Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.33 no.5 Madrid sep./oct. 2016
https://dx.doi.org/10.20960/nh.576
TRABAJO ORIGINAL / Valoración nutricional
Nutritional status and food intake of HCV/HIV coinfected patients
Evaluación del estado nutricional y de la ingesta de alimentos de los pacientes coinfectados por el HCV/HIV
Giselle Souza Pinto1, Anelise Fernanda Zanolla2, Cristiane Valle Tovo3,5, Catarina Bertaso Andreatta Gottschall4 and Caroline Buss2,4
1Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA).
2Postgraduate Study Program in Medicine: Hepatology.
3Clinical Department (Gastroenterology) and 4Nutrition Department. UFCSPA. Porto Alegre, Brazil.
5Hospital Nossa Senhora da Conceição. Porto Alegre, Brazil
ABSTRACT
Introduction: Hepatitis C virus (HCV) and human immunodeficiency virus (HIV) coinfection may cause nutrient deficiency and affect the nutritional status.
Objetive: To assess nutritional status, and energy and macronutrient intake in HCV/HIV coinfected patients.
Methods: Cross-sectional study on HIV/HCV-coinfected patients treated in a public hospital. Nutritional status was assessed by measurements of weight, height, waist circumference (WC), arm circumference (AC), triceps skinfold thickness (TST), non-dominant hand grip strength (NDHGS), body mass index (BMI) and mid-upper arm circumference (MUAC). Dietary intake was assessed by 24-hour recall.
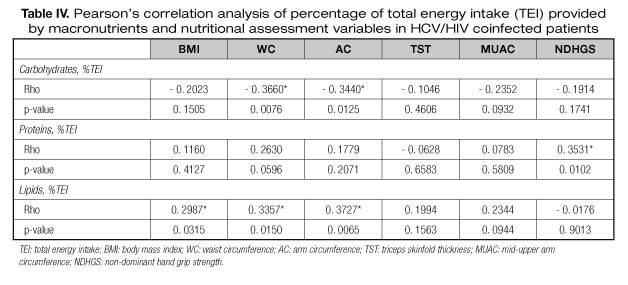
Results: Fifty-seven patients (59.6% women) with mean age of 46 ± 11.2 years were studied. According to BMI, more than half of patients were overweight or obese, and 41% of men and 68% of women had increased or substantially increased WC. The prevalence of malnutrition varied between the methods -10.5% (BMI), 29.8% (AC), 56.2% (TST), 17.6% (MUAC), and 12.3% (NDHGS). We found a high percentage of patients with inadequate intake of protein, fat and energy. The percentage of total energy intake (%TEI) from carbohydrates inversely correlated with WC and AC. A positive correlation was observed between %TEI from protein and NDHGS, and between %TEI from fat and BMI, WC and AC.
Conclusion: We found a high prevalence of increased body weight and WC, and inadequate dietary intake in HCV/HIV coinfected patients. We observed a positive association between protein intake and muscle function, and between fat intake and obesity.
Key words: HCV/HIV-coinfection. Nutritional status. Food consumption.
RESUMEN
Introducción: la coinfección con el virus de la hepatitis C (HCV) y el virus de la inmunodeficiencia humana (HIV) puede comprometer el estado nutricional y causar deficiencia de nutrientes.
Objetivo: evaluar el estado nutricional y la ingesta de energía y macronutrientes en pacientes coinfectados por el HCV/HIV (human immunodeficiency virus).
Métodos: estudio transversal con pacientes coinfectados por el HCV/HIV de un hospital público. El estado nutricional se evaluó por mediciones de peso, altura, circunferencia de la cintura (CC), circunferencia del brazo (CB), pliegue cutáneo del tríceps (DCT), fuerza de prensión mano no dominante (FAM), índice de masa corporal (IMC) y circunferencia muscular del brazo (CMB). La evaluación del consumo de alimentos se realizó mediante encuesta de recordatorio de 24 horas.
Resultados: se evaluaron 57 pacientes (59,6% mujeres) con una edad media de 46 ± 11,2. De acuerdo con el IMC, más de la mitad de los participantes eran obesos o con sobrepeso. Además, el 40,9% de los hombres y el 67,6% de las mujeres tenían CC aumentada. La prevalencia de desnutrición varió entre los métodos: IMC (10,5%), CB (29,8%), DCT (56,2%), CMB (17,6%), FAM (12,3%). Hubo un alto porcentaje de consumo insuficiente de proteínas, lípidos y energía. El porcentaje del valor energético total (%VET) de carbohidratos se asoció inversamente con las medidas de CC y CB. El %VET de proteínas se correlacionó positivamente con las medidas de FAM. El %VET de lípidos mostró una asociación positiva con el IMC, CC y CB.
