Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Archivos Españoles de Urología (Ed. impresa)
versión impresa ISSN 0004-0614
Arch. Esp. Urol. vol.59 no.9 nov. 2006
INTERNATIONAL SECTION
Conformal prostate brachytherapy guided by realtime dynamic dose calculations using permanent 125iodine implants: technical description and preliminary experience
Pedro J. Prada1, German Juan1,
José Fernández2, González-Suárez H3,
Álvaro Martínez4, José González5 y
Ana Alonso3
1Department of Brachytherapy, Hospital Sagrado Corazón. Valladolid, Spain
2Department of Radiation Physics, Hospital Central de Asturias. Oviedo, Spain
3Department of Radiation Oncology, Hospital Central de Asturias. Oviedo, Spain
4Department of Radiation Oncology, Willian Beaumont Hospital. Royal Oak, MI, USA
5Department of Urology, Willian Beaumont Hospital. Royal Oak, MI, USA
SUMMARY
Objetive: Low dose rate (LDR) prostate brachytherapy (permanent 125I or 103Pd seeds) is an accepted treatment option for low risk prostate cancer patients. However, differences in prostate spatial location, volume and gland deformation between the images obtained during pre-planning and later on during the implant procedure prevent the pre-planned intended dose to be accurately delivered. We are reporting on a new technique based on interactive real-time dynamic intra-operative dose calculation with avoidance of post-implant CT for final dosimetry. The reasons leading us to implementing this new technique are discussed and preliminary results reported.
Methods: A pre-planning TRUS for volumetric analysis is performed in all our patients prior to implantation. This TRUS accomplishes two objectives: 1) assessment of implantability of the gland, of organs at risk and anatomical considerations and 2) determination of seed activity and total number of seeds. On the day of the implant, new TRUS images from base to apex are obtained using a motorized stepper connected to the ultrasound and planning system. Each real time needle position placed on the target is identified and capture by the planning system in the true position. Once all real needle positions have been captured, dosimetry is performed intra-operatively and the physician approves the corresponding isodoses on real time. Flexible cystoscopy is then performed followed by seed placement. Each seed implanted is then identified upon withdrawing the needle using TRUS guidance. This allows real-time intra-operative dosimetric analysis, allowing for correction of under-dosed zones during implantation in an interactive dynamic manner. Peripheral loading is used.
Results: We began our LDR prostate brachytherapy program on 1999. While we have treated >700 patients with LDR, the last 63 patients were treated with our real time dynamic intra-operative planning system. The median time duration for the procedure was 90 minutes. The median follow up time for these 63 patients was 20 months with a range of 10-36 months. At presentation, Stage T1c was seen in 55%, T2a in 36% and 9% as T2b. The Gleason grade was <7 in 81% of the patients. The median PSA value was 9 ng/ml (range 4.2-30). The median age was 64 years (range 47-78 years). For the real time intra-operative dosimetric analysis the following values were obtained: a median of 98% (90%-100%) for V90, of 60% (22%-76%) for V150 and 24% (9%-34%) for V200. The median intra- operative D90 obtained was 16,817 cGy with a range of 13,743 to 19,553 cGy. The median dose point calculation to the rectum maximum was 12,936 cGy and for the maximum in urethra was 21,880 cGy. For the real-time dynamic planning, the acute GU grade 1&2 toxicity was reduced from 28% and 21% to 16% and 6% respectively. Acute urinary retention was seen in 2/63 or 3% requiring a temporary post-implant bladder catheter. In addition, a decrease in chronic GU grade 1-2 toxicity was also seen from16% and 17% to 11% and 2% respectively. No change in GI toxicity pattern was noted. No severe grade 3-4 intra-operative complications were noted.
Conclusión: Real-time intra-operative planning was successfully implemented in our center. It avoids the possible implant quality and dose delivery disadvantages of the standard post-implant CT-based dosimetry by improving the accuracy of seed placement on real time, which was translated in lower rates of acute and chronic GU morbidity. In addition, avoids the unnecessary time, effort and cost of post-implant CT-based dosimetry.
Keywords: Prostate cancer, Brachytherapy, Dynamic dose calculation, Real-time.
