INTRODUCTION
Malnutrition in children is a global public health concern because they have a higher risk of dying from infectious diseases 1. It is estimated that malnutrition is the underlying cause of 45% of global deaths in children under five years of age 2,3,4. In children, malnutrition syndromes are responsible for 3.1 million deaths each year 5. Childhood is characterized by a high demand for nutrients to support growth and development 6; therefore, any nutritional insult caused by a disease, infection or fever can have a high metabolic cost that could impair nutritional status and increase morbidity and mortality from other causes, usually infectious diseases 4,5.
While the prevalence of protein-energy malnutrition (PEM) in Mexican children under five years of age has decreased in the last decade 7,8, malnutrition secondary to an underlying pathology has not been widely studied 9. It has been shown that the worldwide prevalence of malnutrition in hospitalized children ranges widely between 6% and 50% 10,11,12,13,14,15. This rate is higher in public hospitals in Latin America, where the prevalence of malnutrition ranges from 7% to 90% 16,17. A percentage of these malnourished patients has been known to deteriorate while in the hospital 10 and on other occasions, patients enter and leave the hospital without undergoing any adequate nutritional assessment 1. One highly specialized Mexican pediatric hospital 9 found that at the time of hospital admission, 17% of children had chronic malnutrition and 8% had acute malnutrition. However, currently there is little information on malnutrition in hospitalized children. Therefore, the purpose of this study was to evaluate the nutritional status in hospitalized children according to their socio-demographic variables, underlying pathology and based on hospital length of stay.
METHODS
In a 2014 cross-sectional study, a convenience sample was collected over nine months consisting of 763 patients admitted to different departments of the Division of Pediatrics, of the Civil Hospital of Guadalajara, Dr. Juan I. Menchaca 18. All patients were admitted Monday through Friday into areas of the Pediatrics Division. Patients who spent less than 72 hours in the Emergency Room and were subsequently admitted in a hospital ward and whose parents or legal guardian signed the informed consent were accepted into the study. Patients hospitalized in the Intensive Care Unit, those with severe burns, and patients with end-stage-kidney-disease (on hemodialysis or peritoneal dialysis) were not included due to technical difficulties in measuring, or to the presence of chronic malnutrition (stunting) of months or years of evolution. Additionally, those children with cerebral palsy, those who could not provide anthropometric measurements or those who were hospitalized more than once in less than a three-month period were not included. Two patients with incomplete files or data were excluded from the analyses. For each participant or family, a questionnaire was administered to the family member or legal guardian that included general identification data and socio-demographic information.
ANTHROPOMETRIC MEASUREMENTS
Two researchers who had been previously standardized in the Habitch method 19 took anthropometric measurements at the time of hospital admission. The weight of children under 24 months was measured without clothes, on a 5 g to 20 kg scale (Seca-354; Seca(r), Hamburg, Germany); children over 24 months were weighed in light clothes or a robe on a scale with a minimum reading of 100 g (Tanita(r) UM-081, Tokyo, Japan). Length of infants and toddlers less than 24 months of age was obtained without clothes in a Seca infantometer-416 mark (Seca(r), Hamburg, Germany). Height of children over 24 months of age was measured using a graduated scale dry-214 mark (Hamburg, Germany) without shoes, with the heels together and the tips of the feet slightly apart and with the head, shoulders, buttocks and heels vertically aligned.
Head circumference was measured in children under three years of age using a metal tape measure (Rosscraft(r), USA). The tape was firmly applied around the head in the supraciliar region, so that it aligned with the most prominent parts of the frontal area and occipital protuberance. Mid-upper-arm circumference (MUAC) was obtained in the middle of the left arm with the same metal tape measure. A tricipital skinfold measurement was taken on the midpoint of the inner, rear face of the previously marked arm; a subscapular skinfold measurement was taken at the lower edge of the scapula. Both measurements were performed on the left side using a Lange skinfold caliper (Michigan, USA).
