My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Angiología
On-line version ISSN 1695-2987Print version ISSN 0003-3170
Angiología vol.75 n.4 Madrid Jul./Aug. 2023 Epub Nov 27, 2023
https://dx.doi.org/10.20960/angiologia.00468
Originals
Early experience with preventive embolization of the inferior mesenteric artery in the endovascular treatment of abdominal aortic aneurysms
2Angiology, Vascular and Endovascular Surgery Department. Hospital Universitario Fundación Jiménez Díaz. Madrid, Spain
Introduction:
type II endoleak (T2EL), through the inferior mesenteric artery (IMA) or lumbar arteries (LA), is the most common endoleak after endovascular abdominal aortic aneurysm repair (EVAR).
Objectives:
the primary endpoint was the presence of type II endoleak at follow-up. Secondary endpoints included aneurysm sac regression and reoperation rate due to T2EL, as well as the analysis of the results in our series of cases treated with IMA embolization prior to the endovascular procedure as a useful method to reduce T2EL at follow-up.
Material and methods:
this was a retrospective analysis of patients treated at our unit with IMA embolization prior to EVAR from 2019 through 2021. The criteria used for IMA embolization were IMA diameter > 3 mm, presence of LA with a diameter > 2 mm, or aortoiliac aneurysms. A total of 7 male patients were included with a mean age of 72.1 years. A total of 42 % had aortoiliac aneurysms. In 2 of the cases, IMA embolization was performed initially followed by EVAR while in the remaining cases it was performed within the same procedure. The mean diameter of IMA was 5.02 mm ± 0.9 mm. All patients had at least 2 LAs facing the origin of the IMA with a diameter > 2 mm.
Results:
technical success was 100 %. The median follow-up was 20.7 months. In the CCTA performed 1 month and 12 months postoperatively, correct IMA embolization was observed. There were no type II leaks at follow-up. In all cases, a decrease in the diameter of the aneurysmal sac was observed with a mean regression of 5.08 mm. There were no subsequent reinterventions associated with aortic valve disease.
Conclusions:
IMA embolization prior to EVAR in patients with a diameters > 3 mm and the presence of at least 2 ALs with diameters > 2 mm and/or aortoiliac aneurysms seems to protect against the development of T2EL at 12 months, waiting to be able to confirm the results in the mid- and long-term with high technical success and an acceptable regression of the aneurysmal sac.
Keywords: Endoleak; EVAR; Inferior mesenteric artery; Embolization
INTRODUCTION
Endovascular aortic aneurysm repair (EVAR) of abdominal aortic aneurysm (AAA) has been shown in numerous randomized clinical trials to offer advantages over open repair like shorter lengths of stay, lower rates of cardiac and respiratory complications, and reduced need for transfusions. However, one of the main complications of endovascular therapy is the presence of intraoperative endoleaks or at follow-up (1-3).
An endoleak is the presence of flow within the aneurysm sac after EVAR (4). The most common type is type II endoleak (T2EL), which occurs in 20 % to 40 % of cases and is due to retrograde flow into the aneurysm sac from the lumbar arteries (LA) or the inferior mesenteric artery (IMA). Some studies have concluded that T2EL due to IMA has a worse prognosis (4,5).
The growth of aneurysm sac can lead to an increased number of reinterventions and even an increased risk of rupture (4).
Preventive embolization of the IMA has been proposed as a valid option to prevent T2EL at follow-up and reduce the diameter of the aneurysm sac (6-8).
Our objective is to evaluate the outcomes in our series of cases treated with pre-implantation embolization of the IMA as a useful method to reduce T2EL at follow-up.
MATERIALS AND METHODS
Population
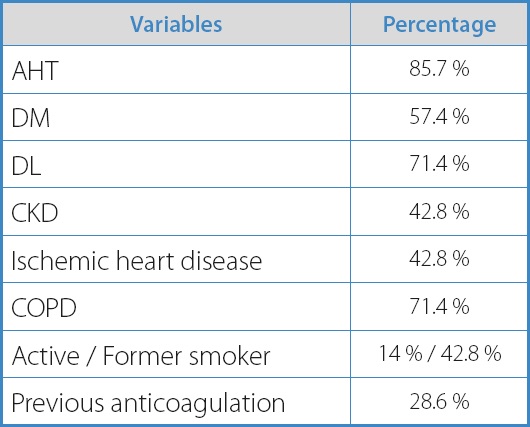
A retrospective analysis was conducted on patients treated at our center with pre-embolization of the inferior mesenteric artery (IMA) prior to EVAR from 2019 through 2021. The demographic data of the patients are shown on table I.
