Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.33 no.5 Madrid sep./oct. 2016
https://dx.doi.org/10.20960/nh.561
TRABAJO ORIGINAL / Nutrición artificial
Enteral feeding through endoscopic gastrostomy in amyotrophic lateral sclerosis patients
Nutrición enteral por gastrostomía endoscópica en pacientes con esclerosis lateral amiotrófica
Gonçalo Nunes1, Carla Adriana Santos1, Miguel Grunho2,3 and Jorge Fonseca1-3
1Gastroenterology Department. Hospital Garcia de Orta. GENE-Artificial Feeding Team. Almada, Portugal.
2Neurology Department. Hospital Garcia de Orta. Almada, Portugal.
3CIIEM, Centro de Investigação Interdisciplinar "Egas Moniz". Monte da Caparica, Portugal
ABSTRACT
Background: Dysphagia is common in amyotrophic lateral sclerosis (ALS) and may result in malnutrition. Endoscopic gastrostomy (PEG) is recommended when oral feeding is unsafe. This work aims to assess the effectiveness and safety of PEG feeding on improving nutritional and prognostic parameters in ALS patients.
Methods: Observational and retrospective study using records from ALS patients referred for gastrostomy. Age, gender and mortality data were collected. NRS 2002, body mass index (BMI), serum albumin, transferrin and total cholesterol were recorded at the time of PEG (T0) and repeated after 3 months (T3). The evolution of these parameters was analysed and compared to survival.
Results: Data from 37 ALS patients (18 men/19 women) aged 43-88 years (mean: 69 years). All patients presented NRS 2002 ≥ 3 points. On average, patients underwent gastrostomy 11 months after diagnosis. No major procedural complications occurred. Mean survival after diagnosis was 22.2 months. Mortality rate at 3 months was 21.6% with a mean survival after PEG of 11.2 months. Albumin, transferrin and cholesterol levels increased from T0 to T3 without reaching statistical significance. Higher albumin (R = 0.3) and transferrin (R = 0.4) at admission tend to be positively correlated with survival. Mean BMI was similar at the two moments but higher initial values were associated with better outcome (R2 = 0.39, p < 0.05).
Conclusions: PEG is a safe and effective technique for enteral feeding and should be considered early in ALS patients with dysphagia. Higher BMI predicts longer survival. The association between higher serum proteins and survival must be confirmed in further studies.
Key words: Amyotrophic lateral sclerosis. Nutrition. Gastrostomy. PEG.
RESUMEN
Introducción: la disfagia es común en pacientes con esclerosis lateral amiotrófica (ELA) y pude resultar en desnutrición. Se recomienda la gastrostomía endoscópica (PEG) cuando la alimentación oral no es más segura. Este trabajo tiene como objetivo evaluar la eficacia y seguridad de la alimentación por PEG en la mejora de los parámetros nutricionales y de pronóstico en pacientes con ELA.
Métodos: estudio observacional y retrospectivo que utilizó los registros clínicos de pacientes con ELA referidos para gastrostomía. Se recogieron datos sobre la edad, el género y la mortalidad. Se registró el NRS 2002, el índice de masa corporal (IMC), la albúmina sérica, la transferrina y el colesterol total en el momento de PEG (T0) y después de 3 meses (T3).
Resultados: fueron recolectados los datos de 37 pacientes con ELA (18 hombres/19 mujeres), con edades comprendidas entre 43-88 años (media: 69 años). Todos los pacientes presentaron NRS 2002 ≥ 3 puntos. En promedio, los pacientes fueron sometidos a gastrostomía 11 meses después del diagnóstico. No hubo complicaciones mayores del procedimiento. La media de supervivencia después del diagnóstico de ELA fue de 22,2 meses. La tasa de mortalidad a los 3 meses fue de 21,6%, con una supervivencia media de 1,.2 meses después de PEG. Los niveles de albúmina, transferrina y colesterol aumentaron de T0 a T3, sin embargo sin alcanzar significación estadística. Mayores niveles de albúmina (R = 0,3) y de transferrina séricas (R = 0,4) en el momento de PEG tienden a estar correlacionados positivamente con una supervivencia más larga. El IMC medio fue similar en los dos momentos, pero valores iniciales más altos están asociados con un mejor pronóstico (R2 = 0,39, p < 0,05).
