Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Pharmacy Practice (Granada)
versión On-line ISSN 1886-3655versión impresa ISSN 1885-642X
Pharmacy Pract (Granada) vol.5 no.4 Redondela oct./dic. 2007
| Original Research |
Pharmacist elicited medication histories in the Emergency Department:
Identifying patient groups at risk of medication misadventure
Maja AJDUKOVIC, Meredith CROOK, Christopher ANGLEY, Ieva STUPANS, Natalie SOULSBY, Christopher DOECKE,
Barbara ANDERSON, Manya ANGLEY.
| ABSTRACT The Australian Pharmaceutical Advisory Committee guidelines call for a detailed medication history to be taken at the first point of admission to an Emergency Department (ED). The elderly, in particular those residing in Residential Aged Care Facilities and those with a non-English speaking background, have been identified as patient groups vulnerable to medication misadventure. Key words: Medication Errors. Pharmaceutical Services. Medical Records. Communication Barriers. Australia. | RESUMEN Las guías del Comité Consultivo Farmacéutico Australiano establecen que se lleve una historia de medicación detallada desde el primer punto de entrada en un servicio de urgencias (SU). Los ancianos, en particular los que residen en Residencias de Ancianos y los que no son hablantes nativos ingleses, se han identificado como grupos de pacientes vulnerables a las desgracias medicamentosas. Palabras clave: Errores de medicación. Servicios farmacéuticos. Registros médicos. Barreras de comunicación. Australia. |
Maja AJDUKOVIC. BPharm(Hons), School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia.
Meredith CROOK. BPharm(Hons), School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia.
Christopher ANGLEY. MBBS FACEM, Senior Consultant in Emergency Medicine, Emergency Department, Royal Adelaide Hospital. Adelaide, Australia.
Ieva STUPANS. BPharm(Hons), PhD, Dean Teaching and Learning, Division of Health Sciences, University of South Australia. Adelaide, Australia.
Natalie SOULSBY. BPharm(Hons), MSc Clin Pharm, PhD Candidate, Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute, School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia.
Christopher DOECKE. BPharm, PhD, Director of Pharmacy Services, Royal Adelaide Hospital and School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia
Barbara ANDERSON. BPharm, BMgt(Hons), PhD, Senior Research Fellow, Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute, School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia
Manya ANGLEY. BPharm, PhD, Quality Use of Medicines and Pharmacy Research Centre, Sansom Institute, School of Pharmacy and Medical Sciences, University of South Australia. Adelaide, Australia.
INTRODUCTION
Medication misadventure presents a burden on the Australian health care system, accounting for 2.4% to 3.6% of all hospital admissions in general patients.1 Furthermore, it is estimated that up to 69% of all medication related admissions are potentially preventable.1 In developed countries elderly populations have a particularly high incidence of medication misadventure, accounting for up to 14 to 30% of all hospital admissions.2-9 Non-compliance is a major contributor to this problem, accounting for 21 to 59 per cent of medication related admissions in the elderly.2-4,6,8
A complete and accurate medication history, taken as soon as possible at the point of presentation, assists in identifying medication related problems that may have contributed to the presentation, as well as the potential medication related problems that may arise during the patient's admission.10 Medication histories, taken at the first point of hospital presentation within the Emergency Department (ED) are important in establishing appropriate and informed therapeutic treatment.11 Early identification of medication-related problems also facilitates early discharge planning and patient counselling10,12,13, particularly when patient non-compliance seems the likely cause of their presentation.
