INTRODUCTION
Hypoglycemia is a condition featuring lower than normal levels of blood glucose. It can be defined as “mild” if episode is self-treated; “moderate” if assisted, and “severe” if hospitalised and assisted by physician (Diabetes Control and Complications Trial, 1993). Hypoglycemia could be classified as a true medical emergency, which left untreated may lead to organ and brain damage1. It is a significant complication of intensive diabetes therapy. Severe untreated hypoglycemia can cause significant economic and personal burden. Hence, identification and prevention of hypoglycemia are very important factors for prevention of hypoglycemic complications2. Diabetic medications, including insulin and sulfonylureas, are among the most common causes of hypoglycemia in diabetic subjects3. Occasional episodes of hypoglycemia with metformin are reported when an imbalance between food intake and dose of metformin2. According to Diabetes Audit and Research in Tayside Scotland (DARTS) study, severe hypoglycemia was observed in 7.3% and 0.8% of patients with Type 2 Diabetes Mellitus (T2DM) treated with insulin and oral sulfonylurea respectively. The risk of hypoglycemia is highest in those with T2DM, who have received insulin for more than 10 years4. T2DM patients lose, on an average, three productive days following a severe hypoglycemic attack. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Trial has demonstrated increased mortality rates in patients who experienced episodes of hypoglycemia. Repeated episodes of hypoglycemia can result significant mortality which is reportedly associated with a six fold increase in death. The clinical approach to minimize hypoglycemia while improving glycemic control includes addressing the issue, applying the principles of aggressive glycemic therapy, including flexible and individualized drug regimens, and considering the risk factors for iatrogenic hypoglycemia5. Main measures to prevent hypoglycemia includes drug counselling, meal plan, limiting the use of alcoholic beverages, and through appropriate diabetes management plan. The knowledge and education can also help patients to manage their glycemic conditions effectively along with pharmacological management6-12. Many health professionals rely on a verbal explanation, but this has been shown to be ineffective; patients tend to forget approximately half of the given information13. One method of providing information is to supply a patient information leaflet. It have also been shown to increase knowledge of drug side effects in a series of studies undertaken in the community14-15. The present study was undertaken to develop a patient information leaflet and evaluate the impact of it in education by pharmacist with respect to knowledge, compliance, life style, and glycemic control in T2DM patients with hypoglycemia. The effect of prescribed drugs pattern for the management of glycemic control in patients will also be investigated.
MATERIALS AND METHODS
Study design
The open labelled, interventional study was conducted in the endocrinology outpatient department in a tertiary care hospital for a period of 9 months from June 2015 to February 2016 . Institutional Ethics Committee (IEC) approval was taken before initiation of the study.
Sample size calculation
Sample size was calculated as 55 based on the outpatient statistics of endocrinology department. Raosoft sample size calculator with margin of error 5%, confidence level 95%, and probability was used for calculation. A total of 385 diabetic patients were screened out of which 100 hypoglycemic patients were identified. Fifty five patients were included in the study based on the inclusion and exclusion criteria.
Inclusion and exclusion criteria
Both male and female hypoglycemic patients of age >18 years diagnosed with T2DM were included. Patients on Oral Hypoglycemic Agents (OHA’s) and/or insulin were included in the study. Pregnancy, lactation, psychosis, mental retardation, active substance abuse, and significant depression patients were excluded from the study. Patients who were not willing to provide consent were excluded from the study.