RESUMEN
Objetivo: El tratamiento con braquiterapia de baja tasa de dosis (LDR) con implantes permanentes de 125-I o 103Pb, constituyen en la actualidad una opción terapéutica en los pacientes con cáncer de próstata de bajo riesgo. La variación observada en el posicionamiento espacial de la próstata, así como en el volumen y contorno prostático entre las imágenes obtenidas durante la planificación y posteriormente durante la intervención, hacen dudar de la exactitud de dosificación, en los pacientes tratados con la técnica de preplanificación. Analizamos la técnica basada en la planificación previa, la planificación intraoperatoria interactiva, así como nuestro proceder actual de planificación intraoperatoria por cálculo dinámico en tiempo real y los motivos que nos llevaron a realizar este cambio de técnica.
Métodos: Con el cálculo del volumen prostático preoperatorio por ecografía transrectal, determinamos la posibilidad de realizar el implante en base a las consideraciones anatómicas existentes y decidimos la actividad por semilla y la actividad total del implante. El día de la intervención comprobamos de nuevo la volumetría, obtenemos de nuevo las imágenes ecográficas de base a apex, ayudados por un stepper motorizado que va conectado con el ecógrafo y el planificador. Cada aguja que se coloca en la posición que deseamos y no en una coordenada obligada, se identifica en el planificador en la posición real, una vez colocadas todas las agujas y obtenidas unas primeras isodosis adecuadas, realizamos una cistoscopia flexible y a continuación sembramos, identificando todas y cada una de las semillas en la retirada de la aguja guía ecográficamente, con lo que nos permite obtener una postplanificación intraoperatoria en tiempo real y hacer las correcciones oportunas en el propio acto quirúrgico. Realizamos un implante periférico puro.
Resultados: Iniciamos los tratamientos con braquiterapia de baja tasa de dosis en 1.999. Superadas las 700 intervenciones, hemos evaluado a los primeros 63 pacientes tratados con la técnica de cálculo dinámico de dosis en tiempo real por presentar un seguimiento mínimo de 10 meses. El tiempo medio del proceso fue de 90 minutos. La media de seguimiento para los 63 pacientes estudiados fue 20 meses con un rango entre 10 y 36 meses. Un 55% de los pacientes fueron estadiados como T1c, 36% T2a y 9% T2b. En el 81% de los pacientes el Gleason fue < 7. La media de PSA al inicio de tratamiento fue de 9ng/ml (4.2-30 ng/ml). La media de edad fue de 64 años (47-79 años). La técnica de braquiterapia por cálculo dinámico de dosis en tiempo real obtuvo los valores que se especifican a continuación: media 98% (90%-100%) para V90, V150 de 60% (22%-76%), V200 de 24% (9%-34%). La D90 media fue de 16.817 cGy (13.743-19.553 cGy). La dosis media máxima a nivel rectal fue de 12.936 cGy y a nivel uretral de 19.553 cGy. Con la técnica de cálculo dinámico de dosis en tiempo real, la toxicidad aguda genitourinaria de grado 1-2 fue reducida del 28% y 21% respectivamente a 21% y 16%. El porcentaje de retenciones fue del 3% y la toxicidad urológica crónica fue reducida del 16% y 17% al 11% y 2% respectivamente. No se observaron cambios gastrointestinales de grado 3-4.
Conclusiones: La técnica de cálculo dinámico de dosis en tiempo real es utilizada de forma habitual con éxito en nuestro centro. Evita las desventajas que presentan otras técnicas, mejorando la cobertura de la próstata por las dosis ideales de irradiación que se traducirán en un mejor control local de la enfermedad y una disminución de las complicaciones así como evitar la realización de la postplanificación postoperatoria.
Palabras clave: Cáncer de próstata. Braquiterapia. Cálculo de dosis dinámico. Tiempo real.
Introduction
Prostate cancer brachytherapy has rapidly gained popularity in the USA (1,2), in Europe (3,4) including Spain [5] as an accepted, effective and safe therapy for localized prostate cancer. A number of techniques have been developed to perform low dose rate permanent seeds interstitial brachytherapy. However, uniform terminology to describe the different methods is somehow lacking. Any description should therefore adhere to a concrete nomenclature for clarity. In this context, we have adopted the American Brachytherapy Society proposal for describing the different planning processes (6):
Preplanning. A treatment plan is developed several days or weeks before the implantation.
