My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Nutrición Hospitalaria
On-line version ISSN 1699-5198Print version ISSN 0212-1611
Nutr. Hosp. vol.34 n.6 Madrid Nov./Dec. 2017
https://dx.doi.org/10.20960/nh.1151
Nutritional and neuropsychological profile of the executive functions on binge eating disorder in obese adults
Perfil nutricional y neuropsicológico de las funciones ejecutivas en el transtorno por atracón en adultos obesos
Mariana Ermel Córdova, Cecilia Cesa Schiavon, Fernanda Michielin Busnello and Caroline Tozzi Reppold
Federal University of Health Sciences of Porto Alegre. Porto Alegre, Brasil
ABSTRACT
Objective: To examine the relationships between obese patients with and without binge eating disorder (BED) and the neuropsychological profiles of their executive functions.
Methods: Data from 36 obese individuals (BMI ≥ 30 kg/m2) were divided into two groups, where one group was found to be positive for signs of BED according to the Binge Eating Scale. Two neuropsychological tests of executive function were carried out: the Go/No-go Task and the Iowa Gambling Task (IGT). Nutritional status was evaluated by measures of body weight, height and abdominal circumference, and from these, body mass indexes (BMI) were calculated.
Results: Both groups presented similar nutritional characteristics; there were no differences when it came to the health status of individuals with or without BED. Participants found positive for signs of BED had the lowest IGT scores (p = 0.004), and Go/No-go omission scores (p = 0.015) and commission scores (p = 0.04). Further statistically significant differences were also observed here between the two groups. Statistical differences in the IGT results correlated with BED, and were associated categorically (p = 0.005).
Conclusion: Obese individuals frequently present deficits in selective attention, inhibitory control, decision-making and planning that can be directly related to binge eating and which is linked to BED. Nutritional status did not differ between the two groups studied, and did not show any connection with the disorder.
Key words: Binge eating disorder. Executive function. Neuropsychology. Obesity. Nutritional status.
RESUMEN
Objetivo: examinar las relaciones entre los pacientes obesos con y sin trastorno por atracón (TA) y los perfiles neuropsicológicos de sus funciones ejecutivas.
Métodos: los datos de 36 individuos obesos (IMC ≥ 30 kg/m2) se dividieron en dos grupos, donde se encontró que un grupo era positivo para los signos de BED de acuerdo con la escala de Binge Eating Scale. Se realizaron dos pruebas neuropsicológicas de la función ejecutiva: la Tarea Ir/No-ir y la Tarea de Juego de Iowa (IGT). El estado nutricional fue evaluado por medidas de peso corporal, estatura y circunferencia abdominal, y de estos se calcularon los índices de masa corporal (IMC).
Resultados: ambos grupos presentaron características nutricionales similares; No hubo diferencias en cuanto al estado de salud de las personas con o sin BED. Los participantes encontraron positivos para los signos de BED que tuvieron los puntajes IGT más bajos (p = 0,004), y puntuaciones de omisión IR/No-ir (p = 0,015) y comisiones (p = 0,04). Otras diferencias estadísticamente significativas también se observaron aquí entre los dos grupos. Las diferencias estadísticas en los resultados IGT se correlacionaron con BED, y se asociaron categóricamente (p = 0,005).
Conclusión: los individuos obesos frecuentemente presentan deficiencias en la atención selectiva, el control inhibitorio, la toma de decisiones y la planificación que pueden estar directamente relacionados con el atracón y que está relacionado con la BED. El estado nutricional no difirió entre los dos grupos estudiados, y no mostró ninguna relación con el trastorno.
Palabras clave: Trastorno binge eating. Función ejecutiva. Neuropsicología. Obesidad. Valor nutricional.