Pharmacists are ideally suited to eliciting medication histories as they have specialised knowledge of medications, including generic names, brand names, routes of administration, dosage forms; doses and adverse effects.12,14 However, medication histories are often compiled by staff least skilled to do so.14 Indeed, studies comparing medication histories recorded by a pharmacist to those of other ED staff have demonstrated that pharmacists are best suited to carry out this important role in patient care.12,15
Physicians and nurses have been estimated to only detect between 5% and 15% of medication related admissions9,15 in the absence of systemic surveillance systems, or dedicated personnel such as pharmacists. Furthermore, the primary activity of physicians does not focus on the frequency and significance of medication related admissions and thus they do not routinely screen for them.16 The problems arising from the failure to identify medication related admissions extends to subsequent prescribing, when an adverse drug reaction is mistaken for a new medical condition, leading to unnecessary drug treatment instead of treating the underlying cause.7 The presence of a pharmacist in the ED has been shown to decrease preventable adverse drug reactions as pharmacists help intercept errors as well as recognise ongoing medication related problems.13,15
Patients of non-English speaking background have been reported to have twice the medication error rate of English speakers17 as well as being more likely to be hospitalised as a result of medication misadventure. This has been attributed directly to language barriers18, such as the inability to read labels. Negative health outcomes have been shown to occur19, including higher rates of hospitalisation20, with patients relying on family members to translate and explain instructions. Jacobs et al19 have highlighted the importance of further research in the following areas: the ways in which language barriers affect health and health care, the efficacy of interpreter services, and the health economic impact of language barriers and development of strategies to minimise the impact. A pharmacist-elicited medication history service has been shown to be economically viable.21 A comprehensive medication history taken by a pharmacist has also been shown to decrease mortality rates.22 In the absence of appropriate interpreter services, it is likely the health benefits of a pharmacist-elicited medication history will be compromised.
When compared with people living independently, residents living in residential aged care facilities generally use more medications.23 Poly-pharmacy combined with advancing age puts these residents at high risk of an adverse drug event.24 Roughead et al25 reported 15 to 22% of emergency admissions in the elderly (aged greater than 65 years) were related to medication misadventure, posing a major public health problem in Australia. This is particularly important as it is reported that 50% of drug related hospitalisations are preventable.26 To minimise medication misadventure in residents of aged care facilities, there are currently two models under which a residential medication management review can be conducted. In one model, each residential aged care facility has an accredited review pharmacist contracted to perform medication reviews for residents, often in conjunction with the supply pharmacy contract. The second model, Medicare Benefits Schedule item 903, the collaborative residential medication management review, is a relatively new initiative that became available in November 2004. It is an item that was created to enable GPs and pharmacists to collaborate in reviewing the medication needs of aged care residents. Residents are eligible for this service if they have had a significant health event that places them at risk of medication misadventure.27
A study conducted by our research group has described the positive contribution an ED pharmacist can make to optimising compilation of medication histories for 100 patients presenting at an ED.13 It has previously been identified that residents living in residential aged care facilities and non-English speaking background patients are more vulnerable to medication misadventure. This paper describes sub-analysis of these demographic groups within the pharmacist-elicited medication histories in this cohort of patients. The paper also describes medication related ED presentations in this patient cohort.
The first aim of this project was to compare the current practices of medication history taking in the ED of the Royal Adelaide Hospital with best practice medication history taking as outlined in principle four of the Australian Pharmaceutical Advisory Committee guiding principles to achieve continuity in medication management.11 This guiding principle states that an accurate and complete medication history should be obtained and documented at the time of presentation or admission, or as early as possible in the episode of care. The second aim was to compare medication histories taken by ED personnel with those obtained by a Pharmacy Researcher in the following patient subgroups; 'general' patients, patients with a 'language barrier' and patients from a residential aged care facility. The third aim was to identify medication-related ED presentations and describe the incidence in these demographic groups.
METHODS
A detailed medication history form was developed specifically for the study. The form allowed for the recording of information regarding allergies, previous adverse drug reactions, social history, dose administration and other medication aids, vaccination status and previous medical history.
Patients identified as being at high risk of medication misadventure were specifically targeted. Inclusion criteria were:
• aged 70 years or older;
• taking five or more regular medications;
• diagnosed with three or more clinical co-morbidities, and/or
• at least one hospital presentation in the last three months.
Exclusion criteria:
• unable to nominate a regular GP and/or regular community pharmacy;
• unable to obtain consent;
The following process was undertaken for each patient included in the study:
1. Subject screening
Patients were screened according to age and triage category determined from the Hospital Administration Software System routinely used in the ED. The triage category ranges from one to five and reflects urgency for medical attention with category one being most urgent. Patients over the age of 70 and of the least urgent triage category were selected first.