The criteria used for IMA embolization were diameters > 3 mm with the presence of at least 2 LAs with diameters > 2 mm facing each other at the exit of the IMA or the coexistence of aortoiliac aneurysms. These criteria are supported by the recently published randomized clinical trial conducted by Samura et al. (9).
In 2 cases, IMA embolization was performed as a first-stage procedure followed by EVAR while in the other 5 patients, it was performed during the same procedure. These 2 patients had concomitant bilateral iliac aneurysms. First, the embolization of IMA and one of the hypogastric arteries was performed. Afterwards, in a second stage (2 weeks later), the endovascular procedure was completed with EVAR and extension to the external iliac artery (EIA) in the axis with previous hypogastric embolization + iliac branch in the contralateral iliac axis.
Procedure
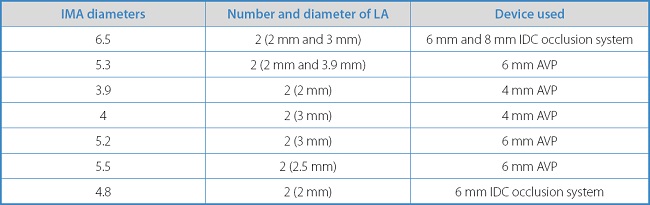
Embolization was ultrasound-guided and performed under regional anesthesia and via femoral access. A 6-Fr introducer shead was placed followed by a 0.035 in guidewire supported by a 4-Fr catheter. Once the ostium of the IMA was catheterized, embolization was performed using 6 mm and 8 mm Interlock coils (Boston Scientific, Marlborough, MA, United States) or 6 mm and 4 mm AVP II devices (St. Jude Medical, St. Paul, MN, United States) as shown on table II.
Technical success was defined as occlusion of the IMA ostium with patency of its distal branches on the final arteriography.
At the end of the procedure, patients spent the first 12 hours in the recovery room, and in the absence of complications, they were transferred to the hospital ward to complete the postoperative period.
Endpoints
The study primary endpoint was to assess the outcome of IMA embolization in preventing T2EL. The study secondary endpoints included aneurysm sac regression and the rate of reintervention due to T2EL.
Preoperative images
Preoperative CCTAs were performed with 0.75 mm slices in all patients. Measurements of the aorta were performed using Philips IntelliSpace 9.0 medical imaging software. The following measurements were included: diameter of the IMA, maximum diameter of the aneurysm sac, diameter and length of the proximal neck, diameter and length of the common iliac arteries, and number and diameter of the lumbar arteries.
The mean aortic diameter prior to the endovascular procedure was 58 mm (range 40 mm to 90 mm). A total of 42 % of the patients had aortoiliac aneurysms. The mean diameter of the IMA on the preoperative CCTA was 5.02 mm ± 0.9 mm. Regarding the embolization device, an Amplatzer vascular plug (AVP) was used in 5 cases, and coils in the remaining 2 cases.
All patients had at least 2 LAs facing the origin of the IMA with diameters > 2 mm.
Postoperative images
Regarding follow-up, control CCTAs were performed at 1 and 12 months while the 6-month follow-up was conducted using ultrasound. In the absence of T2EL, annual follow-ups were conducted with ultrasound and abdominal X-rays. Due to other conditions, some patients underwent abdominal CT scans that were used for measuring purposes at follow-up.
RESULTS
Between 2019 and 2021, preventive embolization of the IMA was performed in 7 male patients who subsequently underwent EVAR. The mean age was 72.1 years.
Technical success was achieved in 100 % of cases with a median follow-up of 20.7 months (12.9 months-26.3 months).
A median aneurysm sac regression of 5.08 mm (range, 2 mm to 14 mm) was observed, which was significantly greater in patients without associated iliac aneurysms (p < 0.01).
The median length of stay for patients who underwent simultaneous embolization and EVAR was 36 hours (34 h to 37 h). However, for patients who underwent embolization without immediate EVAR, the mean length of stay was 24 hours (22 h to 28 h).