Patient Information leaflet development
Before the main study, a preliminary study was carried out with 10 consecutive hypoglycemic literate and illiterate patients who were attending the outpatient clinic. First step of the study was patient interaction, which helped us identifying various barriers such as poor knowledge about the condition, lack of compliance towards treatment, lifestyle, and poor medication adherence. After assessing the barriers, a questionnaire was prepared based on diabetic patients perception about hypoglycemia and its management. The institution developed questionnaire in vernacular language was validated by two expert endocrinologists in the study site. The questionnaire was an effective tool to identify patient problems in order to give an effective education. The questionnaire cited (Table 1) includes 20 questions under 4 different categories like knowledge (9 questions), compliance (5 questions), life style (3 questions), and glycemic control (3 questions) , which was tested in preliminary study 2 in 10 literate and illiterate patients. None experienced problems with its readability in vernacular language and the patients thought that the patient information leaflet based on the 20 questionnaire, answered the queries they would raise about hypoglycemia and it’s management. Based on this, a comprehensive patient information leaflet was prepared. A data collection form was also designed to record laboratory values, including blood glucose level and other patient specific details. Informed consent from all patients was collected before participation, briefing them about the study in colloquial language.
Table 1: Hypoglycemia Questionnaire
| Parameter | Questions |
|---|---|
| Knowledge | Do you know what diabetes is? a) It is an abnormal increase in blood glucose levels in human body. 2) Do you know what the types of diabetes are? Increase in blood glucose due to absence of insulin producing cells. Increase in blood glucose because the cells doesn’t take up the insulin. Increase in blood glucose during pregnancy. Increase in blood glucose due to other reasons. 3) Do you know what hypoglycemia is? a) It is an abnormal lowering in blood glucose levels in human body. 4) Do you know what HBA1c is? a) It is the average level of blood glucose. 5) Do you know what the symptoms of hypoglycemia are? Headache Feel shaky Sweating Feel hungry Rapid heart beat Drowsiness Difficulty in talking Blurred vision Double vision 6) Is diabetes a hereditary disease? (Yes/No) 7) Do you regularly take your medications as advised by the doctor? (Yes/No) 8) Do you know what insulin is? a) Insulin is a key that opens the cells to take up glucose. 9) Do you have a glucometer? Do you know how to use it? (Yes/No) |
| Compliance | 1) How often do you check your blood glucose? a) Once in a month or whenever sugar level is to be checked. 2) How often do you check your HBA1c values? a) 1 to 3 months. 3) What precautions do you take to prevent or treat hypoglycemic episode? a) Keep candy or chocolate. b) Check your blood glucose level regularly 4) Do you know how to treat hypoglycemia immediately? 2 to 3 spoon of glucose powder Half cup of any fruit juice 5 or 6 piece of hard candy One tablespoon of sugar 5) What have you done to prevent further episodes of hypoglycemia? Reducing the dose of insulin Reducing the dose of tablets Eating more food(rich in carbohydrate) |
| Life style | 1) At what time of the day there is high risk of hypoglycemic episode? a) Night 2) Do you exercise regularly? (Yes/No) 3) Have you ever met a dietician for dietary counseling regarding diabetes mellitus? (Yes/No) |
| Glycemic control | 1) What are the normal blood glucose levels? FBS<100 RBS>100 PPBS<140 2) Do you know, below which level the hypoglycemia is happening? a) Below 70 mg/dL 3) Is there any improvement in your blood glucose than the previous blood glucose levels? (Yes/No) |
Method of assessment
Patient information leaflet (Table 2) was given to the patient and the questionnaire was read out to them. Marks were recorded based on the answering pattern after their enrolment in the start of the study (baseline) and during revisit at sixty days interval (final). Scoring of marks was done at the baseline and in final based on 1 for Yes and 0 for No. The assessment was done based on the patient questionnaire marks and glycemic status. The quantitative variables related to glycemic status like Fasting Blood Sugar (FBS) and Post Prandial Blood Sugar (PPBS) and the other parameters related to patient information leaflet like knowledge, compliance, lifestyle and glycemic control were recorded. The changes in the variables and parameters before and after the patient information leaflet education were recorded.