INTRODUCTION
Binge eating disorder (BED) was recently added as a diagnostic category among eating disorders (EDs) in the Diagnostic and Statistical Manual of Mental Disorders - Fifth Edition/DSM-V (1). Binge eating is the concept applied to the unbridled and excessive ingestion of large quantities of food, known as binge eating episodes, in which the act is obtainable and uncontrollable. Patients with BED are more likely to respond to situations that cause emotional tension by consuming food. In this process, a person allows him/herself to transgress by means of eating in a manner that could be justified physiologically with cortisol that, released during stressful situations, stimulates food intake and results in weight increase (2).
Patients with BED generally have among the highest rates of dissatisfaction with their own body image; their desired weight and their actual weight are relatively distant and, therefore, they have greater difficulty forming holding realistic expectations about treatment (3). In addition, they feel unable to control their food intake (4) and present an accentuated oscillation in relation to their original weight (5,6). From a clinical perspective, these individuals frequently present a nutritional status of overweight or obese. Bulik et al. explained that obese individuals with BED tend to have more health problems as a whole, and, significantly, demonstrate dissatisfaction with this (7).
A study published in 2013 assessed 24,124 participants from 14 countries, including countries from Latin America, the United States and Europe. Data showed that the prevalence of BED in the general population was 1.9% (8). However, in medical treatments for overweight and obese individuals, the prevalence may vary between 7.5% and 30% (9,10). Regarding prevalence among the gender, BED affected 3.5% of women and 2% of men (11), which indicates a relatively more diverse population when compared to other eating disorders (EDs). It is especially important to emphasize, however, that approximately 20% of people report that they have binge eating, while in fact, the diagnosis of BED is necessarily performed by healthcare professionals (12,13).
Different ED rates have been linked to certain types of deficits in executive function (EF), though this topic is relatively new and sometimes controversial. Studies show that obsessive/compulsive individuals present low competence in planning activities and organizational strategies (14,15), which reflects on EF deficits. Therefore, once BED is related to binge eating episodes, and as it is the main criteria for diagnosis, it plays a significant role in the development and maintenance of obesity and eating disorders.
EF, according to Malloy-Diniz et al. (2007), consists of a set of cognitive processes that, together, enable individuals to direct their behaviors and goals, evaluate the appropriateness of these behaviors, abandon ineffective strategies in favor of other more effective ones, and thereby solve problems (16). It turns out that for a task to be performed coherently and fully, it is necessary for individuals to know exactly what their ultimate goals are, and that they choose goal-directed behaviors to make achieving these goals possible. An organizational hierarchy is required for this to work properly, in which the effectiveness and efficiency of each behavior is constantly evaluated in order to alter the unsuccessful ones and to choose new strategies to replace those that have failed. Concomitantly, individuals must remain focused on performing these behaviors and on their ultimate goals (17).
Multiple components are involved in EF to enable the formation of a coherent plan of action, to strive for and ultimately achieve a goal, and to adjust behaviors along the way (18). EF components are discussed by different authors from different perspectives to define what their functions are. Most important among these are operating or working memory, inhibitory control (selecting the most appropriate behavioral response to a situation while inhibiting others), selective attention or vigilance, planning, organizational questioning, mood, self-regulation, creativity, problem solving, decision-making, fluency, categorization, prioritizing and cognitive flexibility (16,17,19,20).
Inhibitory control is fundamental to avoiding binge eating episodes because difficulties related to this are usually associated with impulsiveness. However, selective attention corresponds to a set of processes that lead to the selection or prioritization of certain categories of information (21,22).
The objective of this study was to assess the nutritional and neuropsychological profile of obese patients with BED in comparison with the control group, while considering the relationship between BED and EF in particular. Analysis included assessing elements of EF (specifically: selective attention, inhibitory control, decision making and planning) and tracing the groups' nutritional profiles by means of anthropometric and laboratory assessments.
METHOD
Participants
Thirty-six obese individuals (BMI ≥ 30 kg/m2) were recruited for the study and divided into two groups of 18 participants each. One group contained individuals that tested positive for signs of BED according to the Binge Eating Scale (BES), and the other group contained those without BED. The participants were interviewed in the Metabolic Nutrition Clinic associated with the Endocrinology Department of a large hospital in the city of Porto Alegre in southern Brazil. Exclusion criteria were: less than six years of schooling, a history of brain injury, neurological disorders potentially (such as epilepsy or clinical diseases, which could have had an impact on their eating behavior or nutritional state).
