Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Archivos Españoles de Urología (Ed. impresa)
versión impresa ISSN 0004-0614
Arch. Esp. Urol. vol.62 no.1 ene./feb. 2009
Ocular proptosis in a patient with adenocarcinoma of the prostate
Proptosis ocular en paciente con adenocarcinoma de próstata
José Antonio Contreras Ibáñez1, Paula Romero Cores2 and Manuel Beltrán Ruiz-Henestrosa3
Medical Oncology Department1. Internal Medicine Department2. Anatomical Pathology Department3. University Hospital Puerta del Mar. Cádiz. Spain.
SUMMARY
Objective: To reach information on a rare clinical finding secondary to an infrequent location of tumour dissemination in prostatic cancer.
Methods: We present a case of an adult male with ocular left proptosis and history of prostatic cancer.
Conclusions: In adults males, the prostatic cancer should be born in mind in the differential diagnosis of the masses in orbital location.
Key words: Orbital metastasis. Prostatic adenocarcinoma. Ocular proptosis.
RESUMEN
Objetivo: Aportar información sobre un raro hallazgo clínico secundario a una localización infrecuente de diseminación tumoral en un cáncer de próstata.
Métodos: Se presenta el caso de un varón adulto con proptosis ocular izquierda y antecedente de cáncer de próstata.
Conclusiones: Incidir en que el cáncer de próstata debe de ser tenido en cuenta en el diagnóstico diferencial de masas orbitarias en varones adultos.
Palabras clave: Metástasis orbitarias. Adenocarcinoma de próstata. Proptosis ocular.
Introduction
Ocular proptosis or exophthalmos, consists of the forward displacement of the eyeball, and it is an uncommon finding in daily clinical practice.
Prostate adenocarcinoma is the most common neoplasm of the urogenital system and it represents the third cause of death from cancer in men (1).
The most common metastatic sites are the skeleton and the pelvic lymph glands. Intracranial involvement is rare and mostly appears as part of a widespread disease (2-4).
Metastases represent approximately 6% of all orbital neoplasms in adults. It has been reported that up to 30% of all orbital metastases are the initial manifestations of hidden primary tumours (5). Most of them are derived from breast and lung cancer (6,7). They are only exceptionally associated to the prostate, although this is the second most common cause in males (8,9).
We present the case of a male patient who, during the course of prostate cancer, presented left ocular proptosis which imaging tests showed was an orbital metastasis, an exceptional site regarding prostate cancer.
Case report
A 60-year old male, with no pathological history of interest, referred from the Urology Department of our center with a diagnosis of stage IV prostate adenocarcinoma and multiple bone metastases, in hormone resistant phase.
In February, 2004, due to prostate syndrome (pollakiuria and micturitional urgency), his General Practitioner (GP) requested a PSA determination showing a value of 12 ng/ml, so he was referred to a specialist. He underwent transrectal ultrasound and ultrasound-guided prostate biopsy, diagnosing bilobular adenocarcinoma, Gleason 7 (4+3). The extension study showed evidence of retro-peritoneal ganglionic metastases and multiple sites of pathological hyperuptake (spine, neck and diaphysis of femur, pelvis). Complete androgenic blockage was instated, with gonadotropin releasing hormone analogue (A-LHRH) and antiandrogen. The PSA level returned to normal in 4 months (June 04) with this treatment.
The patient received pain killing treatment for bone pain with NSAIDs and morphic treatment. He was also treated with dorsolumbar vertebral irradiation with 30 Gy administered in 10 sessions.
In April 2006, when the patient was asymptomatic, the PSA level started to increase gradually to 7.3, 13.1, 21 ng/ml, with testosterone remaining at castration levels. It was then decided to suspend the antiandrogen. The biochemical response was good, and the situation returned to normal by August 2006.
Unfortunately, in November 2006 he visited the emergency room complaining of intense and disabling generalized bone pain, in spite of an increased dose of analgesics (VAS = 8-9) for which he was treated with strontium (St) in the Nuclear Medicine Department. The clinical symptoms were also accompanied by PSA levels of 850 ng/ml.
In December 2006, with his informed consent, we decided to start palliative CT with docetaxel and prednisone. We also started therapy with bone resorption inhibitors (zoledronic acid). The clinical response was satisfactory, with analgesic control (VAS = 2-3) and PSA reduction to 150 ng/ml.
On 15/02/07, he visited the emergency room, referring that for the last 15 days he had been presenting protrusion of the left eyeball, finding it difficult to completely separate the eyelids.
Neurological examination
Proptosis, palpebral ptosis, little reactive mydriasis secondary to affectation of the third pair. No orbital murmurs.