Intra-operative planning. The treatment plan is defined within the operating room, followed by seed implantation. Three types of intra-operative planning have been defined:
1. Intra-operative preplanning: Definition of a plan within the operating room immediately before implantation, and involving immediate execution of the plan.
2. Interactive planning: The procedure is the same as before, with the addition of an isodose calculation derived from identification of the needles in the prostate gland.
3. Real-time dynamic dose calculation: Dose calculation is carried out based on identification of the seeds after placement in the prostate. In 1999 we performed our first interstitial implant procedure with 125I seeds (RAPID-strand®), following the classical preplanning technique described by the Seattle group (7-9). Our initial experience using the Seattle approach has been previously described (5).
We have noted a series of limitations when using the standard above mentioned preplanning with CT-based dosimetry technique:
From the needle placement point of view, there are changes in prostate gland volume, gland deformation and spatial location between the images obtained at preplanning and those TRUS images during the actual surgical procedure. In addition, there are uncertainties related to differences in patients positioning for the test and the implant procedure as well as pelvic muscle relaxation induced by the spinal anesthesia. Another source of pre-planning dosimetric quality degradation is the intra-operative swelling related to the needle trauma in it self. Occasionally pubic arch interference requires either immediate change of needle coordinates and or changing patients positioning. All these problems introduce many uncertainties between dose planned and dose delivered from using a pre-planning strategy.
Post-implant dosimetry and implant evaluation with CT poses a series of difficulties due to poor delineation of the prostatic contour as well as accurate identification of the base and apex of the gland. The ideal timing of CT-based dosimetry compounds these significant uncertainties. In addition, this process does not allowed for either real time dosimetry assessment or for intra-operative correction of these uncertainties.
The purpose of the present study is to contrast the classical preplanning technique, the intra-operative planning with or without interactive planning (10) with our real-time dynamic calculations technique. Also, to describe our present protocol based on intra-operative planning with real-time dynamic dose calculation reporting our preliminary results obtained in 63 patients so treated. Few institutions have already made reference to intra-operative planning as a better technical approach (11, 12).
Material and Methods
Considering that the preplanning technique, the implantation procedure and post-implant CT based evaluation, including ours, is well documented in the literature (6-9), we are not describing the process.
LDR Intra-operative planning Technique.
Both intra-operative preplanning and interactive planning eliminate the patient visit for preplanning, since the procedure in question is carried out in the actual operating room. The approximate number of seeds is defined from nomograms or tables based on the prostate volume (usually determined by trans-rectal ultrasound).
Image capture by TRUS is performed during the intervention. The target, rectum and urethra are contoured, and the ideal needle position within the volume to be implanted is defined and depicted by the TRUS monitor. Implantation is then carried out accordingly.
The intra-operative planning technique solves the problems of changes in spatial prostate location, but cant correct for changes related to needle placement such as organ distortion, deformation and spatial dislocation. Occasional difficulty placing the needles due to pubic arch interference remains a problem. However, since the seeds are not identified during the implant procedure, intra-operative corrections cant be executed. As a result, post-implant dosimetry and implant evaluation by CT must be performed with the above-mentioned consequences and drawbacks. The implantation technique referred to as intra-operative planning with real-time dynamic dose calculation avoids all these problems. We have therefore developed this approach and have used it in all our LDR prostate implantation procedures. Our technique is described below.
Technique
On of the first visit we perform a trans-rectal ultrasound to assess anatomical implantability, and to determine prostate gland volume, calculated by the software (volume of an ellipsoid).
Based on the information obtained, we can then determine:
Total implant activity, based on the nomogram published by Wu et al. (13), as a function of prostate gland volume.
Activity per seed to be used, based on our own experience (see Table I).
Of the total number of seeds, 75-80% is positioned within the periphery of the prostate, since our aim is to perform peripheral loaded implantation.
