My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.62 n.4 May. 2009
Mondor’s síndrome. Case review and bibliographic review
Síndrome de Mondor: revisión de la literatura a propósito de un caso
Roberto Molina Escudero, Ramiro Cabello Benavente, Juan Ignacio Monzo Gardiner, Iñigo López Diez, Juan Tabares Jiménez, Eva Paños Fagundo and Carlos Hernández Fernández
Department of Urology. Hospital General Universitario Gregorio Marañón. Madrid. Spain.
SUMMARY
Objective: We review the presen-tation, diagnosis and treatment of Mondor's disease of the penis, with the contribution of a new clinical case.
Methods: A 43-year-old male reported to the emergency room with preputial inflammation and edema associated to swelling of the dorsal region of the penis for the previous three weeks.
Results: Doppler ultrasound revealed thrombosis of the superficial dorsal vein of the penis, associated to candidiasic balanitis. Treatment was provided in the form of nonsteroidal antiinflammatory drugs and antibiotic and antifungal agents. The symptoms disappeared after 7 days of treatment, followed by the development of punctate phimosis that required circumcision.
Conclusions: Mondor's syndrome is an infrequent condition usually caused by trauma, though it is important to consider the possibility of associated coagulation problems, infections and neoplastic processes.
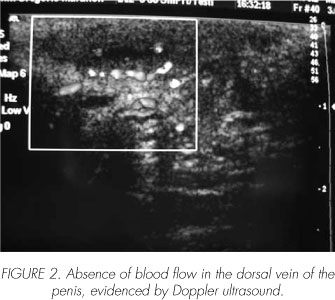
Doppler ultrasound is the technique of choice for confirming the diagnosis and resolution of the condition.
Treatment is based on nonsteroidal antiinflammatory medication, antibiotherapy and sexual abstinence. The use of anti-coagulation is controversial, but may prove useful in patients with coagulation disorders.
Key words: Mondor's syndrome. Venous thrombosis. Anticoagulation.
RESUMEN
Objetivo: Revisar la forma de presentación, diagnóstico y tratamiento de la enfermedad de Mondor del pene mediante la presentación de un nuevo caso.
Métodos: Varón de 43 años que acude a urgencias por inflamación y edema prepucial asociado a tumefacción del dorso peneano de 3 semanas de evolución.
Resultados: Se realizó ecografía doppler peneana con el diagnóstico de trombosis del la vena dorsal superficial del pene, asociada a balanitis candidiásica. Se instauró tratamiento con antiinflamatorios no esteroideos, antibiótico y antifúngico. La sintomatología desapareció tras 7 días de tratamiento, con desarrollo posterior de fimosis puntiforme que requirió circuncisión.
Conclusiones: La enfermedad de Mondor es una patología infrecuente cuya etiología suele ser traumática, aunque es importante tener en cuenta su posible asociación a trastornos de la coagulación, infecciones y neoplasias.
La técnica de elección para la confirmación del diagnostico y la resolución del cuadro es la ecografía doppler.
El tratamiento se fundamenta en AINES, antibioterapia y reposo de la actividad sexual. La utilización de anticoagulantes es un aspecto controvertido, aunque de utilidad en los pacientes que presentan trastornos de la coagulación.
Palabras clave: Síndrome de Mondor. Trombosis venosa. Anticoagulación.
Introduction
In 1939, Mondor established the first diagnosis of thoracoepigastric vein thrombosis in a woman. In 1955, Braun-Falco described generalized phlebitis of the dorsal zone of the penis, and in 1958 Helm and Hodge reported thrombosis of the superficial dorsal vein of the penis, referring to it as "Mondor's disease of the penis" - this being the term used to describe the condition today.
Mondor's syndrome appears most often in patients between 20-45 years of age, and generally 24-48 hours after prolonged sexual activity. Its main manifesting feature is the presence of a palpable and painful cord on the dorsal surface of the penis.
Case report
A 43-year-old male reported to the emergency room with preputial inflammation and edema associated to swelling of the dorsal region of the penis for the previous three weeks.
The patient denied risk sexual practices, micturition syndrome or fever. He complained of pain in the dorsal region of the penis, related to the presence of an indurated and palpable cord in the zone, and which became accentuated upon erection.
The case history showed him to be a smoker of 20 cigarettes/day, with no background disease or regular treatment. The familial history was likewise unremarkable.
The physical examination revealed intense preputial inflammation, with whitish erosions suggestive of candidiasis. The dorsal region of the penis presented a hard and painful cord extending from the base to the balanopreputial sulcus, associated to inflammation of the adjacent tissue. The rest of the physical examination proved normal.
With the suspicion of Mondor's disease, penile Doppler ultrasound was carried out, with confirmation of the diagnosis (Figure 1 and 2).

Treatment was started with topical fluconazole as a single application/12 hours, amoxicillin-clavulanate 875 mg/8 hours, and ibuprofen 600 mg/8 hours for 10 days, together with sexual abstinence until resolution of the clinical condition.
During the first week the dorsal cord gradually decreased distally, along with the pain. The lesions related to candidiasis disappeared. At this time exploration revealed punctate phimosis preventing retraction of the prepuce; circumcision thus proved necessary. Doppler ultrasound after 6 weeks revealed repermeation of the superficial vein of the penis, with no venous thrombus.
Discussion
Mondor's syndrome is intimately related to intense and repeated mechanical trauma of the penis, as during vigorous sexual activity and the use of constricting elements during intercourse. It is also seen in patients with other disorders such as tumors (prostate and bladder neoplasms, as well as migratory thrombophlebitis in the context of pancreatic cancer), coagulation disorders (protein C and S deficiencies) and genitourinary infections (3).