Conclusión: se encontró una alta prevalencia del aumento de peso corporal y CC, y una ingesta dietética inadecuada. Se observó una asociación positiva entre la ingesta de proteínas y la función muscular, y entre la ingesta de grasa y la obesidad.
Palabras clave: Coinfección HCV/HIV. Estado nutricional. Consumo alimentício.
Introduction
Hepatitis C virus (HCV) and human immunodeficiency virus (HIV) coinfection is a public health problem, that may cause nutrient deficiencies and affect nutritional status (1,2). HIV infection may exacerbate the clinical manifestations of HCV, increase the risk for cirrhosis, liver failure and hepatocellular carcinoma, and hence worsen the prognosis of these patients due to higher morbidity and mortality (3).
Weight loss has been indicated as a marker of high risk for morbidity and mortality in HIV patients (4). Along with low food intake, it exacerbates energy-protein malnutrition and reduce life expectancy (5,6). Antiretroviral therapy (ART) has increased the life span among HIV-patients, although it has been associated with metabolic changes, including obesity, dyslipidemia, insulin resistance, hyperglycemia, and lipodystrophy, which are risk factors for cardiovascular diseases (7). In addition, the occurrence of some of these conditions, such as lipodystrophy may affect the diagnosis of the nutritional status.
Therefore, nutritional assessment is an important component of the ART, contributing to the management of obesity or malnutrition, and hence improving treatment tolerance and reducing the risk of opportunistic infections and cardiovascular diseases. The aim of the present study was to evaluate the nutritional status by different methods and assess energy and macronutrient intake in HCV/HIV patients.
Methods
This was a cross-sectional study using a convenience sample of HCV/HIV-coinfected patients, treated at the outpatient clinic of infectious diseases of a public hospital in the south of Brazil from August 2013 to June 2014.
Inclusion criteria were: HCV/HIV-coinfected patients, of both sexes, aged greater than 18 years. Diagnosis of hepatitis C and viremia were confirmed by the detection of anti-HCV antibodies and polymerase chain reaction, respectively. Diagnosis of HIV was confirmed according to the Ministry of Health ordinance no. 151 of 2009 (8). Exclusion criteria included patients in nutritional therapy, patients with cirrhosis, psychiatric disorders, neurological diseases (such as Alzheimer's and Parkinson's diseases), digestion and absorption disorders (including inflammatory bowel disease and celiac disease) or electrolyte disorder (e.g. edema and/or ascites), and pregnant and lactating women.
Patients answered a questionnaire on HIV therapy and sociodemographic data, including age, sex, educational attainment, marital status, and household income. Household income was classified according to the Brazilian Association of Research Companies criteria (9).
Nutritional status was assessed by measurements of body weight, height, triceps skinfold thickness (TST), arm circumference (AM), waist circumference (WC), non-dominant hand grip strength (NDHGS), body mass index (BMI) and mid-upper arm circumference (MUAC).
Body weight was measured to the nearest 0.1 kg using a digital scale (150 kg capacity), and height was measured using a portable stadiometer. BMI was calculated by dividing body weight (kilograms) by the square of the height (meters), and categorized using the World Health Organization (WHO) cut-off values for adults (10) and the classification proposed by Lipschitz (11) for elderly patients. WC was measured once using a flexible anthropometric tape at the midpoint between the iliac crest and the lowest rib, on the mid-axillary line, and classified according to WHO criteria (12). AC and TST were measured at the midpoint between the acromion and the olecranon. TST was measured according to the protocol by Harrison et al. (13), and MUAC was calculated from the AC and TST measures. Patients were classified by AC, TST and MUAC based on the standards described by Frisancho (14).
Muscle function was assessed by NDHGS using a dynamometer. The measurements were taken in triplicate at 1-minute intervals with patients in the sitting position and the elbow (of non-dominant arm) flexed at 90 degrees. Patients were classified according to the reference values proposed by Budziareck et al. (15).