Conclusiones: PEG es una técnica segura y eficaz para la nutrición enteral y se debe considerar temprano en pacientes con ELA y disfagia. Un mayor IMC predice una mayor supervivencia. La asociación entre proteínas séricas más altas y la supervivencia debe ser confirmada en estudios posteriores.
Palabras clave: Esclerosis lateral amiotrófica. Nutrición. Gastrostomía. PEG.
Introduction
Amyotrophic lateral sclerosis (ALS) is a severe and relentlessly progressive neurodegenerative disease of unknown aetiology, characterized by the degeneration of both upper and lower motor neurones, leading to progressive muscle paralysis (1). ALS affects 1.7-2.1 per 100,000 person/years worldwide, most cases are sporadic (90-95%), there is a slight male gender predilection, and the mean age at diagnosis is 60 years (2).
The classical limb-onset form of the disease is mainly characterized by focal muscle weakness and wasting in the limbs (due to spinal cord involvement), while the bulbar-onset form usually presents with dysarthria, dysphagia and dyspnoea, with limb features developing later in the course of the disease (1). Additional clinical features include cognitive impairment (frontotemporal dysfunction), constipation, anxiety, depression, fatigue and insomnia (3). Since disease-modifying treatment is limited to riluzole (extends survival of patients by 3-6 months), symptomatic treatments, namely nutritional support, remain the keystone of ALS management. Notwithstanding, death due to respiratory failure ultimately occurs within 2-5 years after diagnosis (1).
During the course of ALS, a decline in nutritional status is common. Weight loss may be explained by several factors, including reduced food intake associated with decrease strength for food manipulation and chewing, impaired salivary secretion, swallowing difficulties, constipation and fear of pulmonary aspiration. On the other hand, most of these patients present a state of hypermetabolism that increases resting energy expenditure and caloric requirements (4-6). Malnutrition is an independent, negative, prognostic indicator for survival as it may exacerbate catabolism, atrophy of respiratory muscles and weakness the immune system, thus contributing for a higher risk of infection (6,7).
Interventions to maintain adequate nutritional intake include altering food consistency, increasing the number of daily meals and the use of feeding assistance devices and high calorie supplements. However, as dysphagia gradually progresses, enteral feeding is often required in the nutritional management of these patients (7). Percutaneous endoscopic gastrostomy (PEG) is used to improve nutrition in patients with ALS who develop severe dysphagia, so that food and liquid can bypass normal oral entry and be delivered directly through the PEG tube, therefore avoiding malnutrition and dehydration. PEG feeding also prevents food aspiration episodes, which can contribute to respiratory function decline and death, although microaspiration of oropharyngeal secretion remains possible in PEG-fed patients. Nevertheless, the timing of gastrostomy is not consensual, the optimal parameters of enteral feeding are not known and its potential disease-modifying effects remain uncertain (8,9).
According with different guidelines and recommendations (9-12) endoscopic gastrostomy is a safe procedure. It should be considered early when dietary counselling for food modification is not sufficient and nutrition status is compromised by severe dysphagia and weight loss (5-10% of usual body weight). Forced vital capacity (FVC) should stay above 50% at the time of the PEG procedure to prevent aspiration and minimize the respiratory risks associated with the technique. However, some trials showed that, even in patients with severe ventilatory compromise, PEG can be placed safely (9-12).
Recent systematic reviews showed no randomised controlled trials assessing the outcome of tube fed patients with ALS and indicating whether enteral nutrition is beneficial compared to the maintenance of oral feeding. The benefits of PEG on improving nutritional status have been shown in observational studies but have not been carefully tested. Some researchers describe an increase in survival time but strong results were not uniformly reported (7-8,11,13-15).
The present work aims to assess the effectiveness of PEG feeding for nutritional support in ALS patients through a retrospective review of the experience of our enteral feeding team. We intend to:
- Characterize the nutritional status of ALS patients referred for gastrostomy using anthropometric and laboratory data.
