My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.61 n.2 Mar. 2008
MONOGRÁFICO: REFLUJO VESICOURETERAL
Laparoscopic anti-reflux plasty: experience of the university of São Paulo
Plastia antirreflujo laparoscópica: experiencia de la universidad de Sao Paulo
Francisco T. Dénes, Anuar I. Mitre, Marco A. Arap1, Ricardo J. Duarte1, José L. Chambo1, Artur H. Brito1 and Miguel Srougi2.
Associate Professor of Urology. Assistant Professor of Urology1. Professor and Chairman of Urology2. School of Medicine. University of São Paulo. São Paulo. Brazil.
Dirección para correspondencia
SUMMARY
Objectives: Vesico-ureteric reflux (VUR) is a common cause of urinary tract infections in children, being less commonly diagnosed in adults. Several anti-reflux plasties have been used successfully for the treatment of such condition, such as Politano-Leadbetter, Cohen and Gregoir-Lich techniques, the latter being our preferred approach in open procedures. Here we describe our experience with laparoscopic Gregoir-Lich anti-reflux plasty (LGLP) in children and adults.
Methods: The LGLP was used for the treatment of VUR in 15 patients (7 adults and 8 children). Four adults and 5 children had bilateral disease and both sides were treated at the same procedure. Data was collected prospectively and we analysed age at treatment, laterality, degree of VUR, previous anti-reflux procedures, operative time, number of detrusor stitches used in each side, intra-operative and post-operative complications, success rate and follow-up.
Results: A total of 23 ureteral units were treated. VUR was graded as I in one unit, II in 4 units, III in 10 units, IV in 7 units and 1 unit was not classified, as it was diagnosed by radioisotopic cystography. Two children had failed previous endoscopic procedures. There were no open conversions. Two muccosal perforations occurred during the procedure and were successfully treated laparoscopically. Nineteen out of 21 ureteral units (90%) presented no VUR at the cystographic control, and no bladder dysfunction was identified on follow-up.
Conclusions: The LGLP is a feasible, minimally invasive alternative for VUR that reproduces the open procedure. It has an excelent success rate and is not associated to bladder disfunction, even in bilateral procedures.
Key words: Vesico-ureteric reflux. Laparoscopy. Gregoir-Lich. Treatment.
RESUMEN
Objetivo: El reflujo vesicoureteral (RVU) es una causa común de infecciones del tracto urinario en niños, siendo diagnosticado con menos frecuencia en adultos. Se han utilizado varias técnicas antirreflujo para el tratamiento de dicha condición, como las técnicas de Politano-Leadbet-ter, Cohen y Gregoir-Lich, siendo ésta última nuestro abordaje preferido en cirugía abierta. Describimos nuestra experiencia con la plastia antirreflujo laparoscópica de Gregoir-Lich en niños y adultos.
Métodos: La plastia de Gregoir-Lich laparoscópica fue utilizada en el tratamiento del RVU en 15 pacientes (7 adultos y 8 niños). Cuatro adultos y cinco niños respectivamente tenían reflujo bilateral, tratándose ambos lados en el mismo acto quirúrgico. Los datos fueron recogidos prospectivamente y se analizó edad en el momento el tratamiento, lado, grado de RVU, operaciones antirreflujo previas, tiempo operatorio, número de puntos del detrusor utilizados en cada lado, complicaciones intra y postoperatorias, tasa de éxitos y seguimiento.
Resultados: Se trataron un total de 23 unidades ureterales. El RVU fue grado I en 1 uréter, II en 4, III en 10 y IV en 7, en un uréter no se asignó grado porque se diagnosticó mediante cistografía radioisotópica. Dos niños habían tenido operaciones endoscópicas previas que fracasaron. No hubo ninguna conversión a cirugía abierta. Hubo dos casos de perforación mucosa durante el procedimiento que fueron tratadas con éxito por vía laparoscópica. Diecinueve de las 21 unidades ureterales (90%) no presentaban RVU en el control mediante cistografía, y no se identificó disfunción vesical en el seguimiento.
Conclusiones: La plastia laparoscópica de Gregoir-Lich es una alternativa factible, mínimamente invasiva para el RVU que reproduce el procedimiento abierto. Tiene un excelente porcentaje de éxitos y no se asocia con disfunción vesical, cruzó en procedimientos bilaterales.
Palabras clave: Reflujo vesicoureteral. Laparoscopia. Gregoir-Lich. Tratamiento.
