My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Nutrición Hospitalaria
On-line version ISSN 1699-5198Print version ISSN 0212-1611
Nutr. Hosp. vol.34 n.6 Madrid Nov./Dec. 2017
https://dx.doi.org/10.20960/nh.1059
Waist-to-height ratio and its relation with cardiometabolic risk factors in children from Bucaramanga, Colombia
Relación cintura-estatura y su relación con factores de riesgo cardiometabólico en niños de Bucaramanga, Colombia
Edna Magaly Gamboa-Delgado1, Clara Lucía Domínguez-Urrego2 and Doris Cristina Quintero-Lesmes3
1Escuela de Nutrición y Dietética. Universidad Industrial de Santander-UIS. Bucaramanga, Colombia.
2Unión Temporal Cardiecol (Conocimiento y acción para reducir la dimensión de la enfermedad cardiovascular en Colombia). Universidad Autónoma de Bucaramanga-UNAB. Floridablanca, Colombia.
3Fundación Cardiovascular de Colombia. Grupo de Estudios Epidemiológicos y de Salud Pública-FCV. Bucaramanga, Colombia
Funding: Project partially subsidized by Colciencias contract 376-2011.
ABSTRACT
Background: Currently, the waist-to-height ratio (WHtR) has emerged as a practical and useful indicator for identifying cardiometabolic risk in child and adolescent population.
Objective: To evaluate the association between the WHtR and cardiometabolic risk factors (CMRFs) in a cohort of children in Bucaramanga, Colombia.
Methods: Analytical cross-sectional study. Child population between 6-10 years old from Bucaramanga (n = 1,282). Dependent variables: hypertension, pre-hypertension, overweight/obesity, impaired glucose, insulin resistance and dyslipidemia. Main independent variable: waist-to-height ratio. The association between dependent and independent variables was evaluated using binomial regression models.
Results: 9.77% of the children presented a WHtR of risk (95% CI: 8.19% to 11.52%). After adjustment for age, sex, socioeconomic status and physical activity, the WHtR of risk was significantly associated with lower HDL levels and higher levels of triglycerides, insulin resistance, hypertension and pre-hypertension (PR = 2.46 95% CI :1.70 a 3.55, p = 0.000, PR = 2.24 95% CI: 1.50 a 3.35, p = 0.000, PR = 9.39 95% CI: 5.40 a 16.30, p = 0.000, PR = 8.03 95% CI: 2.01 a 32.07, p = 0.003 y PR = 2.67 95% CI: 1.60 a 4.47, p = 0.000, respectively).
Conclusion: Children with WHtR of risk were more likely to develop high levels of blood pressure and triglycerides, insulin resistance and lower levels of HDL.
Key words: Child. Metabolic syndrome X. Waist-height ratio.
RESUMEN
Introducción: en la actualidad, el índice de cintura-talla (ICT) ha emergido como un indicador práctico y útil en la detección del riesgo cardiometabólico en población infantil y adolescente.
Objetivo: evaluar la asociación entre el índice de cintura-talla y los factores de riesgo cardiometabólicos (FRCM) en una cohorte de niños de Bucaramanga, Colombia.
Metodología: estudio de corte transversal analítico anidado en una cohorte poblacional. Población infantil entre 6-10 años de Bucaramanga (n = 1.282). Variables dependientes: hipertensión arterial, pre-hipertensión arterial, sobrepeso/obesidad, glucosa alterada, resistencia a la insulina, y dislipidemia. Principal variable independiente: índice cintura-talla. La asociación entre variables dependientes y las independientes fue evaluada mediante modelos de regresión binomial.
Resultados: el 9,77% de los niños presentó un índice cintura-talla de riesgo (IC 95%: 8,19% a 11,52%). Al ajustar por edad, sexo, nivel socio económico y actividad física, el índice cintura-talla de riesgo resultó asociado significativamente con menores niveles de HDL y mayores niveles de triglicéridos, resistencia a la insulina, hipertensión arterial y prehipertensión (RP = 2,46 IC 95%: 1,70 a 3,55, p = 0,000, RP = 2,24 IC 95%: 1,50 a 3,35, p = 0,000, RP = 9,39 IC 95%: 5,40 a 16,30, p = 0,000, RP = 8,03 IC 95%: 2,01 a 32,07, p = 0,003 y RP = 2,67 IC 95%: 1,60 a 4,47, p = 0,000, respectivamente).