ZThe sample size was calculated with Programs for Epidemiologists (PEPI) version 4.0, based on a pilot study of 10 patients in each group. Significance level of 5%, a power of 80%, a minimal difference between the groups of 24 points with standard deviation of 24 points, and with these a minimum total of 17 individuals in each group was obtained.
Instruments
Case histories
Cases histories were compiled with participants' data from school and employment records, clinical history, age and socioeconomic status. All information was collected at the time of the interview. Employment data were categorized into: paid work, student, retired or unemployed. Clinical history was categorized into: not having associated pathologies, having two or more, or having only one condition associated with obesity.
Signs of BED
A version of the Binge Eating Scale (BES), translated and adapted for Brazil, was used for tracking BED (23). This instrument was developed to evaluate the severity of binge eating in obese subjects. The range comprises 16 items for assessing behavioral manifestations, feelings and cognition involved in compulsive episodes. Results were divided into three categories: serious binge eating (scores ≥ 27), moderate (scores between 18 and 26) and absence of binge eating (scores ≤ 17). This study included patients with BED who achieved a score between moderate and serious binge eating.
Neuropsychological assessment of EF
Iowa Gambling Task (IGT)
This task assesses decision making and planning skills in a real-life simulation (24). A version translated into Portuguese (25) was presented to the participants, in which four virtual piles of cards appear on a computer screen which participants can select from. According to the players card choice, he/she will be ether rewarded fictitious money or, alternative "bed card", will cause to lose money. Players have to pay attention and select cards assessing the best cost-benefit ratios. The IGT scores are categorized into five blocks (S1 to S5) according to the scores obtained in the first 20 games (S1), in 20 subsequent games (S2), and so on.
Go/No-go Task
To evaluate the EF elements of selective attention and inhibitory control, we used the Go/No-go Task (26-28). In this task several letters flashed on a computer screen each second, in different colors, and the participants were instructed to react quickly by pressing the "space" bar for all letters, except for those which had been previously identified as part of the exclusion set. The test provided measures for task errors and reaction times, which are positively correlated with selective attention and inhibitory control.
Nutritional assessment
Anthropometric assessment
Body weights, heights and abdominal circumferences (ACs) were measured, and body mass indexes (BMIs) were subsequently calculated [BMI = weight (kg)/height2 (m2)]. Cut-off points established by the World Health Organization (WHO) (2000) were used for the AC measurements (29).
Biochemical examinations
Biochemical tests were done on participants' blood samples to analyze glucose, triglycerides, total cholesterol, low density lipoprotein (LDL), high density lipoprotein (HDL) and glycemic exposure (HbA1c). These included liquid chromatography HPLC (HbA1c), automated enzyme analysis (glucose, cholesterol, triglycerides and HDL) and the Friedewald equation (LDL).
Procedure
The study was approved under opinion number 1,733/12 issued by the Ethics Committee of the ISCMPA. All participants signed an informed consent agreement. The instruments were applied individually in the Metabolic Nutrition clinic over the course of one 45-minute session for each participant. In these sessions, the BES was applied along with neuropsychological assessment instruments (IGT and Go/No-go Task), and weight, height and AC were measured. Biochemical data were collected from patient records six month period prior to these sessions.
Statistical analysis
A descriptive analysis of the results was conducted employing frequency, percentages and standard deviation. To verify the associations between variables we used the Pearson Chi-square test and, when necessary, the Fisher's exact test, with the additional resource of standardized residue analysis adjusted to identify the location of associations.
