcus and Propionibacterium (9). Ricucci et al. (10), analyzed 50 untreated extracted teeth with periapical lesions, finding bacteria colonizing the necrotic tissue of the root canal, the dentinal tubules or the apical ramifications in all teeth, however, bacteria were found in the body of the periapical lesion in only 18 abscesses or cysts. Molander et al. (11) carried out microbiological and electron microscope studies which demonstrated the presence of fungi in the roots of teeth with periapical lesions, mainly Candida albicans. Extraradicular periapical actinomycosis is a chronic granulomatous infection, caused by species of types Actinomyces and Propionibacterium; with A. israelii being the most frequently isolated species. These microorganisms are able to build cohesive colonies and so escape the bodys defense mechanisms, thus establishing themselves in the periapical tissue (12).
Among the non-microbiological causes are found foreign body reactions to intraradicular filling material extruded from the canal at the periapex, producing an asymptomatic radiotransparent lesion. The most-frequently used material for root-end filling is gutta percha; the extruded points are associated with periapical lesions as they induce an intense localized response in the tissue, characterized by macrophages and giant multinucleate cells. Other materials that can induce this type of reaction are paper points, silver amalgam, endodontic sealants and calcic salts derived from the extruded Ca(OH)2 (6).
The incidence of cholesterol crystals in periapical lesions varies between 18% and 44% of all lesions (13); they are surrounded by macrophages and giant multinucleate cells that are unable to degrade the crystals and act as mediators, increasing inflammation and bone resorption (6). True cysts and scar tissue are the two other pathologies that may be associated with a periapical radiotransparency (8).
Periapical periodontitis is the inflammation and destruction of the periapical tissue caused by agents responsible for pulpar infection. When the infection reaches the periapex a predominantly anaerobic mixed flora is established; in response, the host releases defense mechanisms, in the form of various cell types, intercellular messengers and antibodies. The microbiological factors and the host defense mechanism interact, destroying are large amount of periapical tissue, giving rise to the different types of periapical lesion (1, 14). The primary response at vascular level is rapid vasoconstriction, followed almost immediately by vasodilation, giving rise to an accumulation of red blood cells in the center of the vessel, and a migration of leukocytes to the peripheral areas, adhering to the vascular walls. This provokes the formation of small fissures in the endothelium of the vessel, inducing an extravasation of plasma towards the connective tissue; edema is produced which increases local pressure and compressing the nerve endings, causing pain. The final consequence of the inflammatory process is an infiltrate containing lymphocytes, macrophages and plasmatic cells. In the acute phase of the inflammation, an exudate is produced as a response to the aggression of the pulp and periapical tissue, with predomination of polymorphonuclear neutrophils. Once the inflammation has reached the chronic stage, the host responds with a proliferation of new cells, vessels and fibers, in an attempt to repair the lesion, resulting in the formation of new tissue, known as granulation tissue (15).
The host attempt to repair and regenerate the damaged tissue is compromised by the presence of bacterial contamination; this becomes a chronic process unless adequate clinical treatment to eliminate the infectious agents is instigated (2).
Chronic periapical periodontitis (granuloma)
The structural components of a periapical lesion depend on the balance between the microbiological factors and the host defenses (14). Thus, when the pulpar infection spreads to the periapex, a symptomatic inflammatory response of the periapical connective tissue is produced in the form of an abscess or acute lesion. The lesion contains a dense accumulation of polymorphonuclear (PMN) leukocytes, lined by granulomatous tissue containing lymphocytes, macrophages and plasmatic cells (16). Not all authors include the periapical abscess in the diagnosis of periapical lesions; Vier and Figueiredo (17) found 70% of abscesses in 102 lesions analyzed, and Ricucci et al., (2) 28% of 57 lesions (Table 1). After the acute phase, the periapical lesion may remain, giving rise to one of the three chronic forms: chronic periapical periodontitis (periapical granuloma), radicular cyst or scar tissue (Figure 1).
Chronic periapical periodontitis (periapical granuloma) is a localized mass of chronic inflammatory tissue, with acute inflammatory infiltrate containing macrophages and polymorphonuclear cells; and chronic inflammatory infiltrate containing B and T lymphocytes (16). The prevalence of apical granuloma, observed in the different series, varies between 9.3% and 87.1% (Table 1).
In chronic periapical periodontitis it is common to find nests of epithelium, formed from epithelial cell rests of Malassez, having a latent capacity to proliferate (Figure 2A). Leonardi et al. (18), examined 17 periapical granulomas, finding epithelial cell rests of Malassez associated with inflammatory cells or epithelial strands in 10. The epithelial cells are normally arranged in layers forming small islands, strands and / or trabecula of varying thickness.
