My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.62 n.5 Jun. 2009
Emphysematous pyelonephritis. Case report
Pielonefritis enfisematosa. Comunicación de un caso
Tristán Dellavedova, María Laura Racca, Rolando Ponzano, Juan Pablo Sarría, Federico Minuzzi and Gustavo Minuzzi.
FUCDIM (Fundación Urológica Córdoba para la Docencia e Investigación Médica). Córdoba. Argentina.
SUMMARY
Objective: To describe an unusual case of emphysematous pyelonephritis, a disease with high morbidity and mortality.
Methods: We present the case of a 62-year old diabetic female with history of kidney stones, who consulted for fever, left lower-back pain and impairment of the general condition. Abdominopelvic computed tomography revealed a perinephric collection of air reaching the abdominal wall.
Results: After initial medical management with antibiotics and general supportive measures, we performed an open incision and drainage. A week later, signs of sepsis reappeared and the left kidney was excised. The patient died two weeks later of septic shock.
Conclusions: This disease must be suspected in diabetic females with renal lithiasis and pyelonephritis not responding to treatment, and impaired general condition. Early diagnosis (computed tomography is the gold-standard) and supportive measures are essential for initial management. Surgery can be open (drainage, initial or deferred nephrectomy), percutaneous (nephrostomy) or endoscopic (double-J stent). Conservative management is a choice in bilateral or mild cases. Mortality rate is high and worsens with delayed therapy.
Key words: Pyelonephritis. Emphysematous pyelonephritis. Complicated urinary tract infection. Urosepsis. Diabetes mellitus.
RESUMEN
Objetivo: Describir un caso de pielonefritis enfisematosa, patología de baja incidencia con alta morbimortalidad.
Métodos: Se presenta el caso de una mujer de 62 años, diabética, con litiasis renal. Consulta por fiebre, lumbalgia izquierda y deterioro del estado general. La TAC abdómino-pelviana evidencia aire en la fosa renal izquierda, que infiltra la pared abdominal.
Resultado: Tras estabilización inicial con antibioticoterapia y medidas de reanimación, se realizó drenaje de fosa renal por lumbotomía, debido a urosepsis. Una semana después reaparecen signos de sepsis y se realiza nefrectomía simple. Óbito 14 días después por shock séptico.
Conclusiones: Este cuadro debe sospecharse en mujeres diabéticas con antecedentes de litiasis renal, que presentan pielonefritis refractaria al tratamiento y compromiso del estado general.
- El diagnóstico precoz (tomografía computada de elección) y las medidas de sostén son clave para el manejo inicial.
- El tratamiento inicial es el avenamiento con puesta a plano de toda la zona afectada, sin descartar la nefrectomía, que puede realizarse de inicio o en forma diferida.
- En casos leves o bilaterales con diagnóstico precoz, se puede intentar manejo médico inicial, con estricto seguimiento clínico y con imágenes, y eventual desobstrucción percutánea (nefrostomía) o endoscópica (catéter "pig-tail"). La mortalidad es elevada y la demora en intervenir incrementa su incidencia.
Palabras clave: Pielonefritis. Pielonefritis enfisematosa. Infección urinaria complicada. Urosepsis. Diabetes mellitus.
Introduction
Emphysematous pyelonephritis (EP) is an acute, necrotizing and fast developing infection of renal and perirenal tissues, caused by gas-producing enterobacteriae (Escherichia coli and other Gram negative bacteria are the usual agents; fungus or anaerobic organisms are exceptionally isolated). This disease generally affects only one kidney, but is bilateral in 5-7% of the cases. The incidence is higher among females between 40 and 60 years old, and also in diabetic or immunocompromised patients. Mortality rates are 21-29% with surgical treatment, 60-75% with conservative management and 80% if the disease extends to perirenal spaces (1,2).
EP presents with symptoms of severe pyelonephritis not responding to medical treatment and may lead to sepsis and shock. Urine and blood cultures usually allow isolation of the bacteria. Up to 20% of the patients present with fever without local symptoms (3).
The presence of air in the kidney or perirenal tissues confirms the diagnosis and can be seen with plain X-rays or ultrasound; however, computed tomography is the most sensitive and reliable method (4).
Management of EP includes general support, antibiotics, and percutaneous, endoscopic or open drainage according to disease severity and local progression. In many cases, immediate or deferred nephrectomy is required. Conservative management is reserved for cases with early diagnosis and incipient lesions (3,4).