Dietary intake was assessed by 24-hour food recall. Three 24-hour recalls were collected, including one weekend day or holiday as an atypical day. The first was conducted face-to-face, with the aid of pictures of food portions (16). The other two were collected by telephone, with a mean of 20 days between the interviews. The percentage of total energy intake from each macronutrient was calculated using the Avanutri® software (Avanutri Ltda).
The recommendation of macronutrient intake for HCV/HIV coninfected patients is not different from that for the general population, i.e. 50%-60% of total energy intake (TEI) from carbohydrates and 30-35% from lipids. The recommended daily intake of protein is 1.2g of protein/kg body weight during the stable phase of disease (6), and of energy is 25 kcal/kg/day for obese or overweight patients, 35 kcal/kg/day for normal weight and 40 kcal/kg/day for malnourished patients (6, 17).
Normally distributed data according to Shapiro-Wilk test (p > 0.05) were analyzed using parametric statistics. Continuous variables were described as mean ± standard deviation, and discrete variables, as absolute and relative frequency. Differences in nutritional status by sex were analyzed using the Pearson's Chi-square test. Correlations between data of dietary intake were analyzed using Spearman's rank correlation coefficient. Data processing and statistical analysis were performed using Microsoft Excel and the SPSS software version 19.0, respectively. A significance level of 0.05 was set for the analyses.
The study was approved by the Ethics Committee of Conceição Hospital Group in Porto Alegre, Brazil (protocol number 11-226), and all participants signed the informed consent form.
Results
Fifty-seven patients (59.6% women) with mean age of 46 ± 11.2 years were studied. All patients were receiving ART, and 35.2% belonged to social class D/E (Table I).
According to BMI, 37% of patients were overweight, and 17% obese. Forty-one percent of men and 68% of women (p=0.002) were at risk of obesity-related metabolic disorders according to WC measurement. The prevalence of malnutrition varied between the methods -10.5% (BMI), 29.8% (AC), 56.2% (TST), 17.6% (MUAC), and 12.3% (NDHGS) (Table II).
Daily energy intake was 100 kcal higher and 300 kcal lower than the mean recommended intake in men and women, respectively. The intake of fat and carbohydrate was higher than recommended values, but insufficient in protein in men, whereas in women, the intake of the three macronutrients was lower than recommendations (Table III).
Significant correlations were found between the percentage of TEI from carbohydrate, protein and fat and the variables of nutritional status (Table IV). The percentage of TEI from carbohydrate inversely correlated with WC (ρ = - 0.3660, p = 0.0076), and AC (ρ = - 0.3440, p = 0.0125). The percentage of TEI provided by protein positively correlated with NDHGS (ρ = 0.3531; p = 0.0102), and that provided by fat showed a positive correlation with BMI ρ = 0.2987; p = 0.0315), WC (ρ = 0.3357; p = 0.0150) and AC (ρ = 0.3727; p = 0.0065). The intake of protein (in g of protein/kg body weight/day) inversely correlated with TST (ρ = - 0.3168, p = 0.0221) and positively correlated with MUAC values ρ = 0.3175, p = 0.0218).
Discussion
The present study identified a high prevalence of overweight and obesity in HCV/HIV coinfected patients. This finding is in agreement with the studies by Jame et al. (18) and Ladeira and Silva (19), which reported a prevalence of 30.5% and 32.5%, of overweight, respectively, in HIV patients. These results may be related to inadequate dietary intake, currently observed in the western culture, characterized by high consumption of saturated fat and refined sugar. In addition, chronic use of ART may cause several side effects, such as lipodystrophy and metabolic syndrome (20).
The high prevalence of malnutrition detected by TST measures and abdominal obesity by WC suggests the occurrence of lipodystrophy, which is commonly observed among HIV patients using ART, and is an important risk factor for noncommunicable diseases (20). In the study by Ladeira and Silva (19), WC was used as an indicator of abdominal fat accumulation, which was higher among women than men, similarly to our results. Also, the study found a predisposition of HIV patients to cardiovascular disease. Others have suggested that WC is associated with obesity-related adverse effects in these patients (21).
The prevalences of malnutrition detected by AC (30%) and MUAC (18%) measurements in our study were different from those found by Paim (22), who reported higher prevalence of malnutrition (51% by AC and 58% by MUAC) in HCV/HIV coinfected patients. However, since we studied HCV/HIV patients in the stable stage of disease and receiving ART, we would expect a relatively lower prevalence of malnutrition and a greater number of obese and overweight patients.