Introducción
Vesico-ureteric reflux (VUR) is one of the most common problems in pediatric urology, being found in up to 70% of infants with urinary tract infections (UTI) (1). It is less commonly diagnosed in adults, in whom it usually leads to symptoms such as UTI and lumbar pain.
Different successful open anti-reflux techniques have been described, such as Leadbetter-Politano (2), Cohen (3) and Gregoir-Lich (4, 5), all presenting success rates of more than 85% on the long-term follow-up (6-11).
As in many other urologic procedures, minimally invasive techniques have also been described for the treatment of VUR. Cystoscopic injection of bulking agents has been introduced, with long-term success depending on the grade of reflux, experience of the surgeon, number of procedures in each patient and the type of bulking agent used (12-14). Presently it is considered a good first line of treatment, but is associated with significant long-term failure rates, particularly in high grade VUR (15, 16).
The first successful laparoscopic correction of reflux in animals was described by Atala in 1993 (17), who employed a laparoscopic modification of the Gregoir-Lich extravesical technique. Since then, several other laparoscopic techniques have been described as successful reproductions of open surgeries (18-20). The LGLP is a feasible alternative for treatment of patients with VUR, as it is an extravesical technique and does not require the ureteral disinsertion. Here we describe our experience with LGLP anti-reflux procedure in 8 children and 7 adults with VUR.
Methods
This study was approved by the institutional ethics committee. From December 2003 to February 2007, 15 patients underwent LGLP for the treatment of symptomatic VUR at our institution (7 adults and 8 children under the age of 9 years). Four adults and 6 children had bilateral VUR. Of this group, all adults and four children had both ureters treated in the same procedure, while two children were submitted to unilateral procedure associated to contralateral nephroureterectomy due to the presence of pyelonephritic kidneys with less than 12% function. Therefore, a total of 23 ureteral units submitted to LGLP were included in the study. Of the 15 patients, 12 (80%) were operated due to breakthrough UTI, 2 adults due to incapacitating lumbar pain unrelated to UTI and 1 child due to an asymptomatic grade IV reflux to both units of a complete duplex system that was diagnosed after the incision of a contralateral ureterocele.
Data was prospectively collected and the following parameters were evaluated: patient age at the time of the procedure, laterality and grade of VUR, previous anti-reflux procedures, operative time, number of detrusorrhaphy stitches applied in each side, intra-operative and post-operative complications and success rates. All patients but one were evaluated preoperatively with voiding cystourethrography and the VUR was graded according to the International Reflux Study (21). One patient was diagnosed with a radioisotopic cystography, and was not classified according to the grade of reflux.
The LGLP was performed by the same technique in children and adults. Briefly, while under general anesthesia, patients were placed in the supine position, and the abdomen and genitals were prepared and draped in sterile fashion, so that the bladders could be filled and emptied by the surgeon during the procedure. The first 5 or 10 mm trocar was placed below the umbilicus after transperitoneal CO2 insufflation through a Verres needle, and two or three trocars (3 or 5 mm) were positioned depending on the side of reflux and bilaterality.
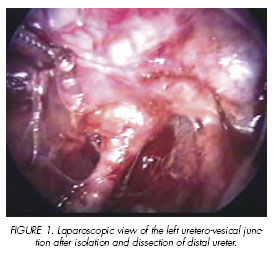
The pelvic cavity was inspected and, after incision of the peritoneum, the refluxing ureter was isolated 3-4 cm proximal to the bladder, and tractioned superiorly to indicate the direction and length of the detrusor incision (Figure 1). With the bladder partially filled with saline, a 2-3cm detrusor incision was done with the laparoscopic scissors, exposing the vesical mucosa (Figure 2). At this point hemostasis of the detrusor was performed with the monopolar cautery. In the cases were the bladder mucosa was accidentally opened, the bladder was emptied and the mucosal laceration was immediately sutured with a running 5-0 absorbable suture. The ureter was then placed over the mucosa and the detrusor was approximated above the ureter with separate 3-0 or 4-0 polyglactin sutures (Figure 3). The new ureteral hiatus was evaluated for ureteral obstruction or angulation with a right angle forceps (Figure 4). In cases of mucosal laceration, a Penrose drain was inserted through one of the ports and left one or two days. In unilateral procedures, the Foley catheter was kept indwelling for three, while in bilateral LGLP it remained for four days.