On the CCTAs performed at 1 and 12 months postoperatively, successful embolization of the IMA with patency of its distal branches was observed. No type II endoleaks occurred at follow-up.
No complications associated with the puncture site or mesenteric ischemia were seen at follow-up. There were no subsequent reinterventions either associated with aortic valve disease.
DISCUSSION
Numerous studies have demonstrated that the presence of type II endoleaks (T2EL) after EVAR is directly associated with the patency of the IMA and lumbar arteries (8-10). In the prospective randomized study conducted by Samura et al. (9), they concluded that preventive embolization of the IMA in high-risk patients with similar preoperative characteristics to those from our study reduces the occurrence of T2EL at follow-up (24.5 % vs 49.1 %, p = 0.009).
Burbelko et al. (10) demonstrated that the blood flow generated by the presence of T2EL can transmit pressure to the aneurysm sac, thereby increasing the risk of rupture. On the other hand, other authors believe that type II endoleaks can be managed conservatively without sac growth since up to 58 % resolve spontaneously (10-13).
In our center, of all EVAR procedures performed in recent years, type II endoleaks have been reported in 20 % of cases at follow-up. The most common complication is the progressive increase in the diameter of the aneurysm sac followed by the need for reinterventions, while the incidence rate of rupture is very low. In most cases, this T2EL was dependent upon the IMA that had diameters > 3 mm, which is why the embolization of IMA was planned as a preventive method of the presence of T2EL. Currently, based on the results obtained, we are performing exclusive IMA embolization followed by EVAR in all patients who meet the previously described embolization criteria with short-term results similar to those described here.
Former studies (14-16) have said that the embolization of both the IMA and LAs further reduces the occurrence of T2EL compared to the embolization of the IMA alone, achieving a decrease in the presence of endoleaks from 3.6 % down to 47.8 % in the control group. However, the study conducted by Alerci et al. (14,16) reported that embolization of the LA was technically challenging due to their small diameter and tortuosity, resulting in a longer procedure time and lower success rate (around 60 %). In cases where embolization of the IMA was performed but embolization of all the LAs was not feasible, no growth of the aneurysm sac was seen.
Another study recently published recommends embolization of the LAs prior to EVAR when they have an internal diameter ≥ 2.0 mm and a maximum aortic luminal diameter without thrombus ≤ 36.1 mm as it is more feasible to cannulate the LAs with smaller aortic diameters. However, the success rate they achieved was 73 % compared to the 96 % achieved with IMA embolization only (15).
Among the results found in the medical literature available regarding exclusive embolization of the IMA prior to endovascular procedures, high success rates (from 93.8 % up to 100 %) with a low rate of complications (close to 0 %) (6-8,18), a significanty low presence of T2EL and a reduced aneurysm sac diameter have been reported. Only the study conducted by Ward et al. (8) reported the death of 1 patient due to ischemia. However, this patient had previously undergone a hemicolectomy.
Most publications show the results of preventive embolization, but there are fewer articles that report the results of IMA embolization in a second stage in case of endoleaks reported at follow-up. In the meta-analysis published by Karh et al. (19), they obtained a technical success rate of 71.5 % for the treatment of T2EL after EVAR, thus advocating for IMA embolization before EVAR.
Out study main limitation is the small number of included patients and the short follow-up period (12 months). This is a retrospective and single-center study, which means that, in the future, a prospective and randomized trial could be considered to confirm the promising results obtained regarding the reduction of T2EL.
CONCLUSION
In conclusion, preoperative embolization of the IMA prior to EVAR in patients with diameters > 3 mm and the presence of, at least, 2 LAs with diameters > 2 mm or aortoiliac aneurysms appears to be protective against the development of T2EL at 12 months. Further confirmation of these results is needed in the mid- and long-term. The procedure shows high rates of technical success and significant aneurysm sac regression.