Radicular cyst
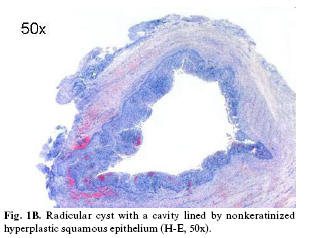
The radicular cyst is a chronic inflammatory lesion with a closed pathologic cavity (16,17,19,20), lined either partially or completely by non-keratinized stratified squamous epithelium. The underlying fibrous connective tissue wall is inflamed with varying degrees of cell infiltration, which consists mainly of macrophages and small blood vessels (21). In radicular cysts, cholesterol crystals move in the direction of the epithelium-lined cyst cavity (Figure 2B), since the outer collagenous capsule of the lesion is too tough for the crystals to move through (6). Occasionally however, periapical cysts are found to be lined, partially or predominantly, by columnar ciliated epithelium or mucosecretory cells, which may be due to the migration of these cells from either the maxillary sinus or the nasal cavity, the metaplasia of the stratified squamous epithelium, or to the differentiation of pluripotent cells within the jaw (22). Nair and Pajarola (23) found three cysts lined with ciliated columnar epithelium out of 256 analyzed periapical lesions.
The radicular cyst is the most frequent cyst found in the jaw (between 52% and 68% of all the jaw cysts) (24). The prevalence of periapical cysts varies between 8.7% and 37.7% of chronic inflammatory periapical lesions (Table 1), this discrepancy is possibly due to the different criteria used in the histological studies; although the boundary between one diagnosis and another is not clearly defined in the literature. Thus, Nobuhara and Del Rio (19), established the diagnosis of cyst with the presence of a cavity partially or completely lined by epithelium; if the lesion was made up of granulation tissue with epithelial proliferation, but without cavitation, it was diagnosed as granuloma. The histological diagnoses of samples with few slices can lead to the incorrect classification of epithelized lesions, diagnosing them as cysts. Nair et al. (16), carried out a study with meticulous serial sections, in which 52% of the lesions contained epithelium, but only 15% were in fact periapical cysts.
The etiopathogeny of cysts is particularly controversial (25), there formation has been explained by diverse theories, such as epithelial colonization, epithelial cavitation, or the formation of microabscesses. The first is based on the formation of an epithelized fistulous tract up to the granuloma from a periapical abscess fistulized to the oral cavity; when the communication is closed, the epithelial cells have already fully colonized the abscess, epithelizing it and giving rise to a radicular cyst. In the theory of epithelial cavitation, accumulations of epithelial cells are created; those furthest from the connective tissue which feeds them are left without vascularization and undergo degeneration and necrosis, thus forming the central area of the cyst. The theory of microabscess formation is based on the degeneration of the connective tissue leading to the development of the cyst; the formation of a microabscess in the nucleus of the granuloma, with the presence of stimulated epithelial cells, would lead to their growth in an attempt to line the created cavity. This process could originate in one or various foci of the granuloma that would converge to form a true cystic cavity (25). Nair (6), does not describe the theory of epithelial cavitation, considering the other two to be the principal theories for the formation of a cystic cavity. Ricucci and Bergenholtz (7) consider that little is known about the exact etiopathogenic mechanisms of cysts.
The pathogenesis of cysts has been described in three phases (22). During the first phase, the epithelial cell rests of Malassez begin to proliferate as a direct result of the inflammation, and influenced by bacterial antigens, the epidermal growth factors, metabolic and cellular mediators. In the second, a cavity is formed, lined by epithelium (according to the above described theories), and in the third phase the cyst grows, probably by osmosis.
Different classifications of cyst exist, Nair et al. (16) differentiate the true cyst when the cystic cavity is surrounded completely by epithelium and is not directly connected with the radicular canal, and the pocket cyst when the cystic cavity is directly connected with the radicular canal. Cury et al. (26) focus on the morphological aspects of the epithelium to classify cysts; the quiescent cysts have a uniform / homogeneous atrophic layer of stratified squamous epithelium, 10 cells thick, usually with a slight or moderate inflammatory infiltrate in the connective tissue; and the active lesions have a hyperplastic stratified squamous epithelium, of irregular but increasing thickness, usually with a tendency to proliferate, and with an inflammatory infiltrate in the fibrous capsule.