In addition, we also detected a 12.3% prevalence of malnutrition using hand grip strength. This relatively low percentage may also be related to disease stability and lack of complications related to coinfection. We did not find other studies on nutritional assessment using this method in HCV/HIV patients. However, hand grip strength was indicated as the most sensitive method for diagnosing malnutrition in HCV cirrhotic patients by another study conducted in Brazil (23).
It is worth mentioning that different methods of nutritional assessment, such as triceps skinfold thickness (TST) and mid-upper arm circumference (MUAC) measure different body components. TST, for example, indirectly evaluates energy fat stores, whereas MUAC assesses muscle mass. The presence of lipodystrophy may affect these measurements, due to a reduction in energy stores on upper limbs and increase of abdominal adiposity. Therefore, the rates of malnutrition should be interpreted with caution in patients receiving ART. Also, we believe that hand grip strength should be included in the nutritional assessment and follow-up of HCV/HIV patients, since it is a functional measure of the nutritional status, not affected by the ART.
With respect to energy and macronutrient intake, although the mean intake of the study group was near the recommended values, we found a high percentage of patients with inadequate intake, especially among women. This result may be related to the occurrence of obesity, overweight and even malnutrition. A study by Carreira and Pereira (24) on the nutritional status of HCV patients, showed a direct relationship between excessive weight and fat intake. This result is in accordance with our findings, which showed a correlation between the intake of this macronutrient and BMI, WC and AC. Therefore, a lipid-rich diet is related to energy storage, which is important in cases of malnutrition, but a risk factor for obesity and overweight in this population.
Protein intake was associated with higher values of NDHGS, suggesting an inverse relationship between the intake of this macronutrient and malnutrition. Protein metabolism disorders have been associated with chronic liver disease, due to a reduction in hepatic function and increased catabolism. Low protein intake can cause malnutrition, which is related to higher mortality index (6).
There were a number of limitations which should also be noted. We used the 24-hour food recall to assess dietary intake, which is a method that relies on subjects' memory (25). Also, the administration of the instrument by telephone may affect the reliability of the results due to the difficulty in estimating portion size (26). However, previous studies have shown that 24-hour dietary recall can be conducted successfully both face-to-face or over the phone (27-29).
Conclusion
In the present study on HCV/HIV coinfected patients, altered nutritional status was detected in these patients, with high prevalence of overweight, obesity and increased WC, and inadequate intake of macronutrients and energy. Protein intake was directly related to muscle function, whereas excessive fat intake was related to high obesity rates in this population.
Different malnutrition indexes were found according to the method of assessment employed. Due to lipodystrophy caution should be taken in interpreting results of anthropometrical indexes in clinical practice and functional measures should be taken into consideration in individual assessments.
References
1. Dietitians of Canada. Hepatitis C: nutrition care Canadian guidelines for health care providers. Can J Diet Pract Res 2003;64:139-41. [ Links ]
2. Food and Agriculture Organization/World Health Organization. Living well with HIV/AIDS - A manual on nutritional care and support for people living with HIV/AIDS; 2002. [ Links ]
3. Puoti M, Bruno R, Soriano V, Donato F, Gaeta GB, Quinzan GP. Hepatocellular carcinoma in HIV-infected patients: epidemiological features, clinical presentation and outcome. AIDS 2004;18:2285-93. [ Links ]
4. Barbosa RMR, Fornés NS. Avaliação nutricional em pacientes infectados pelo vírus da imunodeficiência adquirida. Rev Nutr 2003;16:461-70. [ Links ]
5. Dutra CNN, Basso C. Alterações nutricionais em portadores de hepatite C. Disc Scientia 2006;7:109-20. [ Links ]