All patients were evaluated during follow-up with blood urea nitrogen and creatinine measurements, urine culture and renal ultrasound. A control voiding cystourethrography was performed two to three months after surgery, except for one patient who was submitted to a radioisotopic cystography after five months, as it was the test that initially diagnosed VUR. Statistical analysis was performed with SPSS® 12.0 for Windows and numerical variables were described as median, minimum and maximum values. For the qualitative variables, data was presented numerically and in percentile.
Results
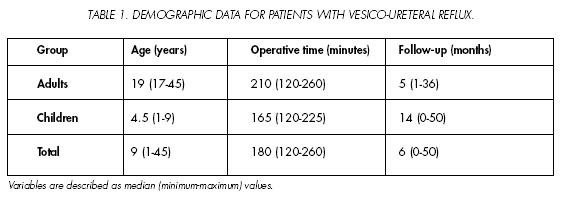
Table I shows data for the 15 patients. A grade I VUR was present in one (4.5%) unit, grade II in 4 units (17.5%), grade III in 10 units (43.5%) and grade IV in 7 units (30%). One patient with unilateral reflux was diagnosed by radioisotopic cystography and therefore was not classified. One child with bilateral VUR was previously submitted to a bilateral endoscopic submmucosal injection of Deflux® and another child with unilateral VUR was previously submitted to 2 endoscopic injections of bulking agents (Deflux® and Durasphere®). Median age was 4.5 (1-9) years for the children, 19 (17-45) years for the adults, and 9 (1-45) years for all patients. Median operative time was 165 (120-225) for the children, 210 (120-260) for the adults and 180 (120-260) for all patients.
Three detrusor stitches were used in 21 ureters (91%) and 4 stitches in 2 ureters (9%). No conversions to open procedures were necessary. Two muccosal perforations occurred (one adult and one child) and both were immediately diagnosed and successfully corrected. There were no other intraoperative or postoperative complications.
Of the 23 units treated, 21 were evaluated postoperatively as one adult patient with bilateral VUR recently operated refused to undergo post-operative control. Of the 21 ureteral units evaluated, none presented any pyelo-ureteral dilatation on the control US examination. Furthermore, 19 (90%) presented no VUR at the first postoperative control and all patients are asymptomatic, without UTI or vesical dysfunction. The patient with the duplex ureteral unit presented an asymptomatic grade II VUR to the inferior unit and no VUR to the superior moeity. She was maintained on antibiotic prophylaxis for 4 months and is now asymptomatic 13 months after surgery. Another adult female presented with residual grade II VUR in the postoperative control and had a symptomatic UTI. She was maintained on antibiotic prophylaxis and will be submitted to another anti-reflux plasty.
Discussion
As seen in other laparoscopic Gregoir-Lich series, our success rates are well over desirable limits. In addition, it reproduces the success rates obtained for open series (11). Although we had only 8 patients with bilateral VUR, no bladder dysfunction was seen. This complication, feared in bilateral open procedures and believed to be the consequence of an extensive bilateral bladder dissection, was probably avoided due to very limited vesical and distal ureteral dissection.
One important aspect of the surgery in adults, which explains the longer operative time for this group, is the difficulty in accessing the ureter near the bladder. To overcome this difficulty, we started after the first few procedures to open a window in the peritoneum close to the iliac vessels in order to find the ureter and repair it with a penrose drain. This allowed us to mobilize the ureter, facilitating its identification near the bladder. In most children, the distal ureters are easily identified by transparency in the retroperitoneum, due to paucity of fatty tissue.
The only complication observed was muccosal perforation, which was easily diagnosed in both child and adult, as the bladder was maintained partially full for the facilitation of ureteral dissection. It was also easily corrected with a running 5-0 absorbable suture and the maintenance of a bladder catheter 4 days after the procedure. This was the rule for all patients with bilateral procedures, whereas those submitted to unilateral LGLP were maintained with the catheter for 3 days. Other complications such as postoperative urinary infections were prevented with antibiotic prophylaxis, which was maintained until the first normal radiological control was obtained.
In our hands, LGLP was a safe and effective treatment for patients with VUR, regardless of previous endoscopic procedures. To our knowledge, this is the largest series of laparoscopic Gregoir-Lich procedure in children and adults.