On the day of the intervention we proceed as follows:
1. Patient positioning:
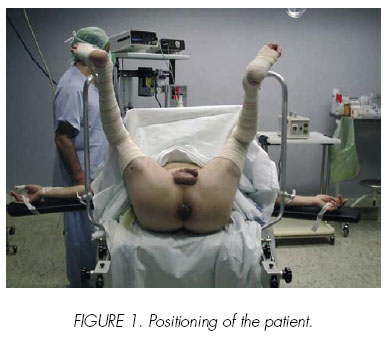
Patient positioning, in the pelvic flex position and image acquisition are depicted on Figure 1.
2. Intra-operative planning:
Prostatic volumetric analysis is performed. Ultrasound images are obtained every 0.5 cm from base to apex. The TRUS images are then transferred to the planning system using a motorized stepper with direct connection between the ultrasound unit, stepper and planning system. The images are processed with the planner, and the contours of prostate, urethra and rectum are obtained in each of the sections.
Needle positioning starts at the place we consider most adequate, not at a given coordinate. A needle is positioned and then identified by TRUS in its true position – since the image obtained is real-time. This same procedure is then repeated with all the needles, thus yielding a first series of isodoses with the corresponding volumes. If the established dosimetric criteria are satisfied (Figure 1) (14), we continue with flexible cystoscopy to confirm that none of the needles have invaded the urethra or bladder.
3. Implantation:
Once all the guiding needles are in the positions considered ideal (Figure 3), each is loaded with the corresponding number of seeds, and during needle withdrawal we identify all the deposited seeds via ultrasound in a longitudinal acquisition – as a result of which the isodoses are generated according to the true positioning of the seeds (Figure 4). This procedure is repeated with each needle, thus yielding the true isodose distribution.
In the event of discovering under-dosed zones, corrective measures are implemented during the surgical procedure. Overdosed zones can be avoided by examining how the isodoses evolve as implantation proceeds. The total duration of the procedure is approximately 90 minutes.
Intra-operative planning requires a trained, coordinated and experienced team in order to avoid prolongation of the surgical intervention and seed placement uncertainties capable of precluding ideal coverage by the reference isodose. Post-implant CT, for dosimetric evaluation, after implantation is avoided, since implant dosimetry and evaluation is done in real time during the implant procedure.
Results
We began our LDR prostate brachytherapy program on 1999. Based on the difficulties previously mentioned, in May 2003 we began our new intra-operative planning implantation technique described in this paper. While we have treated >700 patients with LDR, the last 63 patients who had a minium follow- up of 10 months were treated with our real time dynamic intra-operative planning system. The median follow up time for these 63 patients was 20 months with a range of 10-36 months.
Patients Characteristics:
In our patient population, more than half of the patients, 55% presented as Stage T1c, 36% as a T2a, and 9% as T2b prostate cancer. The Gleason grade was <7 in 81% of the patients and 7 in the remaining 17%. The median PSA was 9 ng/ml with a range of 4.2-30 ng/ml. The median prostate volume implanted was 38cc (16-69cc). The median age was 64 with a range of 47-78 years.
Dosimetric analysis:
For the real time intra-operative dosimetric analysis, we obtained a median of 98% (90%-100%) for V90, of 60% (22%-76%) for V150 and 24% (9%-34%) for V200. The median intra-operative D90 obtained was 16,817 cGy with a range of 13,743 to 19,553 cGy. The median dose point calculation to the rectum maximum was 12,936 cGy and the median for the maximum in urethra of 21,880 cGy.
Acute and Chronic Toxicity:
All 63 patients were discharge from the center the same day of the procedure between 6-8 hours of implantation. All patients have been seen in follow up. The RTOG toxicity criteria were utilized to score acute and late complications. Using this glossary, a toxicity comparison was performed between those patients treated with standard pre and post-implant CT planning with those treated with our real-time dynamic planning. For the real-time dynamic planning, the acute GU grade 1&2 toxicity was reduced from 28% and 21% to 16% and 6% respectively. Acute urinary retention was seen in 2/63 or 3% requiring a temporary post-implant bladder catheter. In addition, a decrease in chronic GU grade 1-2 toxicity was also seen from16% and 17% to 11% and 2% respectively. No change in GI toxicity pattern by planning technique was noted. RTOG-rectal complications consisted in acute proctitis of 8% and 2% for chronic. No severe grade 3-4 intra-operative complications were noted. However one patient treated with the standard technique developed a rectal ulcer (Table II, III).