2. Enrolment of subjects
Eligible patients were approached by the Pharmacy Researcher, provided with both verbal and written information regarding the project and asked to participate. The patients were informed that if they chose not to participate it would not in any way alter their treatment in the ED. Patients enrolled in the study were asked to sign a patient consent form. If patient was unable to provide consent, it was sought from their carer, who was asked to sign a "carer consent form". The patient was asked to nominate their regular community pharmacy and GP.
3. Interview
An interview was conducted in the absence of other ED staff and when applicable, in the presence of a carer and or other persons nominated by the patient. The interview did not delay patient's access to medical treatment, as the Pharmacy Researcher suspended the interview during any periods of medical assessment and treatment. The interview was then re-commenced following the completion of assessment and treatment.
4. Clarification of medication histories
Upon the completion of the patient interview, the Pharmacy Researcher contacted the patient's nominated GP and community pharmacy by telephone, advising them of the patient's consent to participate in the study. The researcher requested a faxed copy of the patient's medication history from both the GP and community pharmacy. The response time was recorded and previously reported.13
5. Clarification of discrepancies
A final comprehensive medication history was compiled by the Pharmacy Researcher from information gleaned from the patient interview as well as from the community pharmacy and GP faxed medication histories. The comprehensive medication history was reviewed for any potential medication-related problems and/or medication-related ED presentations. The final medication history was compared to the medication history complied by the ED physician and discrepancies identified. Discrepancies considered by Pharmacy Researcher to have a significant impact on the patient's treatment and or health outcomes were discussed and reconciled with the treating ED physician. ED physicians were alerted when possible medication related ED presentations were identified and strategies were developed between the ED physicians and Pharmacy Researcher to minimise recurrence and impact.
6. Inclusion of final medication history in patient notes
The final comprehensive medication history was included in the patient's medication folder.
7. Patient group sub analysis
For the purposes of sub analysis, patients were assigned to different groups. In order to be assigned to the 'language barrier' group, patients had to have English as a second language and deemed to require a translator by the Pharmacy Researcher for the purposes of compiling a comprehensive medication history. Patients who permanently resided in a residential aged care facility were assigned to the 'RACF' group and all other patients were classified as 'general'.
Approval for this project was granted by the relevant institutional ethics committees.
RESULTS
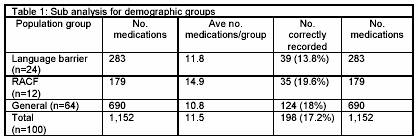
During the six week study period, 6,600 patients presented to the Royal Adelaide Hospital ED. Of these, 1,300 patients were over the age of 70, with 106 being interviewed, of whom 100 patients were included in the final study. This population comprised 42 males and 58 females, with the mean age of 80.1 (SD=5.7) (range, 70 - 96); 24 participants were classified as 'language barrier'; 12 participants were admitted from residential aged care facilities, and 64 participants were classified as 'general'. The average duration of a patient interview was 13.0 minutes (SD=6.0) as reported previously.13
For 20 of the 24 'language barrier' participants, an interpreter was present during the interview. In 18 cases, the interpreter was a spouse or child and in 2 cases, translation was carried out by a friend. For the remaining 4 cases, the comprehensive medication history was compiled from information obtained from the patient's nominated GP and community pharmacist. In a number of interviews, the interpreter answered for the patient, which was problematic when the interpreter did not live with the patient and/or was not familiar with their medications. The problem was overcome by asking the interpreter to translate the questions rather than answer for the patient and by directing the questions to the patient, not the interpreter. The Royal Adelaide Hospital ED has access to professional interpreters that are either employed or contracted by the hospital but they are not always immediately available when the patients who require their services present to the ED.
A total of 1,152 medications were recorded for the 100 patients in the study. When the Pharmacy Researcher or final medication histories were analysed, the average number of medications per patient was 11.5 (SD=4) (Range 5-23). The frequencies of medications taken were as follows: cardiovascular (28.1%, n=324), gastrointestinal (11.6%, n=134), endocrine (11.5%, n=132), anticoagulant/antithrombotic (8.9%, n=103), respiratory (7.4%, n=85), analgesic (7.4%, n=85), psychotropic (5.5%, n=63) and complementary and non-prescription medicine (5.3% n=61). Medications were categorised according to the Australian Medicines Handbook classifications.28
Comparison of medication histories recorded by ED medical staff and Pharmacy Researcher revealed that only 198 (16.4%) medications were recorded accurately by ED physicians. Medications omitted by ED medical staff was the most common discrepancy occurring for 48.9% (n=563) of the medications for the 100 study participants as reported previously.13
Sub analysis of the three demographic groups of interest is presented in Table 1.