- Assess the survival of those patients and to identify factors that are associated with shorter or longer survival after the gastrostomy procedure.
- Ascertain the effectiveness of PEG in improving parameters usually associated with nutritional status and prognosis, including Body Mass Index (BMI), serum proteins and serum total cholesterol.
- Demonstrate the safety of PEG and its low complication rate.
Materials and methods
STUDY DESING
A single centre, observational, longitudinal and retrospective study was performed in a large hospital setting. This project was approved by the Ethic Committee of our hospital.
PATIENTS
We studied consecutive patients with ALS that were referred to the Enteral Feeding Team (GENE) of the Gastroenterology Department of Hospital Garcia de Orta from 2003 until 2015, underwent endoscopic gastrostomy to improve nutritional support and were followed at the Artificial Nutrition Outpatient Clinic.
The diagnosis of ALS was made according to the revised El Escorial criteria published by the World Federation of Neurology (16) and all patients were previously assessed by a neurologist. Only patients who fulfilled the revised El Escorial criteria for a definite ALS diagnosis were enrolled. The indications for gastrostomy were the presence of malnutrition defined by clinical, anthropometric and laboratory data, persistent moderate-severe dysphagia with chewing and swallowing compromise or at least one previous episode of aspiration pneumonia. Study exclusion criteria included diagnosis of other neurodegenerative diseases with motor impairment as well as patients with terminal ALS and an admission-estimated life expectancy less than one month. Patients under non-invasive ventilation were also not eligible for endoscopic gastrostomy.
Furthermore, all patients included had normal lung auscultation and peripheral oxygen saturation (> 90%). No severe respiratory compromise was evident despite pulmonary function tests were not routinely performed.
CLINICAL OUTCOME
According to the clinical outcome, patients were divided into three categories: alive and still PEG fed, deceased, and lost to follow-up. All the patients with unknown survival status were considered lost for follow-up. Time span from ALS diagnosis until the gastrostomy procedure and death (or until June 30th 2015) was rounded up to the nearest month. Reports of major complications were evaluated.
NUTRITIONAL RISK SCREENING 2002
NRS 2002 was performed in every patient as part of a systematic hospital routine.
ANTHROPOMETRIC EVALUATION
Anthropometric evaluation was performed, according with the ISAK manual of International Society for the Advancement of Kinanthropometry, just before the gastrostomy procedure (T0), between 8:00 and 10:00 AM. The average of three consecutive measurements was then recorded on the patients' file. The anthropometric evaluation was repeated three months later (T3) for surviving patients not lost to follow-up:
1. Body Mass Index (BMI) was obtained in most patients using the equation Weight/Height2. If patients were unable to easily stand up for weight and height evaluation, BMI was estimated using the Mid Upper Arm Circumference (MUAC) and regression equations described by -Powell-Tuck and Hennessy (17) which were previously been used and proved to provide a reliable BMI estimation in PEG feeding patients (20). Each patient was classified according to age: having low weight if BMI < 18.5 kg/m2 for patients under 65 years or BMI < 22 kg/m2 for patients 65 years old or older (19).
2. MUAC was measured in centimeters, using a flexible measuring tape wrapped around the mid upper arm, halfway between the olecranon and the acromion process.
LABORATORY EVALUATION
A blood sample for serum albumin, transferrin and total cholesterol was obtained minutes before endoscopic gastrostomy (T0), between 8:00 and 10:00 AM following at least 12 hours of fasting. The whole laboratory evaluation was repeated three months later (T3) for surviving patients not lost to follow-up. -Values of -albumin < 3.5 g/dL, transferrin < 200 mg/dL and total cholesterol < 160 mg/dL were considered low values, suggestive of malnutrition and/or poor prognosis.
STATISTICAL ANALYSIS
The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS®Inc., Chicago, IL), version 21, and Microsoft Office Excel Professional 2013®. The demographic variables analyzed in every patient were age, gender, time span from diagnosis until PEG, survival after diagnosis until death (or until June 30th 2015), and survival after PEG until death (or June 30th 2015).
The anthropometric and laboratory variables considered at T0 and T3 were: BMI, serum albumin, transferrin and total cholesterol levels.