RESULTS
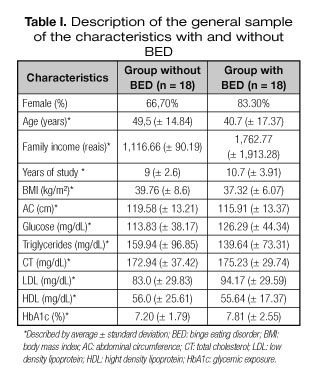
Both groups have similar characteristics, which demonstrates that the samples are homogeneous, as table I shows. This uniformity is observed between the groups, both in the nutritional status of the participants (BMI, AC and laboratory exams) and in variables related to gender, age, household income, education and occupation. The average BES score was 26.77 points; 55.6% were classified as serious binge eaters.
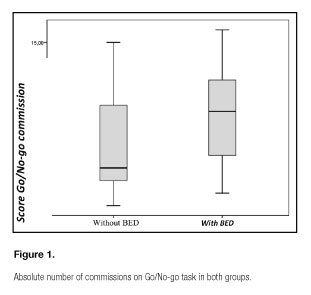
The Go/No-go Task was assessed according to the number of omissions and commissions the participants scored.
Individuals who had higher BES scores, representing a greater severity of pathology, had lower scores in the Go/No-go Task for the omission portion (rs = -0.565; p = 0.015). Therefore, participants who failed to react in a timely or correct manner in the task also demonstrated more severe instances of eating disorder. When assessing the number of commissions, significantly higher scores were found in the group of participants with BED (SD = 9.5) when compared to participants without BED (SD = 5). Thus, different median scores were obtained for the two groups (p = 0.04), as is described in figure 1. It can be stated that the participants in this study with BED tended to respond by pressing the keyboard when presented with any visual stimuli, supporting the possibility that selective attention deficit is associated with BED in the Go/No-go Task.
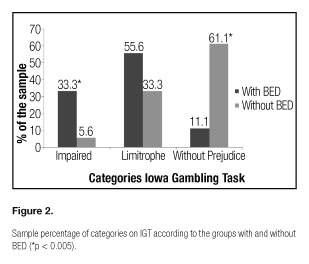
In the IGT, final scores also presented differences between the two groups. The group without BED obtained an average score of 18.55 (SD = 22.48), whereas the group with BED reached an average score of -5.66 (SD = 25.13), showing that participants with the disorder obtained lower numbers when assessed for decision-making and planning. It is significant that, even with a high standard deviation, the groups are significantly different statistically (p = 0.004).
The results of the IGT were evaluated and separated into categories classified as either impaired (scores < 18), borderline (scores between 18 and -18), and unimpaired (scores > -18) (30). Statistically significant results were obtained (p = 0.005). Figure 2 shows that, in the group with BED, more participants presented impaired outcomes on the IGT when compared to those in the control group. These results were obtained despite the fact that the group without BED presented a greater sampling of unimpaired participants according to the IGT scores.
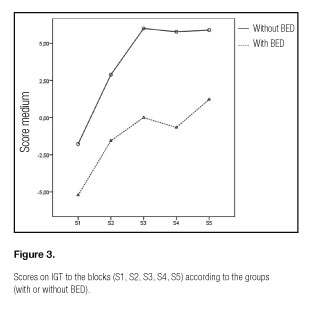
The IGT blocks (there are five blocks of twenty rounds each: S1, S2, S3, S4 and S5), which are intended to determine whether learning occurred during the task (31), demonstrated no significant difference among them. However, as can be seen in figure 3, the group of participants without BED presented lower scores in the first block (p = 0.004).
In assessing the relationship between BMI and IGT performance in both groups, it is apparent that IGT scores generally decrease as BMI increases, though this relationship is not statistically significant (p = 0.079). However, when evaluating the group of participants without BED, a significant degree of association (rs = -0.534; p = 0.023) with BMI was observed in the final IGT block. This does not appear to occur in the group with BED, which, as seen figure 4, demonstrates a borderline association (rs = -0.319; p = 0.197).
DISCUSSION
In assessing the comparison between the two groups' neuropsychological profiles as determined in EF tasks, it can been seen in this study that patients who presented positive signs of BED, according to the BES, presented lower scores on the IGT and the Go/No-go task. Thus, it can be assumed that most obese individuals with BED have selective attention deficits and deficient inhibitory control, decision-making and planning when compared to those without the disorder.