Conclusión: los niños con un índice de cintura-talla de riesgo presentaron mayor probabilidad de desarrollar niveles elevados de presión arterial y triglicéridos, resistencia a la insulina y menores niveles de HDL.
Palabras clave: Niño. Síndrome X metabólico. Índice cintura-talla.
INTRODUCTION
Preliminary studies applied to a young and adult population, support the clinical utility of the waist-to-Height Ratio (WHtR) in the early characterization of cardiometabolic risk. This anthropometric index is practical, simple to calculate and its results interpretation do not require age or sex specifications. In children populations, the body mass index (BMI) is widely used as an anthropometric index, commonly known for its sensitivity and moderate specificity when detecting the adiposity excess in children, as well as its variability, fastened to this population's development and annual growth change patterns (1,2).
The WHtR arises as an indicator with multiple advantages, some of which can be useful for clinical use; its application has a simple results interpretation, thus WHtR values are not correlated with the characteristic development and growth constant changes on infant and adolescent population (3,4), which strengthens its utility by early detections of obesity and cardiometabolic risk. Additionally, the WHtR indicates the regional body fat distribution through central adiposity or intra-abdominal measurement, which is broadly recognized as an important factor associated to metabolic comorbidity and cardiovascular complications, such as hypertension, dyslipidemia, disorders of glucose metabolism and insulin resistance (5-7). Some authors suggest that children and adolescents with a WHtR ≥ 0.5 increase the probability of having more than two cardiometabolic risk factors (8,9), leading to the development of cardiovascular diseases during adulthood.
Overall, the cardiometabolic profile alterations are known as metabolic syndrome (MS), whose diagnostic criteria are widely used in children and adolescent studies, introduced by Cook et al., which establishes the relation between three or more criteria by age and sex for MS (fasting glucose levels, triglycerides, HDL-c, systolic/diastolic blood pressure and waist circumference). Nevertheless, standardization and consensus of cardiometabolic marker cut-off points for this population remains a challenge that requires further exploration, which, to be clarified, will provide an adequate representative MS patterns characterization in early stages of life.
Regarding the proposed interpretation of metabolic and cardiovascular risk given by the WHtR cut-off point, nowadays, the international scientific community accepts a ≥ 0.5 value as an indicator of an increased risk, however, this result in the child and adolescent population is still in discussion. Some studies support the cut-off point established before (5,8-13), while other authors report different values in children and adolescents of diverse populations (1,14-16,18), whose values are slightly below or above to the previously described.
Therefore, the present study aims to determine the association between the WHtR and the cardiometabolic risk factors (CMRFs) in children between 6 to 10 years old in Bucaramanga, Colombia.
METHODS
Design: analytical cross-sectional study sheltered in a cohort of population type.
Population and sample: the study population includes 1282 children aged from 6 to 10 years' old who reside in XXX. They belong to a population cohort study that evaluates the prevalence of MS and its related factors. Currently, this population is being analyzed by the original study, which is looking for new relations between MS diagnostic criteria and the early onset cardiometabolic dysfunction in the youth population.
Study variables: this study's main dependent variables related to cardiometabolic factors are defined as follows: hypertension: (systolic blood pressure (SBP) or diastolic (DBP) ≥ 95 percentile for age, gender and size measured 3 or more times). Pre-hypertension: SBP or DBP ≥ 90 percentile < 95 percentile for age, gender and height (19). Overweight or obesity: overweight: BMI for age between percentile 85% and 95%. Obesity: ≥ 95 percentile BMI for age (20). Impaired fasting glucose: ≥ 100, diabetes: ≥ 126 mg/dL (21). HOMA-IR: was obtained from the mathematical model using the next formula: (22.5/[IF*GF]), where IF stands for the insulin fasting levels in UL/L and GF for the glucose fasting levels. HOMA-IR cut-off point was ≥ 3.2 (22). Dyslipidemia: a) impaired triglycerides: 0-9 years: ≥ 100 mg/dL HDL cholesterol alterations: < 40 mg/dL; and b) LDL cholesterol alterations: ≥ 130 mg/dL (23).