The histopathological study reveals thinning of the vascular wall, with the loss of differentiation between the intimal layer (which appears thinned, with thickened endothelial cells) and the connective tissue (reduced elastic tissue). The venous lumen moreover appears occupied by conventional thrombotic material (red cells, fibrin, platelets) associated to a local inflammatory reaction (4).
The clinical picture evolves in three phases: acute, subacute and repermeation. The acute phase manifests within 24-48 hours, is the least constant of the three phases, and is associated with intense pain and occasionally also fever. Posteriorly the pain decreases in intensity and may be associated with irritative micturition symptoms. This situation can last 4-8 weeks. Finally, repermeation of the vein is observed, with elimination of the thrombus and resolution of the clinical picture within 6-8 weeks (2).
The tentative diagnosis is based on the anamnesis and physical exploration findings, with palpation of a hard and painful cord ("metal wire") on the dorsal surface of the penis. The cord occasionally may appear pulsatile. Blood and urine testing is advised to discard thrombophilia and infection as possible causes of the disorder. Penile Doppler ultrasound is the technique of choice for confirming the diagnosis. This technique makes it possible to differentiate Mondor's disease from other processes characterized by pain and thickening of the dorsal region of the penis without venous thrombosis - such as venereal sclerotizing lymphangitis or La Peyronie's disease (5). A biopsy is not indicated on a routine basis. Treatment is conservative, with rest, nonsteroidal antiinflammatory medication, and occasionally topical heparinizing agents to reduce the pain and local inflammation (6). The use of antibiotics is particularly indicated in patients with evidence of cellulites at physical examination, as well as in the acute phase of the disorder. The indicated antimicrobials are those that cover the bacterial flora commonly implicated in skin processes (e.g., amoxicillin - clavulanate or cloxacillin). Local anesthetics such as bupivacaine are not routinely employed, due to their brief action, and because they may exacerbate any existing cellulites (2).
The use of anticoagulants is subject to controversy. In general terms, the literature does not recommend their use in patients diagnosed with Mondor's syndrome. However, Sasso et al. (4) recommend anticoagulation in the acute phase (24-48 hours) in order to avoid possible additional thrombotic events. They are also indicated in patients with a history of thrombotic disease or coagulation disorders (activated C protein or S protein deficiencies, etc.). In the rare case of thrombosis of the deep dorsal vein of the penis, Shen et al. advocate anticoagulation in the same way as in other cases of deep venous thrombosis, due to the associated risk of pulmonary thromboembolism. In any case, anticoagulation must be conditioned to the existing benefit / risk ratio, and to the possibility of further thrombotic events (7).
In those cases where the symptoms persist after 8 weeks, surgery can be considered - the most common technique being thrombectomy, and in some cases excision of the superficial dorsal vein of the penis. In some cases the preputial edema and surrounding inflammation caused by the vascular damage may give rise to phimosis, which is amenable to treatment in the form of circumcision (8).
Conclusions
Mondor's syndrome is an infrequent and generally self-limiting condition caused by vigorous sexual activity, coagulation problems, infections and neoplastic processes. The typical symptoms are pain and the presence of a palpable cord in the dorsal zone of the penis. When the condition is clinically suspected, doppler ultrasound is indicated, revealing thrombosis of the superficial dorsal vein of the penis.
Treatment is based on nonsteroidal antiinflammatory medication, antibiotherapy in selected cases, and sexual abstinence. The use of anticoagulation is controversial, and is conditioned to the existing benefit / risk ratio, though it appears to be useful in the acute phase of the disorder, and in those presentations associated to thrombophilia.
 Correspondence:
Correspondence:
Roberto Molina Escudero
Juan Esplandiú, 9A - 14 - B
28007 Madrid. (Spain).
robersescu@hotmail.com
Accepted for publication: June 18th, 2008.
References and recomended readings (*of special interest, **of outstanding interest)
*1. Kumar B, Narang T, Radotra BD. Mondor's disease of penis: a forgotten disease. Sex Transm Infect, 2005; 81:480-482. [ Links ]
**2. Rodríguez Faba O, Rodríguez Muntaner L. Trombosis de la vena dorsal del pene (Flebitis de Mondor). Aportación de un nuevo caso. Actas Urol Esp 2006; 30: 80-82. [ Links ]
3. Schmidt B, Schwarz T. Spontaneous Thrombosis of the deep dorsal penile vein in a patient with trombophilia. J Urol; 2000; 164:1649 [ Links ]
**4. Sasso F, Gulino G, Basar M, et al. Penile Mondor's disease: an underestimated pathology. BJU 1996; 77: 729-732. [ Links ]
5. Griger D, Tanae A, Douglas B. Penile Mondor's disease in a 22-year-old man. JAOA 2001; 101: 235-237. [ Links ]
6. Al-Mwalad, Loertzer H, Wicht A., et al. Subcutaneous penile vein thrombosis: Pathogenesis, diagnosis and therapy. Urology 2006; 67: 586-588. [ Links ]
7. Shen H, Liu S, Wang S, et al. Elevated plasma factor VIII coagulant activity presenting with thrombophlebitis of the deep dorsal vein of the penis. Int J Urol 2007; 14: 663-664. [ Links ]
*8. Lilias LA, Mumtaz FH, Madders DJ. Phimosis after penile Mondor's phlebitis. BJU Int 1999; 83: 520-521. [ Links ]
9. Dicuio M, Pomara G, Cuttano MG, et al. Penile mondor's disease after intensive masturbation in a 31- and a 33-year-old man. Thromb Haemost 2003; 90: 155-156. [ Links ]











 text in
text in 