After a descriptive analysis of all the variables, we applied a Student T Test with paired samples to compare the evolution of BMI, albumin, transferrin and cholesterol at the two moments, a Pearson Test to assess the correlation between those markers and patient survival, and a multivariate analysis using the ordinary least squares (OLS) regression model. Inferential tests were performed at the 5% level of statistical significance.
Results
PATIENTS
This study involved 37 ALS patients (18 men and 19 women) ranging from 43 to 88 years old (mean: 69 years; median: 71 years) that underwent PEG for nutritional support. Only 12 individuals were younger than 65 years. The demographic data of our sample are displayed in table I.
All patients had a definite ALS diagnosis according with the revised El Escorial criteria. The major indication for gastrostomy was established malnutrition or evidence of high nutritional risk associated with persistent moderate-severe dysphagia. All patients were previously assessed by a speech therapist with a large experience in swallowing evaluation who confirmed the aspiration risk. Nevertheless, none of the patients developed aspiration pneumonia.
Twenty-two patients presented with bulbar-onset symptoms and 15 with the spinal form of the disease. Time span from ALS diagnosis to gastrostomy ranged from zero to 49 months (mean: 11 months; median: 6.5 months) and did not differ between ALS bulbar and spinal form. Nine patients (24%) underwent PEG within the first month after diagnosis.
NUTRITIONAL RISK SCREENING 2002
NRS 2002 was performed in every patient as part of the hospital routine. NRS 2002 was ≥ 3 points in all patients, signalling high nutritional risk.
CLINICAL OUTCOME
By the end of June 2015, from the 37 included patients, 32 have died, two were alive and still PEG fed and three were lost to follow-up. It was possible to perform PEG in all referred patients with no major procedural complications.
Survival after PEG ranged from less than one month (two patients) to a maximum of 58 months. Mean survival after PEG insertion was 11.2 months (median: eight months). Mortality rate at three months was 21.6%. Mean survival after ALS diagnosis was 22.2 months (minimum two; maximum 64; median 18 months). Patient age was poor correlated with survival after ALS diagnosis until death (R = - 0.1, p = 0.46) and survival after PEG (R = - 0.1, p = 0.63). There were no differences in survival after diagnosis and survival after PEG between genders and the two presentation forms. A survival analysis after endoscopic gastrostomy using Kaplan Meier method is shown in figure 1.
No episodes of aspiration were documented after the gastrostomy procedure.
ANTHROPOMETRY
Regarding the 37 patients included in this study, we obtained BMI from 32 patients at admission (T0). In 26 patients, BMI was assessed using the equation weight/height2, and in the remaining six patients it was estimated using Powell-Tuck and Hennessy regression equations. At admission, BMI ranged from 16 to 33 (mean: 21.5; median: 21) and, adjusting to age, 15 patients displayed low BMI.
In the clinical assessment performed after three months of PEG feeding (T3) we recorded BMI data from 23 patients out of the initial 32. BMI values ranged from 14 to 31.5 (mean: 21.4; median: 21.3). Eleven patients displayed low BMI. However, eight patients died before the three months anthropometric evaluation and one was lost for follow-up.
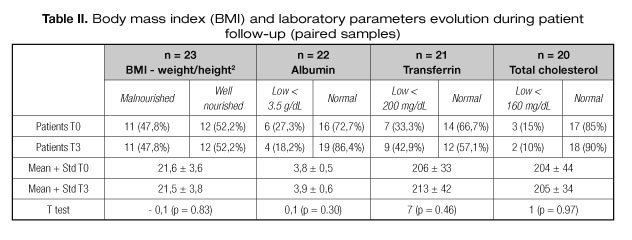
Among the patients for whom BMI evolution was known, the number of low BMI patients at T0 and T3 was similar. Using a Student T test with paired samples to compare means, BMI did not increase after three months of PEG feeding (IC95%: 21.6-21.5, p = 0.83) (Table II).
There was a positive correlation between BMI and survival (R = 0.3) that almost reached statistical significance (p = 0.06) (Fig. 2).