This study's main independent variable is WHtR, which it's been calculated from the height measurement and waist circumference in centimeters. Additionally, the following criteria will be considered variables such as: Sociodemographic variables: sex, age, socioeconomic level and breastfeeding length. Anthropometric variables: sex, height, BMI, waist circumference, hip circumference, moderate-intensity physical activity, screen time and breastfeeding length.
Data collection: this process was conducted for 16 months (from July 2006 to October 2007), where a home visit to collect information was held, regarding sociodemographic, nutritional and physical activity variables, and a second visit for a full clinical assessment and a laboratory sample taking by Fundación Cardiovascular de Colombia. Physical activity was assessed by using the International Physical Activity Questionnaire (IPAQ) (24,25) asking the time (hours per day) the children spent doing several activities such as sleeping, studying, doing moderate physical activity, vigorous physical activities and spending in front of screens during one day of the week and the weekend.
The data collection activity was carried out by health professionals previously trained by the study investigators.
Data quality: the data quality was revisited to ensure that the information was complete. The data input by duplicate was made in Excel (Microsoft Corp., Redmond, Wash.) and were compared using the Epi-Info 2000. All discrepancies in the two databases were corrected using the original formats of data capture.
Statistical analysis: a descriptive analysis was made in which categorical variables were presented as proportions and the continuous variables as mean and standard deviation, or median and interquartile range, according to the distribution shown. If the continuous variables had a normal distribution, the differences were determined using the Student t test; otherwise, the Mann Whitney U test. The independent variable association from this study and the dependent variables were assessed using binomial regression models. In multivariate models, the variables obtained a p < 0.20 in the bivariate analysis. All p values were considered two-tailed, considering statistical significance at a p < 0.05. All data were analyzed in the statistical program Stata, version 12.0 (College Station, TX: Stata Corporation).
Ethical considerations: this study was designed in compliance with the Helsinki declaration and approved by the Ethical Committee in Research from Fundación Cardiovascular de Colombia. A full consent was given from the participant parents or caregivers. In addition, all children gave their verbal assent.
For a more detailed methodology review, may refer to the published cohort study protocol (26).
RESULTS
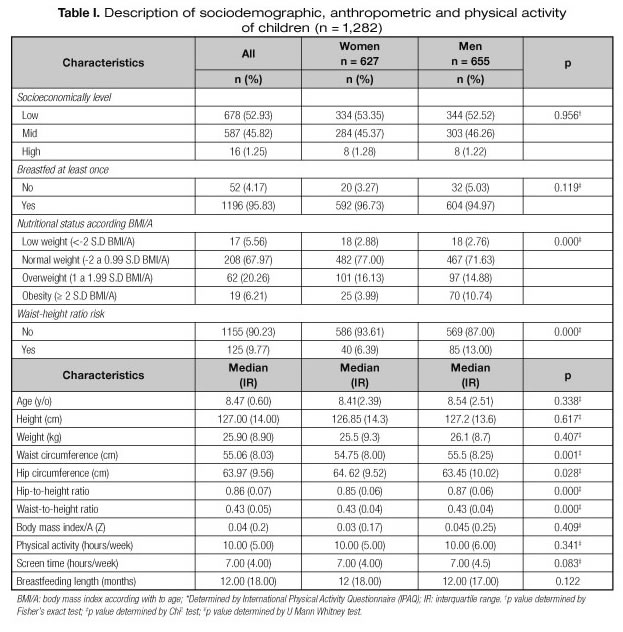
The analytical sample was taken from a population of 1282 children, most of them belonging to mid and low socioeconomic levels (Table I). According to risk factors related with the behaviors, 6.81% is not engaged in a moderate physical activity and 62.64% does not performs high intensity activities, fact that contrasts with 41.58% of the children who spend 8 or more hours a week in front of screens (such as TV, videogames and tablets). In addition, 1.56% (n = 20) acclaimed to have smoked at least once -average starting age: 9 years old, standard deviation (SD) 1.41 years old- and 49.34% said they had consumed alcohol in the previous years.