Díaz Cruz J, González García A, Arízaga Idrovo VC, Baeza Bermejillo C, Arribas Díaz AB, Aparicio Martínez C. Early experience with preventive embolization of the inferior mesenteric artery in the endovascular treatment of abdominal aortic aneurysms. Angiología 2023;75(4):212-217
REFERENCES
1. Greenhalgh RM, Brown LC, Powell JT, et al. Endovascular versus open repair of abdominal aortic aneurysm. New Engl J Med 2010;362(20):1863-71. [ Links ]
2. De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. New Engl J Med 2010;362(20):1881-9. [ Links ]
3. Lederle FA. Outcomes following endovascular vs open repair of abdominal aortic aneurysma randomized trial. JAMA 2009;302(14):1535. [ Links ]
4. White GH, May J, Waugh RC, et al. Type III and type IV endoleak: Toward a complete definition of blood flow in the SAC after endoluminal AAA Repair. J Endovasc Ther 1998;5(4):305-9. [ Links ]
5. Baum RA, Carpenter JP, Tuite CM, et al. Diagnosis and treatment of inferior mesenteric arterial endoleaks after endovascular repair of abdominal aortic aneurysms. Radiology 2000;215(2):409-13. [ Links ]
6. Vaillant M, Barral P-A, Mancini J, et al. Preoperative inferior mesenteric artery embolization is a cost-effective technique that may reduce the rate of aneurysm sac diameter enlargement and reintervention after evar. Ann Vasc Surg 2019;60:85-94. [ Links ]
7. Manunga JM, Cragg A, Garberich R, et al. Preoperative inferior mesenteric artery embolization: A valid method to reduce the rate of type II endoleak after evar? Ann Vasc Surg 2017;39:40-7. [ Links ]
8. Ward TJ, Cohen S, Fischman AM, et al. Preoperative inferior mesenteric artery embolization before endovascular aneurysm repair: Decreased incidence of type II endoleak and aneurysm sac enlargement with 24-month follow-up. J Vasc Int Radiol 2013;24(1):49-55. [ Links ]
9. Samura M, Morikage N, Otsuka R, et al. Endovascular aneurysm repair with inferior mesenteric artery embolization for preventing type II endoleak. Ann Surg 2020;271(2):238-44. [ Links ]
10. Van Marrewijk C, Buth J, Harris PL, et al. Significance of endoleaks after endovascular repair of abdominal aortic aneurysms: The Eurostar Experience. J Vasc Surg 2002;35(3):461-73. [ Links ]
11. Burbelko M, Kalinowski M, Heverhagen JT, et al. Prevention of type II endoleak using the amplatzer vascular plug before Endovascular Aneurysm Repair. Eur J Vasc Endovasc Surg 2014;47(1):28-36. [ Links ]
12. Veith FJ, Baum RA, Ohki T, et al. Nature and significance of endoleaks and endotension: Summary of opinions expressed at an international conference. J Vasc Surg 2002;35(5):1029-35. [ Links ]
13. Nevala T, Biancari F, Manninen H, et al. Inferior mesenteric artery embolization before endovascular repair of an abdominal aortic aneurysm: Effect on type II endoleak and aneurysm shrinkage. J Vasc Intervent Radiol 2010;21(2):181-5. [ Links ]
14. Alerci M, Giamboni A, Wyttenbach R, et al. Endovascular abdominal aneurysm repair and impact of systematic preoperative embolization of collateral arteries: Endoleak analysis and long-term follow-up. J Endovasc Ther 2013;20(5):663-71. [ Links ]
15. Parry DJ, Kessel DO, Robertson I, et al. Type II endoleaks: Predictable, preventable, and sometimes treatable?J Vasc Surg 2002;36(1):105-10. [ Links ]
16. Bonvini R, Alerci M, Antonucci F, et al. Preoperative embolization of collateral side branches: A valid means to reduce type II endoleaks after endovascular AAA repair. J Endovasc Ther 2003;10(2):227-32. [ Links ]
17. Aoki A, Maruta K, Hosaka N, et al. Predictive factor of the possibility for aortic side branches coil embolization during endovascular abdominal aortic aneurysm repair. Ann Vasc Diseases 2020;13(3):240-7. [ Links ]
18. Güntner O, Zeman F, Wohlgemuth WA, et al. Inferior mesenteric arterial type II endoleaks after endovascular repair of abdominal aortic aneurysm: Are they predictable?Radiology 2014;270(3):910-9. [ Links ]
19. Karch LA, Henretta JP, Hodgson KJ, et al. Algorithm for the diagnosis and treatment of endoleaks. Am J Surg 1999;178(3):225-31. [ Links ]
Received: September 08, 2022; Accepted: March 03, 2023











 text in
text in