LABORATORY ASSESSMENT
At admission, serum albumin, transferrin and total cholesterol levels were recorded in 34, 30 and 34 patients, respectively: 12 displayed low albumin, 10 low transferrin and eight low total cholesterol.
At T3, serum albumin, transferrin and total cholesterol levels were obtained in 22, 21 and 20 patients, respectively. From these patients, three displayed low albumin, nine low transferrin and two low total cholesterol.
Analysing these data using a Student T test with paired samples to compare means we found that serum albumin (IC95%: 3.8-3.9, p = 0.30), transferrin (IC95%: 206-213, p = 0.46) and total cholesterol levels (IC95%: 204-205, p = 0.97) were slightly improved after 3 months of PEG feeding, but not reaching statistical significance (Table II).
Data from Pearson correlation test showed that high albumin (R = 0.3, p = 0.35) and transferrin (R = 0.4, p = 0.26) were positively correlated with longer survival in the group of patients who had low levels of these markers at admission, although not reaching statistical significance (Fig. 2).
There was no linear correlation between total cholesterol levels and survival after PEG (R = - 0.06; p = 0.89).
A multivariate analysis, using the ordinary least squares regression model (OLS), was also performed to assess the relationship between BMI, biochemical markers and patient survival. This approach revealed a positive impact of high initial BMI on survival (R2 = 0.39; p = 0.004). Data regarding albumin, transferrin and total cholesterol (p > 0.05) failed to achieve statistical significance.
Discussion
Neurological dysphagia, the most important cause of malnutrition in ALS, is a classical indication for endoscopic gastrostomy in this setting. Besides its potential negative impact on nutritional status, dysphagia raises other important concerns, such as predisposition to aspiration pneumonia and pneumonitis, frequent hospital admissions, accelerated functional decline, and overall poor prognosis (8,9).
ALS is a chronic, incurable, and inexorably progressive neurodegenerative disease (1). Because of the scarcity of disease modifying treatments, supportive measures, including nutritional status improvement, remain the mainstay of care in ALS. When these patients become malnourished and oral feeding is deemed unsafe, PEG can be placed in order to maintain hydration and muscle mass, avoid micronutrient deficiency, as well as prevent further complications associated with dysphagia (6,7).
For over a decade, a considerable number of ALS patients at high nutritional risk were referred to our centre. PEG placement for nutritional support was decided, according to the existing guidelines, taking into account the severity of dysphagia, and the patient's comorbidities and performance status. With the present study, we intended to assess the effectiveness and safety of PEG feeding, an efficient method of prolonged enteral nutrition in ALS patients.
Considering the small prevalence of the disease, its rapidly progressive nature and the fact that not all patients present with dysphagia or have indication for gastrostomy, we were still able to study an appreciable number of ALS patients for a single centre. Most of our patients were older adults with a slight female predominance. Survival after diagnosis ranged from two months to approximately five years, with a mean of almost two years. This high short-term mortality rate has been previously reported in literature. During the course of the disease our patients were gastrostomized, on average, 12 months after diagnosis, and survived around a year after the procedure. Mortality after gastrostomy was not negligible, with 21.6% of the patients dying within the first three months. Specific causes of death were not examined because most patients died outside the hospital and we could not access their death certificates. However, we admit probable development of respiratory failure caused by disease progression in most cases.
Several patients were referred to our department with established malnutrition, as defined by both anthropometric and laboratory parameters. We evaluated BMI on admission in most patients, since it is the anthropometric parameter most frequently used to assess nutritional status. However, between the two evaluations, mean BMI did not increase and the number of malnourished patients according with this parameter remained the same. We believe that, for ALS patients, three months may be a too short time period to achieve significant changes in weight, which requires protein synthesis and increased cell turnover in order to replenish metabolic reserves and improve muscle and fat mass. BMI changes may need a period longer than three months to become noticeable, which can be infeasible in this clinical setting.
Compared to the initial evaluation, fewer laboratory data were available at 3 months, chiefly because some patients did not survive or did not return for further assessment. Our results show that mean serum albumin, transferrin and total cholesterol increased slightly after 3 months of adequate PEG feeding. However, this difference was not statistically significant. This was probably due to the small number of patients that participated in both T0 and T3 laboratory evaluations. We conceive that PEG feeding may have a favourable biochemical effect and that a longer period using this approach can also have a positive anthropometric repercussion.