References and recomended readings (*of special interest, **of outstanding interest)
1. WALKER, R.D.; DUCKETT, J.W.; BARTONE, F.F. y cols.: Screening schoolchildren for urologic disease. Birth. Defects Orig. Artic. Ser., 13: 399, 1977. [ Links ]
2. POLITANO, V.A.; LEADBETTER, W.F.: An operative technique for the correction of vesicoureteral reflux. J. Urol., 79: 932, 1958. [ Links ]
3. COHEN, S.H.: Ureterozystoneostomie. Eine neue Antirefluxtechnik. Aktuel Urol., 6, 1975. [ Links ]
4. GREGOIR, W.; VANREGEMORTER, G.: Congenital Vesico-Ureteral Reflux. Urol. Int., 18: 122, 1964. [ Links ]
5. LICH, R. Jr.; HOWERTON, L.W. Jr.; GOODE, L.S. y cols.: The Ureterovesical Junction of the Newborn. J. Urol., 92: 436, 1964. [ Links ]
6. CARPENTIER, P.J.; BETTINK, P.J.; HOP, W.C. y cols.: Reflux-a retrospective study of 100 ureteric reimplantations by the Politano-Leadbetter method and 100 by the Cohen technique. Br. J. Urol., 54: 230, 1982. [ Links ]
7. BURBIGE, K.A.: Ureteral reimplantation: a comparison of results with the cross-trigonal and Politano-Leadbetter techniques in 120 patients. J. Urol., 146: 1352, 1991. [ Links ]
8. WACKSMAN, J.: Initial results with the Cohen cross-trigonal ureteroneocystotomy. J. Urol., 129: 1198, 1983. [ Links ]
*9. MARBERGER, M.; ALTWEIN, J.E.; STRAUB, E. y cols.: The Lich-Gregoir antireflux plasty: experiences with 371 children. J. Urol., 120: 216, 1978. [ Links ]
10. GREGOIR, W.; SCHULMAN, C.C.: Extravesical antirefluxplasty (authors transl). Urologe A., 16: 124, 1977. [ Links ]
**11. ARAP, S.; CABRAL, A.D.; DE CAMPOS FREIRE, J.G. y cols.: The extra-vesical antireflux plasty. Statistical analysis. Urol. Int., 26: 241, 1971. [ Links ]
12. STENBERG, A.; LACKGREN, G.: A new bioimplant for the endoscopic treatment of vesicoureteral reflux: Experimental and short-term clinical results. J. Urol., 154: 800, 1995. [ Links ]
*13. FREY, P.; LUTZ, N.; JENNY, P. y cols.: Endoscopic subureteral collagen injection for the treatment of vesicoureteral reflux in infants and children. J. Urol., 154: 804, 1995. [ Links ]
14. BHATTI, H.A.; KHATTAK, H.; BOSTON, V.E.: Efficacy and causes of failure of endoscopic subureteric injection of Teflon in the treatment of primary vesicoureteric reflux. Br. J. Urol., 71: 221, 1993. [ Links ]
*15. HAFERKAMP, A.; CONTRACTOR, H.; MOHRING, K. y cols.: Failure of subureteral bovine collagen injection for the endoscopic treatment of primary vesicoureteral reflux in long-term follow-up. Urology, 55: 759, 2000. [ Links ]
16. DE GRAZIA, E.; CIMADOR, M.: Long-term follow-up results of vesico-ureteral reflux treated with subureteral collagen injection (SCIN). Minerva Pediatr., 52: 7, 2000. [ Links ]
**17. ATALA, A.; KAVOUSSI, L.R.; GOLDSTEIN, D.S. y cols.: Laparoscopic correction of vesicoureteral reflux. J. Urol., 150: 748, 1993. [ Links ]
18. GILL, I.S.; PONSKY, L.E.; DESAI, M. y cols.: Laparoscopic cross-trigonal Cohen ureteroneocystostomy: Novel technique. J. Urol., 166: 1811, 2001. [ Links ]
19. EHRLICH, R.M.; GERSHMAN, A.; FUCHS, G.: Laparoscopic vesicoureteroplasty in children: initial case reports. Urology, 43: 255, 1994. [ Links ]
20. JANETSCHEK, G.; RADMAYR, C.; BARTSCH, G.: Laparoscopic ureteral anti-reflux plasty reimplantation. First clinical experience. Ann. Urol. (Paris), 29: 101, 1995. [ Links ]
21. MEDICAL VERSUS SURGICAL TREATMENT OF PRIMARY VESICOURETERAL REFLUX: Report of the International Reflux Study Committee. Pediatrics, 67: 392, 1981. [ Links ]
![]() Dirección para correspondencia:
Dirección para correspondencia:
Francisco Tibor Dénes
Rua Barata Ribeiro, 414 conj. 35
São Paulo. CEP 01308-000 (Brasil).
ftdenes@terra.com.br