Suspected medication related ED presentations were identified and categorised as medication related problems according to Gilbert et al29 which was based on the classification system developed by Cipolle et al.30 Suspected medication related ED presentations were later ranked to assess the likelihood of actually being a medication related admission. The ranking system that was used was adapted from the work of Naranjo et al31, who assigned the likelihood of a medication related admission according to a set of scored questions. There were 21 suspected cases of medication related ED presentations and 55.6% (n=15) were thought to be related to compliance and the adapted scale takes this into account.
A suspected adverse drug reaction (ADR) with a total score ≥9 is considered to be definitely caused by a drug, probably if the score is 5 to 8, possibly if 1 to 4 and unlikely if the score obtained is 0.
The 21 suspected cases of medication related ED presentations, were ranked according to the adapted scale (Table 2). Two cases were identified as definite and 19 cases (90.5%) as probable. There were a further two cases of suspected medication related ED presentations, but these were scored four or less on the probability scale. Table 2 outlines the 21 cases, of which 7 (33.3%) were 'language barrier'; 1 (4.8%) was from a residential aged care facility and 13 (61.9%) were from the 'general' category. All patients were subsequently admitted to hospital.
In terms of the total study population: 7 (29.2%) 'language barrier'; 1 (8.3%) residential aged care facility and 13 (20.3%) patients from the 'general' category were admitted for suspected medication related issues.
DISCUSSION
The results of this study confirm the vulnerability of patients with a language barrier to medication misadventure. Not only did this group have the lowest frequency of correctly recorded medications, but also it had the highest proportion of medication related hospital admissions.
These findings are significant as 16% or 2.8 million of the total Australian population speak a language other than English at home.32 Of these people, the lowest proficiency in the English language is found in those aged 65 years and over, of whom 40.2% do not speak English well or at all32; the population of interest in this study.
The difficulties associated with using family members or unqualified people as interpreters were experienced in this study. Several studies have shown that use of family and/or friends as interpreters has negative clinical consequences, such as a lower patient satisfaction, a lesser trust in the health professional, breach of patient confidentiality and inaccurate communication.19,33 The use of trained interpreters has been shown to result in a significantly higher quality of communication between the health professional and the patient and the recommendations for the use of trained interpreters in hospitals34-36 are supported by these findings. Furthermore, it is known that patients whose primary language is not English have a poorer understanding of the care they have received.19 It can be speculated that this includes advice regarding quality use of medicines. Therefore, it can be anticipated that they will be less likely to be concordant with their medications post-discharge highlighting the importance of access to interpreter services when they are seen by pharmacist at critical time points during admission particularly during discharge planning.
Patients from residential aged care facilities had the smallest number of omitted medications and the greatest number of correctly recorded medications (albeit 19.6%), which is despite the availability of residential aged care facility medication charts for these patients. Indeed, the availability of medication charts from residential aged care facilities may have resulted in the perception of treating staff that it was not necessary to record detailed medication histories. The medication related ED presentation of only one subject in the residential aged care facility category may be attributed to the fact that this group are entitled to annual residential medication management review s where medication related problems can be identified and medication related admissions minimised.
Patients from the 'general' category had similar numbers of medications omitted and correctly recorded as those from residential aged care facilities, but the second highest proportion of medication-related admissions (20%). This finding highlights the potential benefits of regular home medicines reviews, a service all participants in this study would qualify for, (excluding those who were clients of a residential aged care facility), as the inclusion criteria for participation in this study aligned with the criteria required for eligibility for an home medicines review referral. Emblem & Miller37 reported 6% of GPs referred patients at risk of medication misadventure rates for a home medicines review. This indicates that although patients meet the eligibility criteria, referrals for home medicines reviews are not optimal despite a vast array of support being available to improve home medicines reviews referral rates in the population at risk of medication misadventure.