Most patients with grade 2 urinary symptoms were treated -blockers and/or anti-inflammatory medications of the non-steroidal types. At this moment the follow-up is short to evaluate the impact on sexual function.
Discussion
Transperineal ultrasound guided interstitial LDR 125I implant is considered a treatment option for selected prostate cancer patients with presume disease confined to the gland. The technique affords local control and survival outcomes similar to those obtained with radical prostatectomy, with fewer complications.
Permanent seed implantation with 125I is usually performed based on the preplanning technique (6-9). However the preplanning technique poses a series of limitations stated in the introduction with the consequence of degrading the optimized pre-planned dosimetry leading to significant inaccuracies, potential errors and modification of the intended prescribed dose. On the other hand, the initial TRUS is used to order the expected number of seeds implanted. Certainly, post-implant CT planning is necessary 4-6 weeks after implantation, to examine the definitive disposition of the seeds and the definitive isodoses. In the event of finding either over or under-dosed zones, corrections seldom can be performed adding complexity to dose delivery.
All permanent seeds techniques including intra-operative planning require determination of prostate gland volume, since this parameter serves to calculate total implant activity based on the volume/ activity encompassing tables developed by Wu et al. (13). These authors used a mathematical model assuming a peripheral load and a sphero-cylindrical shape of the implanted volume. In an analysis of 40 patients, they observed good prostate coverage with the 145 cGy isodose (V100), with good coverage of 90% of the prostate gland. Knowledge of the prostate volume can also inform us of the activity per implanted seed (Table I). We have adopted this correlation after performing over 200 125I seed implants, with the observation that it allows peripheral implantation in compliance with the symmetrical parameters specified by the American Brachytherapy Society (14), and with the premise of placing over 1.5 seeds per millimeter volume.
With the intra-operative planning technique it is advisable to place 5-10% more seeds, due to possible changes in prostate volume, which can be seen in the real time TRUS, secondary to pelvic muscle relaxation induced by spinal anesthesia and swelling due to trauma.
In 1991 William Beaumont Hospital pioneered real time dynamic intra-operative dose calculations using HDR prostate brachytherapy for locally advanced prostate cancer (15-17). In 1995 they expanded the real time dosimetry planning to include HDR monotherapy for patients with favorable disease (18). Following the WBH intra-operative dosimetry concept, we developed our own in-house project for LDR brachytherapy. It will allow us to make a first dose calculation and quick evaluation of gland coverage intra-operatively with the first attempt to needle position selection by the computer. Changes in virtual needle positions can be executed in the computer to improve implant quality. This allows us to further adjust needle positioning in the central and posterior prostate regions, thus improving the coverage dose delivered to the prostate gland and tissues at risk (such as the urethra and rectum).
The concept of performing the entire LDR procedure in a single intervention with intra-operative planning has already been advocated by a couple of authors. Gewanter et al. (19) reported improvement in administration of the prescribed dose, with significant improvement of D100 (dose covering 100% of the prostate volume) and V100 (prostate volume bathed by the 100% isodose). Wilkinson et al. (20) likewise observed improvement in relation to parameters such as V80, V90, V100, V150, and D90, when they compared the cases treated with pre-planning to intra-operative planning. Similar findings were reported by Polo et al. (21).
With the technique we are reporting, the guiding needles are all implanted as captured by TRUS before loading. In this way we observe less mobility and increased accuracy when placing the posterior seeds, compared with one-by-one insertion and individual loading of the needles. Moreover, with all needles in the appropriate spatial distribution we can perform a flexible cystoscopy and assess the possibility of needle penetration into the urethra or bladder. Any such needles can be repositioned, before seed placement.
Using the Variseed 7.1 (Varian) planning system to identify the seeds as they are deposited in the prostate gland, we can monitor the true dose coverage in real time. Following placement and identification of each seed, we can intra-operatively determine the true gland coverage and corresponding dose distribution. Thus allowing us to implant additional seeds in underdosed areas and overcome a problem that is otherwise difficult to solve when final dosimetry and planning are performed 4-6 weeks after the procedure. Stone and Stock (22-25) also indicated that intra-operative dosimetry offers a good representation of the dose administered. Implantation modifications are thus made possible in real time during a single stage process.