Table 2: Patient Information Leaflet
| HYPOGLYCEMIA: | Hypoglycemia or hypo, is the lowering of blood glucose level below 70 mg/dL.This is too low to provide sufficient energy for your body activities. Hypoglycemia can happen when you are treated with insulin or certain diabetes medication. No matter how much you know about diabetes or how careful you are, if your diabetes is treated with certain medication, you are likely to experience some hypoglycemia. Leaflet is designed to give you information to prevent, recognize and treat hypoglycemia. |
| SYMPTOMS: | Sweating Hungry Tingling Tremor Heart pounding Difficulty in speaking warm weak confused Tired/drowsy Faint/dizzy. |
| CAUSES: | Too much insulin/too many tablets. Delayed or missed meal or snack. Not enough food, especially carbohydrate. Unplanned or strenuous activity. Drinking too much alcohol or alcohol without food. |
| IMMEDIATE TREATMENT: | 2 to 3 spoons glucose powder. Half cup of any fruit juice Half cup of a regular soft drink 5or 6 piece of hard candy 1 table spoon of sugar, if anyone |
| FOLLOW ON TREATMENT: | To prevent the blood glucose dropping again, you should follow your sugary foods with a starchy carbohydrate snack.eg: a sandwich, fruit, a bowl of cereal, biscuits and milk, the next meal if it’s due. |
| MANAGEMENT OF HYPOS AT NIGHT: | Check your blood glucose between 2 am and 3 am when hypos are most likely to happen. Keep something sugary by your bed. Alternatively have a bed-time snack such as biscuits and milk, sandwich, fruit or yogurt. |
| HYPOS AND PHYSICAL ACTIVITY: | Physical activity lowers your blood glucose level, so it is important to eat some form of carbohydrate before hand, and possibly during and after your activity if it is strenuous or lasts a long time. Hypos can happen up to 36 hours after strenuous or prolonged physical activity so you might need to adjust your medication or carbohydrate intake. |
| HYPOS AND DRIVING: | Always test your blood glucose levels before driving. If you feel you may be experiencing a hypo, pull over, stop the car and remove the keys from the ignition. |
| HYPOS AND ALCOHOL: | During a lot alcohol or drinking on an empty stomach makes a hypo more likely. The signs of a hypo are also very similar to those of being drunk. Always have something to eat if you are drinking alcohol, and tell the people you are with about your diabetes and what to do if you need help treating a hypo. |
| IMPORTANT POINTS TO REMEMBER: | Always have something sugary with you for use in an emergency. Always carry/wear some form of identification specifying you have diabetes and your treatment. Tell your friends, relatives and colleagues that you have diabetes and let them know how to help if you have a hypo. |
Statistical analysis
Data was statically analysed using student’s t test (graph pad prism version 5). Statistical significance was taken at 95% CI (p<0.05) using SPSS 16 version. The multivariable studied and analyzed were knowledge, compliance and lifestyle, and glycemic control. P values<0.05 were accepted as statistically significant
Ethics
This study was in accordance with the Ethics Committee of the institution (protocol no: 14/272). Permission was taken from the hospital administrators. After revealing the aim and duration of the study to the participants, the participants were announced that they could leave the study whenever they wanted. Written informed consent was provided from all the participants/Care takers.
RESULTS
Out of 55 patients included in the study, 26 patients had a family history of T2DM. Regarding the literacy of patients, 47 (85.45%) patients were literate, 8 (14.54%) patients were illiterate. Patients who did not complete high school education were categorised as illiterate persons. Among the subjects, 17 (30.90%) were alcoholic, 20 (36.36%) were smokers.
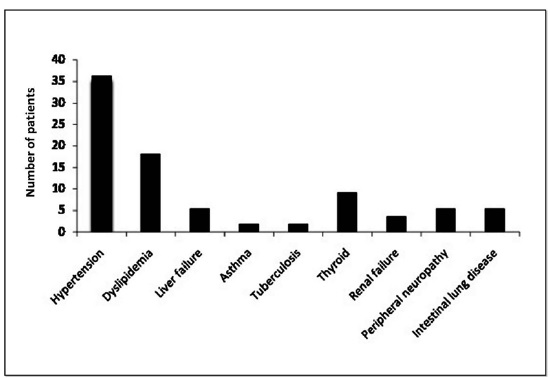
Hypoglycemic episodes were more prevalent in the age group of 50-59 years in both male and female patients followed by the age group of 60-69 years (Table 3). Hypertension and dyslipidemia were the co morbidities in the study subjects and the other co morbidities are shown in Figure 1.