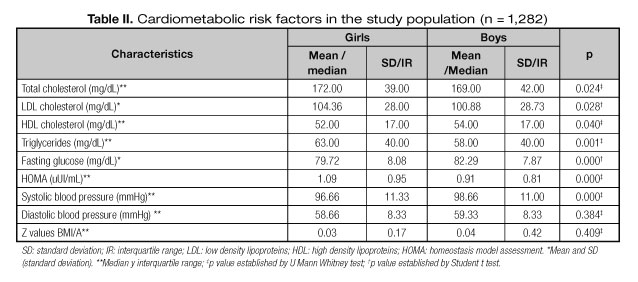
In respect to the CMRFs, the overweight or obesity prevalence was 26.47% (95% CI 23.22% to 27.84%). Concerning dyslipidemia, it shows upper levels of LDL cholesterol in a 17.24% (95% CI 15.20% to 19.41%) and low HDL cholesterol in 11.31% (95% CI 9.62% to 13.17%), high triglycerides levels in a 10.37% (95 %CI 8.75% to 12.17%). As for the blood pressure component, 0.70% of the sample presented hypertension (95% CI: 0.32% to 1.30%) and 6.13% (95% CI 4.87% to 7.58%) pre-hypertension. Likewise, it was found out a prevalence of 1.01% (95% CI 0.54% to 1.72%) in impaired fasting glucose and 2.74% (95% CI 1.91% to 3.79%) of insulin resistance.
The prevalence of CMRFs, according to the sex, is shown in figure 1. Male children had higher fasting glucose levels, HDL-c and systolic blood pressure (p = 0.000, p = 0.040, p = 0.000, respectively), while female children had higher triglycerides, LDL-c and insulin resistance levels (p = 0.01, p = 0.028, p = 0.000, respectively) (Table II).
Concerning the WHtR, 9.77% of the sample, exposed a WHtR ≥ 0.5 (95% IC: 8.19% 11.52%). The WHtR median was 0.43, Interquartile range (0.05).
After adjusting by age, sex, socioeconomic level and physical activity, WHtR ≥ 0.5 was mainly associated with lower HDL-c levels and higher triglycerides levels, insulin resistance, hypertension and pre-hypertension in the population study (Table III).
DISCUSSION
This analytical cross-sectional study, nested in a population cohort study, shows that WHtR uses as an anthropometric marker associated with CMRFs: lower HDL-c levels, higher levels of triglycerides, insulin resistance, hypertension and pre-hypertension, in the study population. These findings are consistent with preliminary and recent studies performed by the pediatric population around the world (12,27).
Overweight and obesity were identified in this study as the CMRFs with greater prevalence in children (26.47%), which is consistent with Suarez et al., with 18% prevalence in a 5-9-years-old population (17). The abdominal and general obesity represents an increase of cardiometabolic risk profile in infant population, which directly implies the cardiovascular happenings and diabetes mellitus type II in adulthood (8,9,28). Currently, this condition is widely recognized as a major issue in public health matters, which has been in increasing in the child population in recent decades, with figures ranging from 8.1% to 12.9% in male children and from 8.4% to 13.4% in female children by 2013 in developing countries (29).
Regarding to WHtR in this study, 9.7% of the analyzed children displayed a cut-off point ≥ 0.5 for the anthropometric index. This value is consistent with Mokha et al., who reported a prevalence of 9.2% in children with normal weight versus a 19.8% of children with overweight/obesity, whose WHtR cut-off point was ≥ 0.5. Likewise, after adjusting by age, sex, socioeconomic level and physical activity, the findings in this research suggest the increase of 9 times the risk of suffering insulin resistance and 8 times of contracting hypertension among the presence of a WHtR ≥ 0.5.