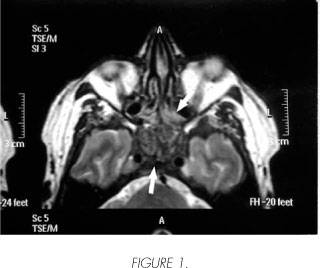
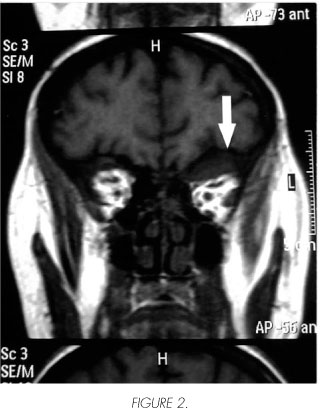
Orbital NMR
Metastatic replacement of the entire central segment of the cranial base, the bone marrow of the vertebrae included in the study and part of the cranial diploé. The ceiling and lateral wall of the left orbit were affected and expanded, causing proptosis of the eyeball. The greater wing of the left sphenoid bone is replaced and thickened and it clearly extends to the wall of the left cavernous sinus and cleft (Figure 1). Similar, but less advanced, changes are found in the bones conforming the contra-lateral orbit. The lesion on the ceiling of the left orbit is accompanied by a lesion of the soft tissues causing lower displacement of the orbital muscles. The sequences with contrast show heterogeneous hyperuptake at all the described lesions (Figure 2).
He received palliative radiation on all the affected areas, rapidly declining and dying on 21/03/07.
Discussion
Prostate adenocarcinoma is the most common neoplasm of the urogenital system and it represents the third cause of death from cancer in men (1).
The most common metastatic sites are the skeleton and the pelvic lymph glands. Intracranial involvement is rare and mostly appears as part of a widespread disease (2-4).
Metastases represent approximately 6% of all orbital neoplasms in adults. It has been reported that up to 30% of all orbital metastases are the initial manifestations of hidden primary tumours (5). Most of them are derived from breast and lung cancer (6,7). They are only exceptionally associated to the prostate, although this is the second most common cause in males (8,9).
The routes of extension from the primary tumor are the lymphatic and blood systems through the Batson intervertebral venous plexus, so when bone is affected it is basically the axial skeleton. Orbital metastases are produced through the arteries (3), through tumor emboli which cross the pulmonary filter.
The clinical symptoms are not very specific and can appear in many other intracranial processes, so neuro-imaging techniques, such as NMR in our case, are an enormous aid for differential diagnosis. In this case, in view of the prior diagnosis of a neoplasm, we did not require confirmation from a cytology-biopsy of the orbital lesion.
From a therapeutic perspective, external radiotherapy can be effective. This was not the case in our patient, in whom the disease was very advanced, and who presented a relatively low functional status. All these aspects are important for the decision-making process (1).
The specific prognosis of metastases at this site is unknown 10 but, as survival was so short after diagnosis in our case, we suspect that it worsens considerably.
To conclude, we would like to emphasize that prostate cancer should be considered in the differential diagnosis of orbital masses in adult male patients with neurological symptoms and imaging tests revealing intracranial lesions.
 Correspondence:
Correspondence:
José Antonio Contreras Ibáñez
Servicio de Oncología Médica (9a Planta)
Hospital Universitario Puerta del Mar
Avda. Ana de Viya, 21
11009 Cádiz. (Spain).
joseantonio.contrerasibaez@gmail.com
Accepted: 19th February, 2008.
References and recomended readings (*of special interest, **of outstanding interest)
1. Rioja LA, Sanz Velez JI, Gil Sanz MJ, Allepuz Losa C. Carcinoma de próstata. En: Tratado de Urología. Editado por JR Proas. Jiménez Cruz JF, Rioja Sanz LA. Barcelona 1993; 2:1205-36. [ Links ]
**2. Pieras E, Rosales A, López, H, Villavicencio H, Vicente J. Metástasis intracraneales en cáncer de próstata. Actas Urol Esp 2000; 24: 626-31. [ Links ]
**3. Romero P, Pelluch A, Lobato JJ et al. Exoftalmos por metástasis orbitária de carcinoma prostático. Arch Esp de Urol 1991; 44: 191-94. [ Links ]
*4. Sutton MA, Watkins HL, Green LK, Kadmon D. Intracranial metastases as the first manifestation of prostate cancer. Urology 1996; 48: 789-93. [ Links ]
5. Carriere VM, Karcioglu ZA, Apple DJ, Insler MS. A case of prostate carcinoma with bilateral orbital metastases and the review of the literature. Ophthalmology 1982; 89: 402-06. [ Links ]
6. Prat-Bartomeu J. Metástasis orbitarias en el adulto. Rev Neurol 2000; 31: 1261-63. [ Links ]
7. Boldt HC, Nerad JA. Orbital metastases from prostate carcinoma. Arch Ophthalmol 1988; 106: 1403-08. [ Links ]
**8. González C, Kuzel T, Carter M. Metastatic adeno-carcinoma of the prostate to the orbit as a presenting symptom. J Urol 1997; 157: 625. [ Links ]
*9. Inagaki T, Ebisuno S, Milla M, Nakamura J. A case of prostatic cancer metastasing to the orbit. Int J Urol 1999; 6:114-15. [ Links ]
10. Aubert J, Irani J, Saint-Blanca TP. Orbital metastasis of prostatic cancer. Clinical and therapeutic aspects. A propos of a case. Chirurgie 1997; 121: 672-75. [ Links ]











 texto en
texto en