The Z-scores for the following indices were calculated: weight/length, weight/height, weight/age, length/age, height/age, head circumference/age and BMI/age using the programs WHO Anthro version 3.2.2 and Anthro Plus version 1.0.4 20,21. Reference limits were set as ± 2 SD (z-score), as defined by the World Health Organization (WHO); however, in children under five years of age, overweight and obesity were defined as > 2 SD and > 3 SD, respectively. Additionally, in children over five years of age, overweight and obesity were defined as > 1 SD and > 2 SD, respectively. Body fat percentage was estimated using the triceps and subscapular fold measurements and the Slaughter equation 22.
STATISTICAL ANALYSES
Student's t tests and Chi-squared tests were used to analyze parametric variables in independent samples and non-parametric variables, respectively. ANOVA with post-hoc tests (T3 of Dunnett) were also conducted and odds ratios were estimated with multivariate binary regression logistic models to identify the probability of deficit on the anthropometric indicators. SPSS version 20 software was used for all analyses.
RESULTS
Seven hundred and sixty-one patients were included in the final study analyses. The population was 53% male, 31% infants, 29% toddlers and preschoolers, 23% school children and 17% adolescents. In 25.9% of cases, pathologies with pneumological origins were observed. In the remaining subject population, 20.1% of cases were admitted with internal medicine diseases, 11% with cancer, 10.2% for surgery, 9.9% with neurological issues, 7.9% with infectious diseases, 5.9% with gastrointestinal diseases, and 9.1% of whom there was not a definite diagnosis.
Forty percent of patients' parents were married by civil and religious laws or by civil laws alone, 36% were cohabiting as couple and 10% were single mothers. Sixty percent of the families were nuclear and 29% were extended. The average ages of the father and the mother were 33 ± 9.2 and 30 ± 8.3, respectively. Among parents, 12.6% were illiterate or had incomplete elementary schooling, 22% had completed elementary school, 39.5% had completed junior high school, 19.5% had completed senior high school, and 6.3% had a college degree or higher.
In the total population, it was observed that at the time of hospital admission, 33.4% of subjects had some degree of malnutrition according to their BMI (Table I). When examining the study population, based on hospital length of stay, those with hospital stay of seven days or more (sub-acute and/or chronic evolution) (12.2 ± 7.3) showed a significantly greater deficit in height/age (-0.55 vs -1.07) and BMI/age (-0.24 vs -0.94) than those patients with hospital stay less than seven days (acute evolution) (3.5 ± 1.8), p < 0.001.
When comparing the nutritional status of children with hospital stay less than seven days vs hospital stay of seven days or more, severe malnutrition was observed in 4% vs 14.1% and moderate malnutrition was observed in 6.3% vs 11.2%, respectively (Table II). The risk of having deficient anthropometric indices at admission was higher in children with hospital stay of seven days or more than in children with hospital stay less than seven days for the several indices. Weight/height index was deficient in 23.3% of children with hospital stay of seven days or more vs 9.6% of children with hospital stay less than seven days (OR = 2.9 [95% CI 1.6-5.07], p < 0.001). The height/age index was deficient in children with hospital stay of seven days or more (20.3%) vs 12.4% of children with hospital stay less than seven days (OR = 1.77 [95% CI 1.16- 2.7], p = 0.007). Head circumference was undersize in 32% of children with hospital stay of seven days or more vs 14.9% of children with hospital stay less than seven days (OR = 2.68 [95% CI 1.5-4.7], p < 0.001). Finally, BMI was lower in children with hospital stay of seven days or more (25.2%) vs. 10.5% of children with hospital stay less than seven days (OR = 2.9 [95% CI 1.9,-4.4], p < 0.001).