In relation with the last aspect, preliminary studies suggest the insulin resistance occurs as one of the early age alterations that benefit the hypertension development in infant population (12,30-32). According to Correia-Costa et al., insulin resistance had an important mediating effect in arterial pressure increase at expense of systolic pressure, with greater visibility in female subjects, attributed by the authors to the composition changes and body fat distribution occurred before women puberty, as well as some pathophysiological mechanisms such as hyperleptinemia and leptin resistance (31). Understanding the relationship between insulin resistance and hypertension requires a deeper study of these mechanisms involving other cardiometabolic risk profile variables in this population. Unlike to these associations, glucose levels did not represent a strong correlation in relation with WHtR in this study, which is similar to what reported Kuba et al., attributing to this situation the incipient manifestation of insulin resistance in 6-10-year-olds (12).
With respect to the lipid profile alterations, the results evidenced in this population demonstrated a significant correlation between WHtR and higher levels of triglycerides and lower levels of HDL-c, with an increased risk between 2.60 and 2.95 times, respectively. Similar results have been reported by other authors in pediatric populations. Mokha et al., identified an increased risk of 1.47 and 1.66 times to have significantly elevated levels in triglycerides and LDL-c, as well of 2.01 times to have significantly lower levels in HDL-c in children with WHtR ≥ 0.5 (8). In contrast to the associations mentioned above, this study did not identify a significant relationship between the LDL-c levels and WHtR, which is also part of the findings of a recent study in a Latin-American child population where LDL-c showed a weak correlation with WHtR, even in the unfixed analysis (33).
In comparison with the studies in adolescents, the association between WHtR and CMRFs are maintained for this population. In this sense, Graves et al., reported a prospective association between the WHtR ≥ 0.5 observed in childhood and increased chances of getting 3 or 4 CMRFs during adolescence, with an increase of 4.6 times in men (95% IC: 2.6 to 8) and 1.6 (95% IC: 0.7 to 3.9) in women (9). Likewise, Nambiar et al. reported a positive correlation between WHtR and insulin resistance observed in female adolescents (32), in the same way as in Mexican adolescent population (1), whose results showed a strong correlation between WHtR and higher pressure levels and insulin resistance in females.
With regard to the WHtR cut-off point interpretation for early detection of cardiometabolic risk profile in children population, a WHtR cut-off point ≥ 0.5 has been proposed as a cardiovascular and metabolic disorders risk predictor, which does not depend of other variables for the result interpretation in different populations. However, some authors have questioned the applicability of this cut-off point as a universal indicator of CMRFs, arguing some significant differences observed amongst sex, races and ages (1,14,15,34). On the contrary, other studies have not found significant differences in their populations (8-13), attributing this characteristic to the division between waist circumference and height, which minimizes these differences (5). For this study purposes, the proposed cut-off point was the most used and accepted by the scientific community, with which the associations described above were obtained, demonstrating their predictive value detection in cardiometabolic risk profile at early ages.
Finally, in relation with risk factors behavior, our study identified a high prevalence (69.45%) of children who do not exercise, compared to 41.58% of children who spend their time in front of screens. As reported by the third National Health and Nutrition Examination Survey (NHANES) (35), children who spend more than 4 hours in front of the TV screen have higher levels of adiposity. Also, this sedentary behavior has been considered one of the main factors that contribute to infant and adolescent obesity in the first-world population (36,37). Accessibility to new technology tools amongst children, could eventually become a contributing factor of sedentarism in these children and the development of risk factors such as obesity and metabolic disorders.
The limitations of this study concern the nature of its cross-sectional type design which prevents the inference of temporality. Although significant associations were found between values of WHtR ≥ 0.5 and some CMRFs. These findings do not suggest any causality.
As strengths of this study, it's important to highlight the rigorous data collection process with properly trained professionals as well as data quality through double fingering, supervision and validation of errors.
Overall, the findings identified in this study support the relationship between WHtR ≥ 0.5 and low levels of HDL-c, high triglycerides levels, insulin resistance and hypertension/pre-hypertension. In addition, the measurement of WHtR has proven to be a low cost and easy tool to use and whose benefits can bring significant changes in the cardiovascular diseases management and its mortality impact. Therefore, the evidence from this study suggest the usefulness of this indicator in children as a predictor of CMRFs and early intervention, as well as building strategies in public health oriented by sex, and aimed to prevent cardiovascular events in adulthood.