Case report: we present the case of a 62 year-old obese female with uncontrolled diabetes. She had history of a left staghorn stone with incomplete treatment. She consulted due to fever and low back left pain for the last 7 days, oral mycosis and serious impairment of her general condition. Blood test showed leukocytosis with neutrophilia, high glucose levels with acidosis, and high values of urea and creatinin. Her abdomen was soft and presented pain in the left flank and lower back.
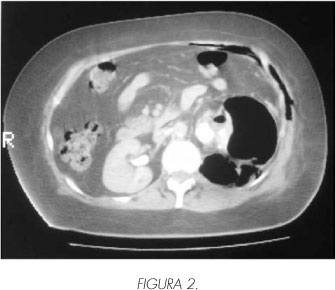
Abdominal ultrasound and plain X-ray showed air in the left kidney. Abdomino pelvic tomography scan diagnosed gas in the left kidney and perirenal tissues, which infiltrated the abdominal wall (Figures 1 to 3).


Due to the fast deterioration of her general condition, open surgical drainage was performed through a lumbotomy, to avoid contamination of the peritoneal cavity. Air was evacuated and devitalized tissues were removed. After initial improvement, signs of sepsis reappeared a week later, and simple nephrectomy was performed. She had good postoperative outcome, but two weeks later, she developed a respiratory infection that resulted in sepsis. Pus commenced to drain from the surgical wound and a "toilette" was made, but the patient died due to multiple organ failure and a nosocomial respiratory infection.
Discussion
EP is a severe complicated urinary tract infection (UTI), favoured by predisposing factors (3). Gram negative bacteria, the usual agents of UTIs, behave as anaerobics under low oxygen pressure, producing gas from glucose (4). E. coli is the most frequently isolated organism, followed by Klebsiella pneumoniae, Proteus mirabilis, Morganella morgagni, Pseudomona aeruginosa and Enterobacter. Fungus or anaerobic bacteria rarely appear and in 20% of the cases, more than one agent can be found (1,2,4).
Infection begins in the renal parenchima or the collecting system, sometimes reaching perirenal spaces, retroperitoneum or neighbouring vessels (2,5). This usually presents in immunocompromised patients; 90-95% are diabetics (1); EP also presents in transplanted kidneys (6) or after renal surgeries (7).
Women account for the majority of cases (male/female ratio 1:5.9), this can be attributed to the higher incidence of UTIs in females (1).
Among predisposing factors, we can mention high glucose concentration in renal tissue, anaerobic-behaving enterobacteriae, urinary tract obstruction (occurring in 15-22% of the patients), altered tissue perfusion and poor immune response (1,8).
Clinical presentation cannot be differentiated from other forms of acute pyelonephritis. Classic symptoms as fever, chills and low back pain are usually present, although more severe symptoms, like confusion, shock or signs of uremia, can be detected: (1). Laboratory findings are high blood glucose level, acidosis or hydroelectrolytic disorders. Advanced cases may present as urosepsis. Urine cultures are generally positives, the same agent can also be isolated, in lesser extent, in blood cultures (9).
Prognostic factors indicating poor response to therapy and risk of death have been proposed, these are not exclusive for EP but their finding indicates poor prognosis. Among them we can cite: thrombocytopenia (less than 120,000 platelets), acute renal failure (serum creatinin >3 mg/dl), altered mental state (lethargy, stupor) and signs of septic shock (1,10). Whenever 2 or more of these are present, conservative management is contra-indicated since failure rate reaches 92% (vs 15% with only one factor). No correlations were found between bad prognosis and age, gender, site of infection and blood glucose level (1).
Initial diagnosis is made by ultrasound and plain X-ray, but computed tomography (CT) with intravenous contrast is the "gold-standard" since it identifies the gas, evaluates local and perirenal compromise, as well as the urinary tract and surrounding vessels, helping also in the surgical planning (4). Huang and Tseng, in 2000, proposed the following radiological classification based on CT findings (10):
I: Gas in the collecting system (emphysematous pyelitis)
II: Air in the parenchyma without extrarenal extension
IIIA: Gas or abscess in the perirenal space
IIIB: Gas or abscess in the pararenal space
IV: Bilateral disease or in a unique kidney
Management of EP is not clear due to the low incidence of this disease. Nephrectomy is considered the "gold-standard" in patients who can undertake a surgical procedure. Conservative management and percutaneous or endoscopic drainage are options for severely compromised patients who cannot tolerate a surgery, in patients with bilateral compromise, those with only one kidney, or as initial approach in mild presentations (10,11).