In addition, patients with higher serum proteins and/or higher BMI prior to gastrostomy appear to survive longer, though not significantly. The low Pearson correlation coefficients and high p-values obtained may again be attributed to the small sample size. However, when we performed a multivariate analysis we were able to verify that higher BMI significantly correlates with lower mortality, which supports the importance of maintaining good nutritional and physical status to improve prognosis.
No major procedural complications were observed in this study, confirming that, despite its (minimally) invasive nature, PEG is a safe procedure. Fear regarding patients' intolerance to the PEG procedure due to respiratory failure is common in ALS. Yet, it was possible to perform the technique without significant risks to our patients, as they did not have significant ventilatory compromise at admission. However, of note, pulmonary function was not routinely studied in all of our patients as most of them had severe malnutrition and considering that the alternative to feed this patients was a surgical gastrostomy (radiological guided gastrostomy is not performed in our institution) with much more risks in this disease we did not consider this tests essential. Furthermore, there are some studies showing that even with impaired respiratory function PEG could be made safely (14).
This study has some limitations. First, it is a retrospective study and the collected data is dependent on the accuracy of the clinical files. Second, we used a convenience sample, individuals were not randomized, and there was no control group to compare survival between patients that underwent PEG and those who did not. Randomization and blinding are virtually impossible in this clinical setting, as the PEG procedure must be individually debated with the patient and the caregivers. Third, despite the small number of patients lost to follow-up, several anthropometric and laboratory markers were not available at the 3 months evaluation, limiting the T0-T3 comparison. The sample is homogeneous in terms of indication for gastrostomy and dysphagia severity but its small size may be an important obstacle when trying to establish stronger conclusions. Lastly, serum albumin, transferrin and total cholesterol may also be influenced by multiple factors besides nutrition, as they are negative acute phase reactants.
Our results clearly show that established malnutrition prior to gastrostomy is associated with poor survival. PEG can successfully deal with the problem of dysphagia by maintaining the nutritional status and reducing the aspiration risk. The use of PEG in correcting malnutrition seems to be effective but needs to be confirmed in a larger and more representative sample. Nevertheless, our results suggest that early optimized nutritional support, while being associated with a decreased risk of aspiration and malnutrition, can possibly explain some cases of prolonged survival in our sample.
Conclusions
Dysphagia plays an important role in the development of malnutrition among ALS patients. From our experience in this study, PEG is a safe procedure in this clinical setting and that short-term survival after endoscopic gastrostomy is substantial, particularly when considering the poor overall survival after diagnosis. Higher BMI at admission clearly predicts a better outcome. PEG-feeding may avoid deterioration of nutritional status, but its effectiveness to correct established malnutrition, and improve BMI and other biochemical parameters needs to be confirmed in larger studies. Based on our results we recommend early enteral feeding through PEG in ALS patients with dysphagia considering that an early optimized nutritional status may contribute to longer survival.