Both groups showed similar characteristics in terms of average body weight, BMI, AC and results from biochemical laboratory tests. Thus, one can characterize the populations in this study as homogeneous regarding nutritional state. However, differences are found in relevant literature in which BED has been associated with increased health risks regardless of nutritional status (7). The present study corroborates this idea, that there are increased health risks associated with BED that are independent from nutritional status. Diseases associated with heath risk, which are commonly reported in cases of patients with obesity and BED (7) were also observed in this study, in which 44.4% had two or more endocrine diseases such as heart problems and diabetes mellitus. The variables of gender, age, household income, education and occupation were also similar in both groups. Most patients were female, which is consistent with findings in the literature (11).
Participants' score on the BES was inversely proportional to the number of omissions on the Go/No-go Task. Thus, the greater the severity of the disorder, the lower the scores in terms of omissions (rs = -0.565; p = 0.015). This relationship characterizes selective attention deficit since these patients could not pay attention to the tasks they were given. As selective attention is a set of processes that leads to selecting or prioritization in the processing of certain categories of information (21), the fact that subjects did not press a computer key in response to visual stimuli indicates that there is a mental deficit associated with task orientation and concentration. A study published in 2012 supports these findings, where 42 participants who had or had had anorexia nervosa (NA) at some point in their lives showed signs of selective attention deficits when evaluated with the Test of Variables of Attention (TOVA) (32). Further literature suggested that participants present deficits when confronted with challenging environments. With several sources of information competing for their attention, participants demonstrated difficulty in maintaining focus (17).
However, Galioto et al. evaluated selective attention with tests like Backward Digit Span, Visual Memory Span, Switching of Attention - Digits and Verbal Interference - Word, with a sample very similar to that of our study, and obtained different results. The author compared the cognitive function of 131 patients with morbid obesity and a former or current history of BED, together with controls, and concluded that both groups had high rates of cognitive deficit. However, there was no significant difference between them, just as there was no difference between those diagnosed with BED in the past and those currently diagnosed (33). This study by Galioto et al. suggests that there is some sort of remaining deficit that can be shown in patients who tested positive for BED in the past.
The commission scores in the Go/No-go Task were significantly higher in participants with BED (MD = 9.5) when compared to participants without BED (MD = 5), and median scores between the groups (p = 0.04) were obtained. Considering that patients with eating disorders frequently demonstrate anxiety behaviors (34) and impulsiveness (3), the methodology employed in this study can point to a possible relationship between keyboard responses and item investigated. According to the study by Mobbs et al., inhibitory control, attention and mental flexibility were considered the most important functions in controlling binge eating episodes, which in turn play a role in the development and maintenance of obesity and eating disorders (35). In 2011, a study evaluated these functions in obese patients with BED, without BED and people with normal weight, and concluded that obese participants had significantly more errors of commission (pressing keys in response to any stimulus) and more errors of omission (not pressing keys when a target was visible) than those in the control group. In addition, the study showed that obese participants with BED had significantly more errors and omissions that those without the disorder (35). The results from Mobbs et al. are consistent with the present study, in which obese patients presented deficits in general inhibitory control and difficulty in relation to selective attention. Another paper evaluated the EF in 106 women after an eating disorders study and noted that 30% of participants had impaired performance in one or more tests. This deficit was associated with anxiety in these participants. The authors then concluded that not only are eating disorders associated with EF, but also that states of anxiety seem to contribute to deficits in these functions (36).