Patients were on antihypertensive and dyslipedmic drugs in addition to drugs controlling diabetes. The treatment aspects of the male and female patients are shown in (Table 3). Combinations of drugs were observed in the diabetic treatment schedule, which may delay the need for insulin or in combination with insulin aid in achieving glycemic goals.
Table 3: Multivariate analysis of dependent variables
| Source | Dependent Variable | Type III sum of squares | Degree of freedom | Mean square | Distribution | Significance |
|---|---|---|---|---|---|---|
| Education | Knowledge | 437.527 | 1 | 437.527 | 133.270 | 0.000 |
| Compliance | 170.909 | 1 | 170.909 | 34.573 | 0.000 | |
| Lifestyle | 109.382 | 1 | 109.382 | 22.127 | 0.000 | |
| Glycemic control | 553.745 | 1 | 553.745 | 156.109 | 0.000 | |
| Gender | Knowledge | 0.000 | 1 | 0.000 | 0.000 | 1.000 |
| Compliance | 7.969 | 1 | 7.969 | 2.988 | 0.090 | |
| Lifestyle | 13.015 | 1 | 13.015 | 1.753 | 0.191 | |
| Glycemic control | 17.169 | 1 | 17.169 | 7.428 | 0.009 | |
| Age | Drugs | 12.363 | 5 | 2.473 | 0.985 | 0.438 |
| Changes in fasting blood sugar | 866.320 | 5 | 173.264 | 4.288 | 0.003 | |
| Gender | Drugs | 2.390 | 1 | 2.390 | .952 | 0.334 |
| Changes in fasting blood sugar | 128.267 | 1 | 128.267 | 3.174 | 0.082 |
Patients treated with sulfonylurea along with biguanides (n=6) the fasting blood sugar level was less and closer to 70 mg/dl hence the hypoglycaemic chances are more (Table 4).
Table 4: Effect of anti-diabetic therapy on glycemic status in hypoglycemic patients
| Age (years) | Male (N) | Female (N) | Percentage (%) | No. of patients | Anti-diabetic therapy regimens | FBS mg/dl | PPBS mg/dl | ||
|---|---|---|---|---|---|---|---|---|---|
| Baseline ME±SD | Final ME±SD | Baseline ME±SD | Final ME±SD | ||||||
| 20-29 | 1 | 2 | 10.84 | 1 | SOHA (B and AGI) | 68 | 90 | 120 | 132 |
| 1 | COHA (S+B) | 68 | 66 | 99 | 95 | ||||
| 1 | SOHA (B) | 65 | 78 | 93 | 103 | ||||
| 30-39 | 0 | 4 | 14.28 | 3 | SOHA (B) | 72 ±1.41 | 81.5±4.9 | 96 ± 4.85 | 114±2.8 |
| 1 | SOHA (B and fI) | 69 | 84 | 92 | 110 | ||||
| 40-49 | 3 | 7 | 36.11 | 1 | COHA (S+B) | 68 | 65 | 90 | 99 |
| 4 | SOHA(B) | 142.6 ±5.9 | 155.6±1.2 | 215.6±7 | 230.6±3.50 | ||||
| 1 | SOHA&COHA ( B) (S+ B) | 69 | 67 | 96 | 103 | ||||
| 4 | SOHA and I (B and I) | 142.3 ±1.5 | 157.5±2.4 | 198.6±1.5 | 229.3 ±0.3 | ||||
| 50-59 | 11 | 9 | 72.88 | 2 | COHA (S + B) | 67 | 67 | 99 | 97.5 |
| 6 | SOHA(B) | 149±8.04 | 167.7±3.9 | 207.5±5.1 | 228±8.14 | ||||
| 10 | SOHA and I (B and I) | 147.6±6.7 | 180.12±8.9 | 214.2±7.5 | 227.2±5.83 | ||||
| 2 | SOHA(AGI)and I | 64 | 80.5 | 92.5 | 113.5 | ||||
| 60- 69 | 9 | 5 | 51.18 | 3 | COHA (S + B) | 71.3±5.6 | 70.6±6.6 | 99.6±15.3 | 108.3±18.9 |