One of the problems that may arise is the difficulty of identifying the 125I seeds by ultrasound at the time of implantation in the prostate. However, this problem is minimized when using the motorized stepper (Acuseed) connected to the Variseed 7.1 (Varian) planner, which allows the identification of guidance needles in sagittal and longitudinal acquisitions, This is facilitated by using stranded seeds (RAPID strand) format offering increased rigidity. This TRUS based software for seed identification after seed placement allow us to assess final gland coverage and isodoses intra-operatively.
The drawback of our technique requires a trained and coordinated operating team, with additional performance pressure by the need that the implant procedure must be completed in less than 120 minutes.
This technique is currently endorsed by the American Brachytherapy Society (14) because of the one stage process increasing dose delivery accuracy and decreasing utilization of resources such as additional CT, Physicians and Physicists time.
Conclusions
Intra-operative planning with real-time dynamic dose calculation represents the latest step in the management of prostate cancer with permanent LDR implants. It avoids the disadvantages of the other LDR techniques such as classical preplanning, intra-operative preplanning and intra-operative interactive planning all requiring the additional cost of a CT and additional personnel time doing the final planning. Our results demonstrated clinically a decrease in acute and chronic GU toxicity with our real-time dynamic intra-operative planning.
References and recomended readings (*of special interest, **of outstanding interest)
1. METTLIN, C.J.; MURPHY, G.P.; McDONALD, C.J. y cols.: The National cancer data base report on increase use of brachytherapy for the treatment of patients with prostate carcinoma in the USA. Cancer, 86: 1877, 1999. [ Links ]
2. LEE, R.W.; MOUGHAN, J.; OWEN, J. y cols.: The 1999 Patterns of care Study of radiotherapy in localized prostatic carcinoma. A comprehensive survey of prostate brachytherapy in the United States. Cancer, 98: 1987, 2003. [ Links ]
3. ASH, D.; FLYNN, A.; BATTERMANN, J.; REIJKE, T. y cols.: ESTRO/EAU/EORTC recomendations on permanent seed implantation for localizad prostate cancer. Radiotherapy and Oncology, 57: 315, 2000. [ Links ]
4. BATTERMANN, J.J.; BOON, T.A.; MOERLAND, A.: Results of permanent prostate brachytherapy, 13 years of experience at a single institution. Radiotherapy and Oncology, 71: 23, 2004. [ Links ]
5. PRADA, P.J.; JUAN, G.; HEVIA, M. y cols.: Tecnica de planificacion intraoperatoria en braquiterapia prostatica con implantes permanentes de 125I o 103Pd. Arch. Esp. Urol., 55: 1217, 2002. [ Links ]
6. SUBIR, N.; LAY, P.; CIEZKI, R. y cols.: Intraoperative planning and evaluation of permanent prostate brachytherapy: Report of the American Brachytherapy Society. Int. J. Radiat. Oncol. Biol. Phys., 51: 1422, 2001. [ Links ]
7. RAGDE, H.; BLASKO, J.C.; SCHUMACHER, D. y cols.: Use of transrectal ultrasound in transperineal Iodine-125 seeding for prostate cancer: methodology. J. Endourol., 3: 209, 1989. [ Links ]
8. GRIMM, P.D.; BLASKO, J.C.; RAGDE, H.: Ultrasound-guided transperineal implantation of Iodine-125 and Palladium-103 for the treatment of early stage prostate cancer-technical concepts in planning, operative technique, and evaluation. Atlas Ural. Clin. N. Am., 2: 113, 1994. [ Links ]
9. BLASKO, J.C.; RAGDE, H.; SCHUMACHER, D.: Transperineal percutaneous Iodine-125 implantation for prostatic carcinoma using transrectal ultrasound and template guidance. Endocuerietherapy Hyperthermia Oncology, 3: 131, 1987. [ Links ]