Non-invasive management has higher rates of mortality and therapy failure, either with the previously mentioned options or partial renal resection. Nephrectomy, on the other side, should be proposed to patients with healthy contralateral kidney, since it provides complete cure in most of the cases (3,12). Kidney resection can be immediate or deferred, achieving best results with the first option (faster recovery and less postoperative complications) (13). Among cases presenting with urosepsis or shock, as our patient, where nephrectomy cannot be performed and a less invasive approach is required, a percutaneous drainage or through a lumbotomy can be done (14). During the follow-up, patients treated with this procedure need more reinterventions and have longer hospital stay (13).
Tailored treatment according to the CT stage has been proposed, using only antibiotics and percutaneous or endoscopic drainage if required, for stages I and II, and for upper stages a more aggressive approach with nephrectomy or wide surgical drainage, due to the high failure rates of conservative therapies (1).
Conclusion
EP should be suspected in rapidly deteriorating immunocompromised patients with pyelonephritis not responding to treatment. CT scan is the method of choice to evaluate local and perirenal tissues. Early diagnosis and management make the difference in survival rates of these patients.
 Correspondence:
Correspondence:
Tristán Dellavedova
FUCDIM
Wenceslao Paunero 2193
Córdoba XHPB 5016 (Argentina).
trisdellavedova@hotmail.com
Accepted: December 6th, 2008
References and recomended readings (*of special interest, **of outstanding interest)
**1. Moreno Romero R, Viveros Contreras C, Lugo García J, De la Cruz Trejo J, Diaz Espinosa de los Monteros C. Pielonefritis enfisematosa. Rev Mex Urol, 2006; 66 (2):74-82. [ Links ]
2. Herring W. Emphysematous pyelonephritis. Disponible en: http://www.learningradiology.com , consultado el 18/07/08. [ Links ]
3. Grabe M, Bishop MC, Bjerklund-Johansen TE, Botto H, Cek M, Lobel B, et al. The management of urinary and male genital tract infections. European Association of Urology, Guidelines 2008; 56. [ Links ]
**4. Blanco Díez A, Barbagelata Lopez A, Fernández Rosado E, Casas Muiño R, Chantada Abal V, González Martín M. Pielonefritis enfisematosa: Presentación de un caso y revisión de la literatura. Actas Urol Esp, 2003; 27 (9):721-725. [ Links ]
5. Cheng KW, Huang JJ, Wu MH, Lin XZ, Chen CY, Ruana MK. Gas in hepatic veins, a rare and critical presentation of emphysematous pyelonephritis. J Urol, 1994; 151:125-126. [ Links ]
6. Fujita S, Watanabe J, Reed AI, Hemming AW, Solis D, Netzel TC, et al. Case of emphysematous pyelonephritis in a renal allograft. Cl Transplantation, 2005; 19 (4):559-562. [ Links ]
7. Jalon Monzon A, García Rodríguez J, Rodríguez Faba O, et al. Pielonefritis enfisematosa. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid. Consultado el 21/10/08. Actas Urol Esp, 2003; 27 (3):250. [ Links ]
8. Peter JV, Biradar V, Peaje SL. Emphysematous pyelonephritis. Med J Australia 2006; 184 (10):533. [ Links ]
*9. Tang HJ, Li CM, Yen MW. Clinical characteristics of emphysematous pyelonephritis. J Microbiol Immunol Infect, 2001; 34:125-130. [ Links ]
**10. Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med, 2000; 160: 797-805. [ Links ]
*11. Melero MJ, Sarquis SG, Biancolini C, Baredes N, Villa R. Pielonefritis enfisematosa aguda bilateral. Un desafío terapéutico. Medicina, 2007; 67 (3): 282-284. [ Links ]
12. Eloubeidi MAS, Fowler VG Jr. Images in clinical medicine. Emphysematous pyelonephritis. N Engl J Med, 1999; 341 (2):737. [ Links ]
13. Abdul-Halim H, Kehinde EO, Abdeen S, Lashin I, Al-Hunayan AA, Al-Awadi KA. Severe emphysematous pyelonephritis in diabetic patients. Urol Int, 2005; 75:123-128. [ Links ]
14. Rathod KR, Narlawar RS, Garg A, Lolge S. Percutaneous conservative management of emphysematous pyelonephritis. J Postgrad Med, 2001; 47:66. [ Links ]











 text in
text in 