| 2 | SOHA (B) | 136 | 150 | 177 | 206 | ||||
| 7 | SOHA& I (B & I) | 142.6±2.8 | 160±5.2 | 191.3±8.5 | 198.3±7.8 | ||||
| 2 | COHA& I (S+B& I) | 64 | 80.5 | 92.5 | 113.50 | ||||
| 70-79 | 3 | 1 | 14.68 | 2 | COHA(S+ B) | 69 | 65.50 | 87.5± | 89.50 |
| 1 | SOHA(B) and I | 71 | 73 | 90 | 103 | ||||
| 1 | SOHA&COHA (B) (S + B) | 62 | 65 | 84 | 90 | ||||
SOHA- Single Oral Hypoglycemic Agent, AGI - Alpha glucosidase Inhibitors, COHA- Combination Oral Hypoglycemic Agent, S- Sulfonyurea, B- Biguanide, I-Insulin, FBS: Fasting blood sugar, PPBS: Post Prandial Blood Sugar, Combination of Single Oral Hypoglycemic Agent and Combination Oral Hypoglycemic Agent, N Number , Mean ± SD average value of determinations.
The baseline and final value of knowledge status were 10.86±6.01 and 21±4.39 respectively with a value (p<0.001). The baseline and final value of glycemic control were 9±7.89 and 17.17± 6.79 with a value (p<0.009) (Table 5).
Table 5: Effect of patient information leaflet education by pharmacist in hypoglycemic patients
| Parameter | Baseline | Final | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male ME±SD | Female ME±SD | Literate ME±SD | Illiterate ME±SD | Male ME±SD | Female ME±SD | Literate ME±SD | Illiterate ME±SD | Male | Female | Literate | Illiterate | |
| Knowledge | 10.86±6.01 | 12.14±7.10 | 32±7.25 | 2.43±0.97 | 21±4.39 | 21.71±5.93 | 39.86±5.81 | 2.86±1.34 | 0.001* | 0.004* | 0.01* | 0.07 |
| Compliance | 15±8.18 | 16.33±6.42 | 36±6.24 | 2.67±0.57 | 21.67±4.04 | 22.33±5.50 | 41±4.58 | 3.33±0.57 | 0.12 | 0.02* | 0.03* | 0.18 |
| Life style | 11.50±8.85 | 14.50±9.46 | 30.25±5.5 | 2±0.81 | 21±4.69 | 23±6.68 | 34.75±5.62 | 2.50±1.29 | 0.08 | 0.10 | 0.061* | 0.182 |
| Glycaemic control | 9±7.89 | 9.17±9.62 | 29.17±9.62 | 2.33±0.81 | 17.17±6.79 | 18.33±7.36 | 39.33±6.47 | 2.83±1.16 | 0.009* | 0.01* | 0.029* | 0.076 |
*paired t-test indicating significance. Mean ± SD average value of determinations
Literate study subjects showed significant improvement in knowledge, compliance, and glycemic control after conveying the relevant information through patient information leaflets. The baseline and final value of knowledge status were 32±7.25 and 39.86±5.81, respectively, with a value (p<0.01). The baseline and final value of compliance were 36±6.24 and 4±4.58, respectively, with a value (p<0.03). The base line and final value of glycemic control were 29.17±9.62 and 39.33±6.47, respectively, with a value (p<0.02) as depicted in (Table 5).
DISCUSSION
Hypoglycemic findings with respect to age group are similar to the observations by the Decoda study group stating that the prevalence was over 30% among those aged 50-69 years17.