Scar tissue
The other form of chronic periapical lesion is scar tissue; this is a reparative response by the body with fibrous connective tissue, characterized by the formation of dense collagen in place of mature bone. The prevalence of these lesions varies from 6.6% to 12%, although not all authors consider it in their diagnosis (Table 1). Unresolved periapical radiolucencies may be due to the lesion healing with fibrous tissue, and not necessarily a sign of endodontic failure (8). Periapical scar tissue originates from connective tissue-forming cells that colonize the periapical area before the cells responsible for generating the different periodontal components do so (27).
Non-inflammatory periapical lesions
Cases of benign and malignant non-inflammatory periapical lesions have been described, that, in the absence of a histological study may be clinically suggestive of chronic inflammatory lesions (Table 1). Described cases included keratocysts (28), cysts of the nasopalatine canal (29), periapical cemental dysplasia (30), benign tumors (31) and locally aggressive or malignant neoplasias (32).
Kuc et al. (33) classified the histopathological diagnoses of 805 periapical biopsies using the following criteria: sequela of pulpar necrosis (chronic periodontitis, cysts, abscesses), complicated sequela of pulpar necrosis (with infection or involving the maxillary sinus), and periapical lesions unrelated with pulpar necrosis (odontogenic and non-odontogenic non-inflammatory lesions). The authors observed that histologically 97.9% were inflammatory lesions, 1.1% were complicated inflammatory lesions (with infection or involving the maxillary sinus), and 1% were non-inflammatory, highlighting that in 5% of the histopathological studies made, information was added to the initial clinical evaluation. Stajcic and Paljm (28) recommend histological analysis of all radicular cysts, in order to discount the possibility of finding a keratocyst and not diagnosing it; since in their study 0.7% of 565 cysts were re-diagnosed as keratocysts. Walton (34) established that from the surgical perspective, periapical lesions do not require a histological analysis, given the higher prevalence of inflammatory (cysts and granulomas) over noninflammatory lesions, finding no relation with the prognosis between the two types of lesion.
References
1. Liapatas S, Nakou M, Rontogianni D. Inflammatory infiltrate of chronic periradicular lesions: an immunohistochemical study. Int Endod J. 2003 Jul;36(7):464-71. [ Links ]
2. Ricucci D, Mannocci F, Ford TR. A study of periapical lesions correlating the presence of a radiopaque lamina with histological findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):389-94. [ Links ]
3. Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990 Oct;16(10):498-504. [ Links ]
4. Sundqvist G, Figdor D. Endodontic treatment of apical periodontitis. In: Orstavik D, Pitt Ford TR eds. Essential Endodontology. Oxford: Blackwell; 1988. p. 242-77. [ Links ]
5. Perrini N, Castagnola L eds. W Hess & O. Kellers Anatomical Plates: Studies on the Anatomical Structure of Root Canals in Human Dentition by a Method of Making the Tooth Substance Transparent (1928). Milano: Lainate; 1998. [ Links ]
6. Nair PNR. Non-microbial etiology: foreign body reaction maintaining post-treatment apical periodontitis. Endod Topics 2003;6:114-34. [ Links ]
7. Ricucci D, Bergenholtz G. Histologic features of apical periodontitis in human biopsies. Endod Topics 2004;8:68-87. [ Links ]
8. Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006 Apr;39(4):249-81. [ Links ]
9. Pinheiro ET, Gomes BP, Ferraz CC, Sousa EL, Teixeira FB, Souza-Filho FJ. Microorganisms from canals of root-filled teeth with periapical lesions. Int Endod J. 2003 Jan;36(1):1-11. [ Links ]
10. Ricucci D, Pascon EA, Ford TR, Langeland K. Epithelium and bacteria in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Feb;101(2):239-49. [ Links ]
11. Molander A, Reit C, Dahlén G, Kvist T. Microbiological status of root-filled teeth with apical periodontitis. Int Endod J. 1998 Jan;31(1):1-7. [ Links ]
12. Figdor D, Sjögren U, Sörlin S, Sundqvist G, Nair PN. Pathogenicity of Actinomyces israelii and Arachnia propionica: experimental infection in guinea pigs and phagocytosis and intracellular killing by human polymorphonuclear leukocytes in vitro. Oral Microbiol Immunol. 1992 Jun;7(3):129-36. [ Links ]