6. Waitzberg DL. Nutrição oral, enteral e parenteral na prática clínica. 4.a ed. São Paulo: Atheneu; 2009. [ Links ]
7. Smith DK, Hanson DL, Graham NH, Flynn M, Greenberg B, Sowell Ding A. Nutritional status and is behavioral and clinical correlates in the hers cohort of HIV infected and at-risk uninfected women. International Conference on Aids; 1996. [ Links ]
8. Brasil. Ministério da Saúde. Portaria N.o 151, de 14 de outubro de 2009. Bvsms.saude 2009. [ Links ]
9. Associação Brasileira de Empresas de Pesquisa. Critério de Classificação Econômica Brasil. São Paulo; 2012. http://www.abep.org/criterioBrasil (acessado em 06/ago/2014). [ Links ]
10. World Health Organization. Technical report series - Physical status: the use and interpretation of anthropometry. Geneva: Wolrd Health Organization; 2005. [ Links ]
11. Lipschitz DA. Screening for nutritional status in the elderly. Prim Care 1994;21:55-67. [ Links ]
12. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. Geneva; 2000. [ Links ]
13. Frisancho AR. Anthropometric standards: an interactive nutritional reference of body size and body composition for children and adults. 4.a ed. University of Michigan Press; 2011. [ Links ]
14. Harrison GC. Skinfold thickness and measurement technique. In: Anthropometric standardization reference manual. Champaing: Human Kinetics, 1988. p. 55-80. [ Links ]
15. Budziareck MB; Duarte PRR; Barbosa-Silva MC. Reference values and determinants for handgrip strength in healthy subjects. Clin Nutr 2008;27:357-62. [ Links ]
16. Vitolo MR. Pesos e volumes de alimentos e medidas caseiras, 1.a ed. In: Nutrição: da gestação ao envelhecimento. Rio de Janeiro: Rubio; 2008. p. 594-611. [ Links ]
17. Cuppari L. Guia de nutrição: nutrição clínica no adulto. 2.a ed. Barueri: Manole; 2005. [ Links ]
18. Jaime PC, Florindo AA, Latorre MRDO, Brasil BG, Santos ECM, Segurado AAC. Prevalência de sobrepeso e obesidade abdominal em indivíduos portadores de HIV/AIDS, em uso de terapia antiretroviral de alta potência. Rev bras epidemiol 2004;7:8. [ Links ]
19. Ladeira P, Silva DC. Estado nutricional e perfil alimentar de pacientes assistidos pelo programa de DST/Aids e hepatites virais de um Centro de Saúde de Itaperuna-RJ. DST J bras doenças sex transm 2012;24:28-31. [ Links ]
20. Filho AC, Abrão P. Alterações metabólicas do paciente infectado por HIV. Arq Bras Endocrinol Metab 2007;51:5-7. [ Links ]
21. Rami Bailony M, Scherzer R, Huhn G, Plankey MW, Peters MG, Phyllis CT. Association of HIV Infection, Hepatitis C Virus Infection, and Metabolic Factors With Liver Stiffness Measured by Transient Elastography. J Infect Dis 2013;208:1776-83. [ Links ]
22. Paim APAC. Estado nutricional e estadiamento histológico de pacientes mono ou coinfectados com os vírus da hepatite C e HIV (dissertation). (Bahia): Universidade Federal da Bahia; 2011. p. 97. [ Links ]
23. Gottschall CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Avaliação nutricional de pacientes com cirrose pelo vírus da hepatite C: a aplicação da calorimetria indireta. Arq Gastroenterol 2004;41:220-24. [ Links ]
24. Carreira CM, Pereira PCM. Perfil nutricional e dietético de indivíduos com hepatite C. Semina cienc biol saude 2011;32:143-54. [ Links ]
25. Willet WC. Nutritional epidemiology. New York: Oxford University Press; 1998. [ Links ]
26. Fisberg R, Martini L, Slater B. Métodos de inquéritos alimentares. In: Fisberg R, Slater B, Marchioni D, et al. Inquéritos alimentares: métodos e bases científicos São Paulo: Manole; 2005. [ Links ]
27. Monteiro C, Moura E, Jaime P, et al. Validity of food and beverage intake data obtained by telephone survey. Rev Saude Publica 2008;42:582-9. [ Links ]
28. Matarazzo H, Marchioni D, Figueiredo R, et al. Reprodutibilidade e validade do questionário de frequência de consumo alimentar utilizado em estudo caso-controle de câncer oral. Rev Bras Epidemiologia 2006;9:316-24. [ Links ]
29. Moshfegh A, Rhodes D, Baer D. The US Department of Agriculture Automated Multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324-32. [ Links ]
![]() Correspondence:
Correspondence:
Cristiane Valle Tovo.
Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA).
Rua Sarmento Leite, 245.
CEP 90050-170, Porto Alegre. RS, Brasil
e-mail: cris.tovo@terra.com.br
Received: 24/01/2016
Accepted: 26/05/2016