However, according to the performance of participants with eating disorders in EF tests, the literature is inconsistent. At the end of 2010, researchers analyzed EF, including inhibitory control, categorization of hypotheses, planning, problem solving, task scheduling capacity, working memory and cognitive flexibility using various neuropsychological tests in 38 obese participants with BED in comparison with obese participants without the disorder. The performance of obese participants with BED did not differ significantly from those without BED when assessed for inhibitory control. However, research published in 2013 found different results when investigating inhibitory control (with the Stop Signal Task, SST) and decision-making (with Game of Dice Task, GDT) in patients with bulimia, with BED and in the control group. People with BED showed no significant differences from controls on the tests applied (p= 0.078 on SST and p = 0.058 on GDT). However, bulimic participants had a higher rate of inactivity in the SST when compared to the control group (p = 0.002), showing that these patients have a higher degree of impulsivity. Nevertheless, they showed no significant difference in relation to decision-making on the GDT (p = 0.034) (37).
Analyzing the decision-making and planning functions, as evaluated through the IGT, in this study it has been seen that the groups present significant differences (p = 0.004) on the final score. This suggests that a pattern of disadvantageous choices (which lead to immediate gains and significant long-term losses) can be associated with a specific pattern of impulsivity or deficits in ability regarding the consequences of short, medium and long term planning (16). Decision-making skills are directly related to unplanned impulses. In order to successfully make decisions in a task, individuals must analyze alternatives and consider factors such as cost/benefit, social and moral aspects, and self-awareness.
A meaningful statistically result (p = 0.005) can be seen in assessing IGT by category (impaired, borderline and unimpaired) in which the group with BED had worse outcomes than the control group, while also presenting greater sampling with the absence of deficits in the test. In 2010, a group of German researchers obtained quite similar results by comparing two groups (17 obese women with BED and 18 without the disorder) via GDT to evaluate risky decision-making, inhibition of behavior and focus, and cognitive flexibility. The authors concluded that women with BED are significantly more likely to make risky decisions when compared to the control group. Moreover, they have an impaired ability to use feedback as an auxiliary mechanism (38). Although the relationship of learning in the IGT was not significant between the groups, in this study participants with BED presented lower scores in the first block (p = 0.004).
A study published in 2012 by a group from the Netherlands also obtained results similar to those of the present study regarding decision-making in female participants with BED when compared to controls (containing obese participants without BED and also participants of normal weight). Via the IGT and questionnaires measuring self-control, the severity of binge eating and sensitivity to punishment and reward, the authors were able to conclude that obese participants and those with BED had underperformed on the IGT, and did not improve their responses throughout the task. However, participants of normal weight demonstrated learning throughout the task (39). Another study that used the IGT to measure decision making in participants with eating disorders, though (anorexia in this case) concluded that this particular group demonstrated a deficient performance on the task in comparison with a control group and with a group of participants who had already had anorexia at another time in their lives. It has been noted that participants who have already had anorexia nervosa at some time in their past do not show results like this in the test (40). This result suggests that after an eating disorder is overcome, deficits in EF are no longer significant.
In relation to learning during the IGT task, the group of participants without BED showed lower scores in the first block of tasks (p = 0.004). However, it has been found through empirical observation that normal individuals and those with neuropsychiatric pathologies tend to demonstrate similar performances in the first instances of the test. However, subjects free of pathology tend to have performances characterized by choices that lead to long-term gains throughout the test. On the other hand, patients with disorders tend to maintain a pattern of short-term choices, characterized by larger gains in the short term and a successive accumulation of long-term losses.
CONCLUSION
Obese patients with BED showed deficits in EF inhibitory control, selective attention, decision making and planning when compared to the control group. There is a good theoretical basis supporting deficient neuropsychological profiles in EF regarding selective attention and inhibitory control, which are consistent with the relationship between binge eating episodes and eating disorders, of which BED is one.
Regarding nutritional profile, both groups showed similar characteristics, which showed that there is no difference as to the state of health and/or nutritional state of individuals with and without BED. According to this study, BED itself is not conducive to the emergence of new pathologies (as a reflection of obesity itself).
Some results may have suffered limitations because of the research sample, which could better elucidate the characteristics of BED if the population were more heterogeneous in schooling and income. One should also consider the possibility of bias in EF testing due the limited education of the participants. Moreover, for better results, more tests are recommended for assessing EF and the neuropsychological profiles of patients.