CONCLUSION
Children with a waist-to-height ratio ≥ 0.5 presented a higher probability of developing upper levels in arterial pressure and triglycerides, insulin resistance and lower levels of HDL. It is necessary to implement cardiometabolic risk prevention strategies addressed to the child and adolescent population.
REFERENCES
1. Rodea-Montero ER, Evia-Viscarra ML, Apolinar-Jiménez E. Waist-to-Height Ratio Is a Better Anthropometric Index than Waist Circumference and BMI in Predicting Metabolic Syndrome among Obese Mexican Adolescents. Int J Endocrinol 2014;2014:195407.
2. Semiz S, Ozgoren E, Sabir N, Semiz E. Body fat distribution in childhood obesity: association with metabolic risk factors. Indian Pediatr 2008;45(6):457-62.
3. Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr 2005;56:303-7.
4. Arnaiz P, Grob F, Cavada G, Domínguez A, Bancalari R, Cerda V, et al. Waist-to-height ratio does not change with gender, age and pubertal stage in elementary school children. Rev Med Chil 2014;142(5):574-8.
5. Maffeis C, Banzato C, Talamini G. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr 2008;152(2):207-13.
6. Casazza K, Dulin-Keita A, Gower BA, Fernandez JR. Intrabdominal fat is related to metabolic risk factors in Hispanic Americans, African Americans and in girls. Acta Paediatr 2009;98(12):1965-71.
7. Cruz ML, Bergman RN, Goran MI. Unique effect of visceral fat on insulin sensitivity in obese Hispanic children with a family history of type 2 diabetes. Diabetes Care 2002;25(9):1631-6.
8. Mokha JS, Srinivasan SR, Dasmahapatra P, Fernandez C, Chen W, Xu J, et al. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: The Bogalusa Heart Study. BMC Pediatr 2010;10:73.
9. Graves L, Garnett SP, Cowell CT, Baur LA, Ness A, Sattar N, et al. Waist-to-height ratio and cardiometabolic risk factors in adolescence: findings from a prospective birth cohort. Pediatr Obes 2014;9(5):327-38.
10. Khoury M1, Manlhiot C, McCrindle BW. Role of the waist/height ratio in the cardiometabolic risk assessment of children classified by body mass index. J Am Coll Cardiol 2013;20;62(8):742-51.
11. Wu XY, Hu CL, Wan YH, Su PY, Xing C, Qi XY, et al. Higher waist-to-height ratio and waist circumference are predictive of metabolic syndrome and elevated serum alanine aminotransferase in adolescents and young adults in mainland China. Public Health 2012;126(2):135-42.
12. Kuba VM, Leone C, Damiani D. Is waist-to-height ratio a useful indicator of cardio-metabolic risk in 6-10-year-old children? BMC Pediatr 2013;13:91.
13. Benmohammed K, Valensi P, Benlatreche M, Nguyen MT, Benmohammed F, Pariès J, et al. Anthropometric markers for detection of the metabolic syndrome in adolescents. Diabetes Metab 2015;41(2):138-44.
14. Zhou D, Yang M, Yuan ZP, Zhang DD, Liang L, Wang CL, et al. Waist-to-Height Ratio: a simple, effective and practical screening tool for childhood obesity and metabolic syndrome. Prev Med 2014;67:35-40.
15. Matsha TE, Kengne AP, Yako YY, Hon GM, Hassan MS, Erasmus RT. Optimal waist-to-height ratio values for cardiometabolic risk screening in an ethnically diverse sample of South African urban and rural school boys and girls. PLoS One 2013;13;8(8):e71133.
16. Santoro N, Amato A, Grandone A, Brienza C, Savarese P, Tartaglione N, et al. Predicting metabolic syndrome in obese children and adolescents: look, measure and ask. Obes Facts 2013;6(1):48-56.
17. Suarez-Ortegón MF, Aguilar-de Plata C. Prevalence of metabolic syndrome in children aged 5-9 years from southwest colombia: a cross-sectional study. World J Pediatr 2016;12(4):477-83.