10. CORMACK, R.A.; TEMPANY, C.M.; DAMICO, A.V.: Optimizing target - coverage by dosimetric feedback during prostate brachytherapy. Int. J. Radiat. Oncol. Biol. Phys., 48: 1245, 2000. [ Links ]
11. DOGGETT, S.: Image registered real-time intraoperative treatment planning: Permanent seed brachytherapy. Radlother. Oncol., 55: 4, 2000. [ Links ]
12. ZELEFSKY, M.J.; YAMADA, J.; COHEN, G. y cols.: Postimplantation dosimetric analysis of permanent transperineal prostate implantation: Improved dose distributions with an intraoperative computer optimized conformal planning technique. Int. J. Radiat. Oncol. Biol. Phys., 48: 601, 2000. [ Links ]
13. WU, A.; LEE, C.C.; JOHNSON, M. y cols.: A new power law for determination of total 125I seed activity for ultrasound-guided prostate implants:clinical evaluations. Int. J. Radiat. Oncol. Biol. Phys., 47: 1397, 2000. [ Links ]
14. NAG, S.; BICE, W.; DE WYNGAERT, K. y cols.: The American Brachytherapy Society recommendations for permanent prostate brachytherapy post-implant dosimetric analysis. Int. J. Radiat. Oncol. Biol. Phys., 46: 221, 2000. [ Links ]
15. EDMUNDSON, G.K.; YAN, D.; MARTINEZ, A.A.: Intraoperative optimization of needle placement and dwell times for conformal prostate brachytherapy. Int. J. Radiat. Oncol. Biol. Phys., 33: 1257, 1995. [ Links ]
16. STROMBERG, J.; MARTINEZ, A.; GONZÁLEZ, J. y cols.: Ultrasound-guided high dose rate conformal brachytherapy boost in prostate cancer: Treatment description and preliminary results of a phase I/II clinical trial. Int. J. Radiat. Oncol. Biol. Phys., 33: 161, 1995. [ Links ]
17. KOVACS, G.; GALALAE, R.; WIRTH, B. y cols.: Optimization of interstitial brachytherapy for locally advanced prostate cancer by a new implantation technique. Strahlenther Onco., 171: 685, 1995. [ Links ]
18. MARTINEZ, A.; PATAKI, I.; EDMUNDSON, G. y cols.: Phase II prospecive study of the use of conformal high dose rate brachytherapy as monotherapy for the treatment of favorable stage prostate cancer. Int. J. Radiat. Oncol. Biol. Phys., 49: 61, 2001. [ Links ]
19. GEWANTER, R.M.; WUU, C.S.; LAGUNA, J.L. y cols.: Intraoperative preplanning for transperineal ultrasound-guided permanent prostate brachytherapy. Int. J. Radiat. Oncol. Biol. Phys., 48: 377, 2000. [ Links ]
20. WILKINSON, A.; LEE, E.J.; CIEZKI, J.P. y cols.: Dosimetric comparison of pre-planned and or-planned prostate seed brachytherapy. Int. J. Radiat. Oncol. Biol. Phys., 48: 1241, 2000. [ Links ]
21. POLO, A.; MARSIGLIA, M.; VAVASSORI, A. y cols.: Dosimetria postimplante usando fusion de imagenes en braquiterapia prostatica con implantes permanentes. Rev. Oncologia, 3: 97, 2001. [ Links ]
22. STONE, N.N.; RAMIN, S.A.; WESSON, M.F. y cols.: Laparoscopic pelvic Iymph node dissection combined with real-time interactive transrectal ultrasound guided transperineal radioactive seed implantation of the prostate. J. UroI., 153: 1555, 1995. [ Links ]
23. STOCK, R.G.; STONE, N.N.; LO, T.C.: Intraoperative dosimetric representation of the real-time ultrasound-guided prostate in plant. Tech. Urol., 6: 95, 2000. [ Links ]
24. STONE, N.N.; STOCK, R.G.: Prostate Brachytherapy: Treatment Strategies. J. Urol., 162: 421, 1999. [ Links ]
25. STONE, N.N.; STOCK, R.G.: Prostate Brachytherapy in patients with prostate volumen > 50 cm3. Dosimetric analysis of implant quality. Int. J. Radiat. Oncol. Biol. Phys., 46: 1199, 2000. [ Links ]
![]() Correspondence to:
Correspondence to:
Dr. Pedro J Prada, MD,
Department of Radiation Oncology
Hospital Central de Asturias
C/ Julian Claveria s/n
E-Oviedo 33006 Asturias. (Spain)
E-mail: pprada@telecable.es
Acepted for publication:19.07.06.