13. Trott JR, Chebib F, Galindo Y. Factors related to cholesterol formation in cysts and granulomas. J Can Dent Assoc (Tor). 1973 Aug;39(8):550-5. [ Links ]
14. Hama S, Takeichi O, Hayashi M, Komiyama K, Ito K. Co-production of vascular endothelial cadherin and inducible nitric oxide synthase by endothelial cells in periapical granuloma. Int Endod J. 2006 Mar;39(3):179-84. [ Links ]
15. López-Marcos JF. Aetiology, classification and pathogenesis of pulp and periapical disease. Med Oral Patol Oral Cir Bucal. 2004;9suppl:52-62. [ Links ]
16. Ramachandran Nair PN, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996 Jan;81(1):93-102. [ Links ]
17. Vier FV, Figueiredo JA. Internal apical resorption and its correlation with the type of apical lesion. Int Endod J. 2004 Nov;37(11):730-7. [ Links ]
18. Leonardi R, Caltabiano R, Loreto C. Collagenase-3 (MMP-13) is expressed in periapical lesions: an immunohistochemical study. Int Endod J. 2005 May;38(5):297-301. [ Links ]
19. Nobuhara WK, Del Rio CE. Incidence of periradicular pathoses in endodontic treatment failures. J Endod. 1993 Jun;19(6):315-8. [ Links ]
20. Vier FV, Figueiredo JA. Prevalence of different periapical lesions associated with human teeth and their correlation with the presence and extension of apical external root resorption. Int Endod J. 2002 Aug;35(8):710-9. [ Links ]
21. Tsai CH, Huang FM, Yang LC, Chou MY, Chang YC. Immunohistochemical localization of cyclooxygenase-2 in radicular cysts. Int Endod J. 2002 Oct;35(10):854-8. [ Links ]
22. Shear M. Cysts of the oral regions. 3rd edn. Oxford: Wright; 1992. [ Links ]
23. Nair PN, Pajarola G, Luder HU. Ciliated epithelium-lined radicular cysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Oct;94(4):485-93. [ Links ]
24. Nair PNR. Non-microbial etiology: periapical cysts sustain post-treatment apical periodontitis. Endod Topics 2003;6:96-113. [ Links ]
25. Gay C. Lesiones periapicales. In: Gay C, Berini L eds. Cirugía bucal. Madrid: Ediciones Ergon; 1999.p.749-80. [ Links ]
26. Cury VC, Sette PS, Da Silva JV, De Araújo VC, Gomez RS. Immunohistochemical study of apical periodontal cysts. J Endod. 1998 Jan;24(1):36-7. [ Links ]
27. Nair PN. Cholesterol as an aetiological agent in endodontic failures--a review. Aust Endod J. 1999 Apr;25(1):19-26. [ Links ]
28. Stajcic Z, Paljm A. Keratinization of radicular cyst epithelial lining or occurrence of odontogenic keratocyst in the periapical region. Int J Oral Maxillofac Surg. 1987 Oct;16(5):593-5. [ Links ]
29. Gulabivala K, Briggs PF. Diagnostic dilemma: an unusual presentation of an infected nasopalatine duct cyst. Int Endod J. 1992 Mar;25(2):107-11. [ Links ]
30. Wilcox LR, Walton RE. Case of mistaken identity: periapical cemental dysplasia in an endodontically treated tooth. Endod Dent Traumatol. 1989 Dec;5(6):298-301. [ Links ]
31. Philipsen HP, Srisuwan T, Reichart PA. Adenomatoid odontogenic tumor mimicking a periapical (radicular) cyst: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Aug;94(2):246-8. [ Links ]
32. Spatafore CM, Griffin JA Jr, Keyes GG, Wearden S, Skidmore AE. Periapical biopsy report: an analysis of over a 10-year period. J Endod. 1990 May;16(5):239-41. [ Links ]
33. Kuc I, Peters E, Pan J. Comparison of clinical and histologic diagnoses in periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000 Mar;89(3):333-7. [ Links ]
34. Walton RE. Routine histopathologic examination of endodontic periradicular surgical specimens--is it warranted. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Nov;86(5):505. [ Links ]
35. Stockdale CR, Chandler NP. The nature of the periapical lesion--a review of 1108 cases. J Dent. 1988 Jun;16(3):123-9. [ Links ]
36. Sanchis JM, Peñarrocha M, Bagan JV, Guarinos J, Vera F. Incidence des kystes radiculaires dans une série de 124 lésions périapicales chronique. Rev Stomatol Chir Maxillofac 1997;98:354-8. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Miguel Peñarrocha Diago
Cirugía Bucal. Clínicas Odontológicas.
Gascó Oliag 1
46021 Valencia. Spain
E-mail: Miguel.Penarrocha@uv.es
Received: 17-12-2006
Accepted: 29-09-2007