This new diagnostic category has shown very specific pathological characteristics, making it necessary to conduct new studies in order to verify the relationships between disorders and neuropsychological profiles. Thus, based on these opportunities, it is expected that support for the appropriate treatment of this disorder will be found in future neuropsychological and nutritional studies.
REFERENCES
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5.a ed. Washington (DC): American Psychiatric Association; 2013.
2. Gluck M, Geliebter A, Satov T. Night eating syndrome is associated with depression, low self-esteem, reduced daytime hunger, and less weight loss in obese outpatients. Obes Res 2001; 9(4):264-7.
3. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4ª ed. Washington (DC): American Psychiatric Association; 2000.
4. Spitzer RL, Yanovski SZ, Wadden T, Wing R, Marcus MD, Stunkard A, et al. Binge eating disorder: its further validation in a multisite study. Int J Eat Disord 1993;13(2):137-53.
5. Borges MB, Jorge MR, Morgan CM, da Silveira DX, Custódio O. Binge-eating disorder in Brazilian women on a weight-loss program. Obes Res 2002;10:1127-1134.
6. Costa RF, Machado SC, Cordás TA. Imagem corporal e comportamento sexual de mulheres obesas com e sem transtorno da compulsão alimentar periódica. Rev Psiquiatr Clin 2010;37:27-31.
7. Bulik CM, Sullivan PF, Kendler KS. Genetic and environmental contributions to obesity and binge eating. Int J Eat Disord 2003;33(3):293-8.
8. Kessler RC, Bergulund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry 2013;73(9):904-14.
9. Ricca V, Mannucci E, Moretti S, Di Bernardo M, Zucchi T, Cabras PL, et. al. Screening for binge eating disorder in obese outpatients. Compr Psychiatry 2000;41(2):111-115.
10. De Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metabol Disord 2001;25(Suppl 1):S51-55.
11. Hudson JI, Hiripi E, Popo HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;61:348-358.
12. Stunkard AJ, Allison KC. Two forms of disordered eating in obesity: binge eating and night eating. Int J Obes Relat Metab Disord 2003;27:1-12.
13. Napolitano MA, Head S, Babyak MA, Blumenthal JA. Binge eating disorder and night eating syndrome: psychological and behavioral characteristics. Int J Eat Disord 2001;30(2):193-203.
14. Fontenelle L. Aspectos neuropsicológicos do transtorno obsessivo-compulsivo. Rev Bras Psiquiatr 2001;23(Supl 2):27-30.
15. Penadés R, Catalán R, Andrés S, Salamero M, Gastó C. Executive function and nonverbal memory in obsessive-compulsive disorder. Psychiatric Res 2005;133:81-90.
16. Malloy-Diniz LF, Bentes RC, Figueiredo PM, Brandão-Bretas D, Costa-Abrantes S, Parizzi AM, et al. Normalización de una batería de tests para evaluar las habilidades de comprensión del lenguaje, fluidez verbal y denominación en niños brasileños de 7 a 10 años: resultados preliminares. Rev Neurol 2007;44(5):275-280.
17. Gazzaniga M. As funções executivas e os lobos frontais. In: Gazzaniga M, Ivry RB, Mangun GR. Neurociência cognitiva: a biologia da mente. Porto Alegre: Artmed; 2006. p. 517-554.
18. Cypel S. As funções executivas e o aprendizado escolar. In: Valle LELR, Valle ELR. Neuropsiquiatria: infância e adolescência. Rio de Janeiro: WMF; 2007. p. 25-32.
19. Pennington B. Diagnosing learning disorders: a neuropsychological framework. New York: Guilford Press; 1991.
20. Lezak MD. Executive functions and motor performance. (4.a ed). In: Lezak MD, Howieson DB, Loring DW, editors. Neuropsychological assessment. New York: Oxford University Press; 2004. p. 611-641.