18. Sardinha LB, Santos DA, Silva AM, Grøntved A, Andersen LB, Ekelund U. A Comparison between BMI, Waist Circumference, and Waist-To-Height Ratio for Identifying Cardio-Metabolic Risk in Children and Adolescents. PLoS One 2016;11(2):e0149351.
19. The Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents. National Heart, Lung and Blood Institute, NHI. USA; 2005.
20. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. National Heart, Lung and Blood Institute, NHI. USA; 2012.
21. Standards of Medical Care in Diabetes. ADA; 2016
22. Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C. Homeostasis Model Assessment Is More Reliable Than the Fasting Glucose/Insulin Ratio and Quantitative Insulin Sensitivity Check Index for Assessing Insulin Resistance Among Obese Children and Adolescents". Pediatrics 2005;115(4): e500-e503.
23. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. National Heart, Lung and Blood Institute, NHI. USA; 2012.
24. International Physical Activity Questionnaire-Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - Short and long forms. 2005. (Cited 2017 Mar 22). Available at: http://goo.gl/39feCk.
25. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35(8):1381-95.
26. Villa-Roel C, Buitrago A, Rodríguez DC, Cano DJ, Martínez MP, Camacho PA. Prevalence of metabolic syndrome in scholars from Bucaramanga, Colombia: a population-based study. BMC Pediatr 2009;9:28.
27. Chung IH, Park S, Park MJ, Yoo EG. Waist-to-Height Ratio as an Index for Cardiometabolic Risk in Adolescents: Results from the 1998-2008 KNHANES. Yonsei Med J 2016;57(3):658-63.
28. Hara M, Saitou E, Iwata F, Okada T, Harada K. Waist-to-height ratio is the best predictor of cardiovascular disease risk factors in Japanese schoolchildren. J Atheroscler Thromb 2002;9(3):127-32.
29. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384(9945):766-81.
30. Chen W, Srinivasan SR, Elkasabany A, Berenson GS. Cardiovascular risk factors clustering features of insulin resistance syndrome (Syndrome X) in a biracial (Black-White) population of children, adolescents, and young adults: The Bogalusa Heart Study. Am J Epidemiol 1999;150(7):667-74.
31. Correia-Costa L, Santos AC, Severo M, Guerra A, Schaefer F, Caldas Afonso A, et al. Sex-Specific Mediating Role of Insulin Resistance and Inflammation in the Effect of Adiposity on Blood Pressure of Prepubertal Children. PLoS One 2015;10(6):e0132097.
32. Nambiar S, Truby H, Davies PS, Baxter K. Use of the waist-height ratio to predict metabolic syndrome in obese children and adolescents. J Paediatr Child Health 2013;49(4):E281-7.
33. Agredo-Zúñiga RA, Aguilar-de Plata C, Suárez-Ortegón MF. Waist: height ratio, waist circumference and metabolic syndrome abnormalities in Colombian schooled adolescents: a multivariate analysis considering located adiposity. Br J Nutr 2015;114(5):700-5.
34. Kruger HS, Faber M, Schutte AE, Ellis SM. A proposed cut-off point of waist-to-height ratio for metabolic risk in African township adolescents. Nutrition 2013;29(3):502-7.
35. National Health and Nutrition Examination Survey. Anthropometry procedure manual. 2000. (Updated May 2013). Available at: http://www.cdc.gov/nchs/data/nhanes/bm.pdf
36. Deheeger M, Rolland-Cachera MF, Fontvieille AM. Physical activity and body composition in 10 year old French children: linkages with nutritional intake? Int J Obes Relat Metab Disord 1997;21(5):372-9.
37. DeLany JP, Harsha DW, Kime JC, Kumler J, Melancon L, Bray GA. Energy expenditure in lean and obese prepubertal children. Obes Res 1995;3(Suppl 1):67-72.
 Correspondence:
Correspondence:
Doris Cristina Quintero Lesmes.
Fundación Cardiovascular de Colombia.
Calle 155A No. 23-58. Urbanización El Bosque.
Oficina Diseño y Desarrollo.
Bucaramanga, Colombia
e-mail: dorisquintero@fcv.org / dorisuql@gmail.com
Received: 21/02/2017
Accepted: 06/08/2017