This study has a number of limitations relating to its scope. First of all, it was conducted over the short time period of six weeks. A number of histories were conducted after normal business hours, up to 9:00 pm. As the majority of medical surgeries do not operate past 5.00-5.30 pm, it was often difficult to confirm medication histories with patient's nominated GP. The response from pharmacies was superior, as many community pharmacists have extended trading hours, often up to 7.00 pm or 9.00 pm. Secondly, the assumption was made that all patients presenting from residential aged care facilities had received an residential medication management review but this was not confirmed. It would have been informative to determine which residential aged care facility patients had previously received an residential medication management review and which 'general' patients had received an home medicines review. Finally, the study was confined to the ED. This prevented patient follow up on the wards and therefore the assessment of the impact that complete medication histories taken on admission may have had on patient outcomes. Another informative end point could have been the comparison of the discharge medication summary, which includes a list of medications plus an explanation for any changes or medication related issues that may have occurred in hospital, with the comprehensive medication history compiled by the Pharmacy Researcher.
CONCLUSION
This study confirms the vulnerability of patients with language barrier to medication misadventure and their need for interpreter services at all stages of their hospitalisation; in particular at the point of ED presentation. In particular, if pharmacists rely on other family members (sometimes a small child), friends, untrained non clinical employees or non fluent health care professionals to interpret when taking medication histories, the potential benefits of a pharmacist-elicited medication history will be mitigated. Furthermore, if interpreter services for patients with limited English proficiency are made a priority in the ED but also at timely encounters during their hospital admission, there is the potential to result in a range of additional improved patient health outcomes.
The findings also tend to confirm the value of regular residential medication management reviews which are carried out regularly in residential aged care facilities and the potential value of medication review via the home medicines reviews scheme for the 'general' population.
CONFLICT OF INTEREST
None declared.
| References |
1. Roughead EE, The nature and extent of drug-related hospitalisations in Australia. Journal of Quality in Clinical Practice 1999;19:19-22. [ Links ]
2. Col N, Fanale JE, Kronholm P, The role of medication non-compliance and adverse drug reactions in hospitalisations of the elderly. Arch Intern Med 1990;150:841-5. [ Links ]
3. Malhoutra S, Karan RS, Pandhi P, Jain S, Drug related medical emergencies in the elderly: role of adverse drug reactions and non-compliance. Postgrad Med J 2001;77:703-7. [ Links ]
4. Grymonpre RE, Mitenko PA, Sistar DS, Aoki FY, Montgomery PR, Drug-associated hospital admissions in older medical patients. J Am Geriatr Soc 1988;36(12):1092-8. [ Links ]
5. Mannesse CK, Derkx FH, de Ridder MA, Man in 't Veld AJ, van der Cammen TJ, Contribution of adverse drug reactions to hospital admission of older patients. Age Ageing 2000;29(1):35-9. [ Links ]
6. Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, Cadoret C, Fish LS, Garber L, Kelleher M, Bates DW, Incidence and Preventability of Adverse Drug Events among Older Persons in the Ambulatory Setting. JAMA 2003; 2889(9):1107-16. [ Links ]
7. Rochon PA Gurwitz JH, Optimising drug treatment for elderly people: the prescribing cascade. BMJ 1997;315:1096-99. [ Links ]
8. Chan M, Nicklason F, Vial J, Adverse drug events as a cause of hospital admission in the elderly. Intern Med J, 2001;31:199-205. [ Links ]
9. Chung MK Bartfield JM, Knowledge of Prescription Medications Among Elderly Emergency Department Patients. Ann Emerg Med 2002;39(6):605-8. [ Links ]
10. Welch S, The Evolving Area of Emergency Medicine Pharmacy. Aust J Hosp Pharm 1997;27:325-7. [ Links ]
11. Australian Pharmaceutical Advisory Council, Guiding Principles to achieve continuity in medication management. 2005, Canberra: Commonwealth of Australia. [ Links ]