Ethical aproval
All procedures performed were in accordance with the ethical standards of the institutional and/or national committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
1. Kiernan MC, Vucic S, Cheah BC, Turner MR, Eisen A, Hardiman O, et al. Amyotrophic lateral sclerosis. Lancet 2011;377(9769):942-55. DOI: 10.1016/S0140-6736(10)61156-7. [ Links ]
2. Logroscino G, Traynor BJ, Hardiman O, Chiò A, Mitchell D, Swingler RJ, et al. Incidence of amyotrophic lateral sclerosis in Europe. J Neurol Neurosurg Psychiatry 2010;81:385-90. [ Links ]
3. Tiryaki E, Horak HÁ. ALS and other motor neuron diseases. Continuum (Minneap Minn) 2014;20(5):1185-207. DOI: 10.1212/01.CON.0000455886.14298.a4. Review. [ Links ]
4. Shoesmith CL, Strong MJ. Amyotrophic lateral sclerosis. Update for family physicians. Can Fam Physician 2006;52:1562-69. [ Links ]
5. Desport JC, Preux PM, Magy L, Boirie Yves, Vallat JM, Beaufrère B, et al. Factors correlated with hypermetabolism in patients with amyotrophic lateral sclerosis. Am J Clin Nutr 2001;74:328-34. [ Links ]
6. Rosenfeld J, Ellis A. Nutrition and Dietary Supplements in Motor Neuron Disease. Phys Med Rehabil Clin N Am 2008;19(3):573-x. Doi:10.1016/j.pmr.2008.03.001. [ Links ]
7. Limousin N, Blasco H, Corcia P, Gordon PH, De Toffol B, Andres C, et al. Malnutrition at the time of diagnosis is associated with a shorter disease duration in ALS. J Neurol Sci 2010;297(1-2):36-9. DOI: 10.1016/j.jns.2010.06.028. [ Links ]
8. Oliveira ASB, Pereira RDB. Amyotrophic Lateral Sclerosis (ALS) Three letters that change the people's life for ever. Arq Neuropsiquiatr 2009;67:750-82. [ Links ]
9. Dorst J, Dupuis L, Petri S, Kollewe K, Abdulla S, Wolf J, et al. Percutaneous endoscopic gastrostomy in amyotrophic lateral sclerosis: a prospective observational study. J Neul 2015;4:849-58. DOI: 10.1007/s00415-015-7646-2. [ Links ]
10. Katzberg HD, Benatar M. Enteral tube feeding for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 2011;1:CD004030. DOI: 10.1002/14651858. [ Links ]
11. Loser Chr, Aschl G, Hébuterne X, Mathus-Vliegen EMH, Muscaritoli M, Niv Y, et al. ESPEN guidelines on artificial enteral nutrition - Percutaneous endoscopic gastrostomy (PEG). Clinical nutrition 2005;24:848-61. [ Links ]
12. Czell D, Bauer M, Binek J, Schoch OD, Weber M. Outcomes of percutaneous endoscopic gastrostomy tube insertion in respiratory impaired amyothophic lateral sclerosis patients under noninvasive ventilation. Respir Care 2013;58(5):838-44. DOI: 10.4187/respcare.02024. [ Links ]
13. Pena MJ, Ravasco P, Machado M, Pinto A, Pinto S, Rocha L, et al. What is the relevance of percutaneous endoscopic gastrostomy on the survival of patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2012;13(6):550-54. DOI: 10.3109/17482968.2012.684215. [ Links ]
14. Spataro R, Ficano L, Piccoli F, La Bella V. Percutaneous endoscopic gastrostomy in amyotrophic lateral sclerosis: effect on survival. J Neurol Sci 2011;304(1-2):44-8. DOI: 10.1016/j.jns.2011.02.016. [ Links ]
15. Miller RG, Rosenberg JA, Gelinas DF, Mitsumoto H, Newman D, Sufit R, et al. Practice Parametter: the care of the patient with amyotrophic lateral sclerosis (an evidence-based review): report of the quality standards subcommittee of the American Academy of Neurology: ALS Practice Parameters Task Force. Neurology 1999; 52(7):1311-23. [ Links ]
16. World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revisited criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Olther Motor Neuron Disord 2000;1(5):293-99. [ Links ]
17. Powell-Tuck J, Hennessy EMA. Comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin Nutr 2003;22(3):307-12. [ Links ]
18. Pereira M, Santos C, Fonseca J. Body Mass Index Estimation on Gastrostomy Patients Using the Mid Upper Arm Circunference. J Aging Res Clin Pract 2012;1:252-55. [ Links ]
19. American Academy of Family Physicians, American Dietetic Association, National Council on the aging. Nutrition Intervention Manual for Professionals Caring for Older Americans. Washington DC: Nutritional Screening Initiative: s.n.; 1992. [ Links ]
![]() Correspondence:
Correspondence:
Gonçalo Nunes.
Gastroenterology Department.
Hospital Garcia de Orta.
Av. Torrado da Silva, 2805-267.
Almada, Portugal
e-mail: goncalo.n@hotmail.com
Received: 23/02/2016
Accepted: 12/07/2016