21. Helene AF, Xavier GF. A construção da atenção a partir da memória. Rev Bras Psiquiatr 2003;25(Supl 2):12-20.
22. Drake M. Evaluación de las funciones ejecutivas. In: Burin D, Drake M, Harris P. Evaluación neuropsicológica en adultos. Buenos Aires: Paidós; 2007. p. 27-62.
23. Freitas S, Lopes CS, Coutinho W, Appolinario JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr 2001;23:215-220.
24. Bechara A, Damasio AR, Damasio H, Anderson S. Insensitivity to future consequences follwing damage to human prefrontal cortex. Cognition 1994;50(1-3):7-15.
25. Schneider DDG, Parente MAMP. O Desempenho de adultos jovens e idosos na Iowa Gambling Task (IGT): um estudo sobre a tomada de decisão. Psicol Reflex Crít 2006;19:442-450.
26. Graffman J. Experimental assessment of adult frontal lobe function. In: Miller BL, Cummings J (editors). The human frontal lobes: function and disorders. New York: Guilford; 1999. p. 321-344.
27. Pennington B. Diagnosing learning disorders: a neuropsychological framework. New York: Guilford Press; 1997.
28. Kristensen C. Funções executivas e envelhecimento. In: Parente MAMP. Cognição e envelhecimento. Porto Alegre: Artmed; 2006. p. 97-111.
29. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation (TRS 894). Geneva: WHO; 2000.
30. Denburg NL, Tranel D, Bechara A. The ability to decide advantageously declines prematurely in some normal older persons. Neuropsychologia 2005;43:1099-1106.
31. Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before knowing the advantageous strategy. Science 1997;275:1293-1295.
32. Gillberg I, Billstedt E, Wentz E, Anckarsäter H, Rastam M, Gillberg C. Attention, executive functions, and mentalizing in anorexia nervosa eighteen years after onset of eating disorder. J Clin Exp Neuropsychol 2010;32(4): 358-365.
33. Galioto R, Spitznagel MB, Strain G, Devlin M, Cohen R, Paul R, et al. Cognitive function in morbidly obese individuals with and without binge eating disorder. Compr Psychiatry 2012;53:490-495.
34. Marcus MD, Wing RR, Ewing L, Kern E, Gooding W, McDermott M. Psychiatric disorders among obese binge eaters. Int J Eat Disord 1996;9:69-77.
35. Mobbs O, Iglesias K, Golay A, Van der Linden M. Cognitive deficits in obese persons with and without binge eating disorder. Investigation using a mental flexibility task. Appetite 2011;57:263-271.
36. Billingsley-Marshall Rl, Basso MR, Lund BC, Hernandez ER, Johnson CL, Drevets WC, et al. Executive function in eating disorders: the role of state anxiety. Int J Eat Disord 2013;46:316-321.
37. Wu M, Giel KE, Skunde M, Schag K, Rudofsky G, de Zwaan M, et al. Inhibitory control and decision making under risk in bulimia nervosa and binge-eating disorder. Int J Eat Disord 2013;46(7):721-728.
38. Svaldi J, Brand M, Tuschen-Caffier B. Decision-making impairments in women with binge eating disorder. Appetite 2010;54:84-92.
39. Danner UN, Ouwehand C, van Haastert NL, Hornsveld H, de Ridder DT. Decision-making impairments in women with binge eating disorder in comparison with obese and normal weight women. Eur Eat Disord Rev 2012;20:e56-62.
40. Tchanturia K, Liao PC, Uher R, Lawrence N, Treasure J, Campbell IC. An investigation of decision making in anorexia nervosa using the Iowa Gambling Task and skin conductance measurements. J Int Neuropsychol Soc 2007;13:635-641.
 Correspondence:
Correspondence:
Caroline Tozzi Reppold.
Federal University of Health Sciences of Porto Alegre.
Sarmento Leite Street 245
Porto Alegre, RS - Brasil.
Zip Code: 90050-170
e-mail: carolinereppold@yahoo.com.br
Received: 25/03/2017
Accepted: 11/05/2017