The advantage of differing mechanisms of action, in combination therapy as a mean of optimizing glycemic control was also observed in the treatment pattern. In multivariate analysis, age and gender does not associate with prescribing practice of anti-diabetic drugs ( Table 3). Patients receiving combination oral hypoglycemic agents (n=6), sulfonylureas (Gliclazide or Glimepride) along with biguanides experienced more hypoglycemic episodes than those on biguanides alone (n=16).
Multivariate analysis confirmed age (p<0.01) have an effect on hypoglycemic states of patients (Table 3). But gender doesn’t affect the hypoglycemic states. In the age group 30-39, 40-49, and 50-59 treated with biguanides alone have shown both FBS and PPBS high. Similarly treatment with biguanides and insulin combination in the age group showed statistically significant (p<0.05) higher level fasting blood sugar level after treatment in the age group (n=21) of 40-49, 50 - 59 and 60-69 years. Hence the hypoglycemic chances are less (Table 4). At the same time we have also also observed that combination of oral hypoglycemic agents (sulphonamides and biguanides) in the age group 50-59, 60-69, 70-79 showed less FBS level but increased PPBS level.
The study results also confirm that biguanides and insulin medication combination maintains fasting blood sugar without hyplglycemia when compared to sulphonyl area with biguanides. Post Prandial Blood Sugar (PPBS) level remains more than 84 mg/dl in all groups with respect to the baseline and final values after treatment (Table 4).
As expected at the onset of the study, both male and female patients knew little about hypoglycemia and this was noted through the baseline score. In this study, there was a considerable improvement in all parameters of hypoglycemic awareness status in male and female patients. Patient knowledge, compliance and lifestyle factor has not been affected by means of gender, but it significantly affects glycemic control (p<0.01) in multivariate analysis. Concurrently, education (p<0.0001) have significantly influence on patient knowledge, compliance and lifestyle factor as well as glycemic control (Table 3).
The literacy have significantly influenced on patient knowledge, compliance, lifestyle factor as well as glycemic control compared to illiterates. Illiterate showed improvement in knowledge, compliance, life style, and glycemic control (Table 5), the level of significance is not perceptible in any of the parameters and this may be due to the small sample size of patients enrolled in the study. This also indirectly confirms that the developed patient information leaflet was concise at readable level, in more easily understood format and increased patient knowledge about hypoglycemia.
This information empowers literate patients to become more involved in the decision making and hypoglycemia management process. Paulose carried out disease awareness study in 400 literate diabetic patients in kerala. The study found that although 80% of patients knew the symptoms of hypoglycemia and 76% knew what to do when they develop these symptoms, only 17% carried glucose packets with them during travel and 29% patients told that their doctors did not inform them about hypoglycemic complications17. These studies suggest that it is essential to educate the patients regarding proper diet, exercise, glucose control, and periodic consultations(1, 6, 11, 18).
Our study results also showed the impact of pharmacist education in the significant improvement about diabetes knowledge, compliance, and glycemic control in hypoglycemic patients. Patient involvement is essential for successful management of hypoglycemia Educational efforts are also necessary to improve self-management of hypoglycemia in diabetic patients. Along with other health care professionals, role of pharmacist as diabetic counsellor is much appreciated in many developed countries.
Although improving patients knowledge on hypoglycemia through patient information leaflet is a laudable aim, it is acknowledged that knowing and understanding are different entities and consequently it cannot be assumed from the results of this study.
The effect of antidiabetic therapy on glycemic status with respect to different age group and duration of diabetes was not determined due to the small sample size among the groups. Further long duration studies covering a large population are needed to validate the data.
CONCLUSION
Our study confirms the patient´s knowledge and glycaemic control in out-patients with type 2 diabetes mellitus with hypoglycemia can be overcome through the development of patient information leaflet and education by a pharmacist. The study confirmed the impact in the knowledge about diabetes, compliance, and glycemic control in hypoglycemic patients significantly (p<0.05). Treatment pattern highlights hypoglycemic risk is less in most age groups treated with biguanides alone and biguanides with insulin compared to sulphonylureas with biguanides.