12. Dodds LJ, An objective assessment of the role of the pharmacist in medication and compliance history taking. British Journal of Pharmaceutical Practice, 1982;4:12-23. [ Links ]
13. Crook M, Ajdukovic M, Angley C, Soulsby N, Doecke C, Stupans I, Angley M, Eliciting comprehensive medication histories in the emergency department: the role of the pharmacist. Pharm Pract (Internet) 2007;5(2):78-84. [ Links ]
14. McFadzean E, Isles C, Moffat J, Norrie J, Steward D, Is there a role for a prescribing pharmacist in preventing prescribing errors in a medical admission unit? Pharm J 2003;270:896-9. [ Links ]
15. Hohl CM, Robitaille C, Lord V, Dankoff J, Colacone A, Berard A, Pepin J, Afilalo M, Emergency Physician Recognition of Adverse Drug-related Events in Elder Patients Presenting to an Emergency Department. Acad Emerg Med 2005;12(3):197-205. [ Links ]
16. Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, Adverse Drug-Related Events, and Potential Adverse Drug Interactions in Elderly Patients Presenting to an Emergency Department. Ann Emerg Med 2001;38(6):666-71. [ Links ]
17. Fejzic JB, Tett SE. Medication management reviews for people from the former Yugoslavia now resident in Australia. Pharm World Sci 2004;26(5):271-6. [ Links ]
18. Baker DW, Parker RM, Williams MV, Pitkin K, Parikh NS, Coates W, Imara M. The health experience of patients with low literacy. Arch Fam Med 1996;5(6):329-34. [ Links ]
19. Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of Interpreter Services on Delivery of Health Care to Limited-English-Proficient Patients. J Gen Intern Med 2001;16(7):468-74. [ Links ]
20. Baker DW, Parker RM, Williams MV, Clark WS. Health Literacy and the Risk of Hospital Admission. J Gen Intern Med 1998;13(12):791-8. [ Links ]
21. Bond CA, Raehl CL, Franke T. Clinical Pharmacy Services, Pharmacy Staffing, and the Total Cost of Care in United States Hospitals. Pharmacotherapy 2000;20(6):609-21. [ Links ]
22. Bond CA, Raehl CL, Franke T. Clinical Pharmacy Services and Hospital Mortality Rates. Pharmacotherapy 1999;19(5):556-64. [ Links ]
23. Cheek J, Gilbert A, Ballantyne A, Penhall R. Factors influencing the implementation of quality use of medicines in residential aged care. Drugs Aging 2004;21(12):813-24. [ Links ]
24. Peterson G, Jackson S. Too many holes in the cheese when medication misadventure results in patient harm. Australian Pharm 2004;23(11):782-7. [ Links ]
25. Roughead EE, Gilbert AL, Primrose JG, Sansom LN. Drug-related hospital admissions: a review of Australian studies published 1988-1996. Med J Aust 1998;168(8):405-8. [ Links ]
26. Roughead L, Gilbert A, Medication misadventure. Australian Pharmacist 2002;21(2):90-4. [ Links ]
27. Department of Health and Aging. Medicare Benefits Schedule item 903. 2006 (cited 2006 viewed May15); Available from: <http://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=903&qt=item> [ Links ].
28. Rossi S, ed. Australian Medicines Handbook. ed. Rossi S. 2005, Australian Medicines Handbook: Adelaide. [ Links ]
29. Gilbert AL, Roughead EE, Beilby J, Mott K, Barratt JD. Collaborative medication management services: improving patient care. Med J Aust 2002;177(4):189-92. [ Links ]
30. Cipolle RJ, Strand LM, Morley PC, Pharmaceutical Care Practice. New York: McGraw-Hill; 1998. [ Links ]
31. Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, Domecq C, Greenblatt DJ. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30(2):239-45. [ Links ]
32. Australian Bureau of Statistics (2001) Older People, Australia: A Social Report, Chapter four: economic environment. [ Links ]
33. Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA 1996;275(10):783-8. [ Links ]
34. Hornberger JC, Gibson CD Jr, Wood W, Dequeldre C, Corso I, Palla B, Bloch DA. Eliminating language barriers for non-English-speaking patients. Med Care 1996;34(8):845-56. [ Links ]
35. Hornberger J, Itakura H, Wilson SR. Bridging language and cultural barriers between physicians and patients. Public Health Rep 1997;112(5):410-7. [ Links ]
36. Bajramovic J, Tett S. Problems of pharmacy communication in multicultural Australia. Australian Pharmacist, 2000;19(7):430-4. [ Links ]
37. Emblen G, Miller E. Home Medicines Review: the how and why for GPs. Aust Fam Physician 2004;33(1-2):49-51 [ Links ]