Table II Percentage of anthropometric indexes (Z score) according to hospital stay: < 7 days vs. ≥ 7 days (n = 761)

Chi-squared test (stratification ± -2 Z score); < 7 days vs ≥ 7 days: *weight/height, p = 0.005; †weight/age, p < 0.001; ‡height/age, p < 0.001; §head circumference, p = 0.017; ǁBMI/age, p < 0.001. Some missing values for unnecessary and/or lack of measurements.
When comparing the nutritional status of subjects according to sex for the weight for age, head circumference and BMI indicators, a significantly greater deficit was observed in males than in females (p < 0.05) (Table III). Regarding BMI, a higher risk of moderate/severe malnutrition in males (18%) than in females (10.5%) was observed (OR = 1.87 [95% CI 1.22-2.85], p = 0.003); there was also greater deficit in head circumference in males (24.6%) than in females (14.7%) (OR = 1.89 [95% CI 1.06-3.37], p = 0.029) and in the weight/age index in males (23.7%) compared to females (16.2%) (OR = 1.61 [95% CI 1.06-2.46], p = 0.024). Table IV shows that infants were the most affected age group at the time of hospital admission (p < 0.001) compared to the preschooler, schoolchildren and adolescent age groups. This trend occurred in both indicators of acute deficit (weight/height and BMI) as well as indicators of chronic deficit (height/age index and head circumference).
Table III Anthropometric indices according to sex
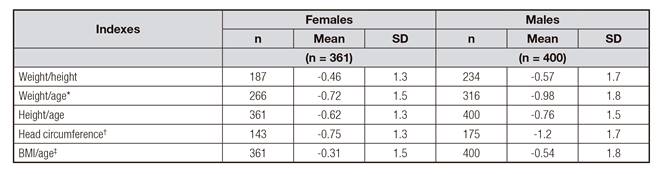
Student's t test for independent samples (two tails) *p = 0.058; †p = 0.010; ‡p = 0.058. Some missing values for unnecessary and/or lack of measurements.
Table IV Anthropometric indexes (Z score) by age group. Mean and standard deviation

One-way ANOVA (post-hoc T3 of Dunnett); height/age: *Infants vs preschoolers, p < 0.001; †Infants vs schoolchildren, p < 0.001; ‡Infants vs adolescents, p < 0.001; **Preschoolers vs schoolchildren, p < 0.001. BMI: §Infants vs preschoolers, p < 0.001; ǁInfants vs schoolchildren, p < 0.001; &Infants vs adolescents, p < 0.001. Some missing values for unnecessary and/or lack of measurements.
It was observed that infants had acute malnutrition (moderate and severe) when using BMI cutoffs (27.3%), whereas chronic malnutrition occurred in 28.5% when using the height/age index. In preschool children, acute malnutrition (moderate and severe) occurred in 6.2% when using BMI cutoffs and chronic malnutrition occurred in 12.7% when using the height/age index. In schoolchildren, there was acute malnutrition in 9.6% of the population when using BMI cutoffs and linear growth retardation (stunting) in 4.2% when using the height/age index. In adolescents, acute malnutrition occurred in 12.2% of the population when using BMI cutoffs and stunting, in 6.9% when using the height/age index. Overweight/obesity was observed in 27.6% of schoolchildren and 25.9% of adolescents, while in infants and preschool children, overweight and obesity were rare (Table V). Infants risk of deficit in BMI was 27.3%, compared to 6.2% in preschool children (OR = 5.7 [95% CI 3.1-10], p < 0.001), 9.6% in schoolchildren (OR = 3.5 [95% CI 1.95-6.37], p < 0.001) and 12.2% in adolescents (OR = 2.6 [95% CI 1.48-4.89], p < 0.001). With the height/age index, a higher risk of deficiency was observed in infants (30.5%) than in preschool children (12.7%) (OR = 2.74 [95% CI 1.69-4.43], p < 0.001), school children (4.2%) (OR = 9.1 [95% CI 4.06-20.45], p < 0.001), and adolescents (6.9%) (OR = 5.41 [95% CI 2.60-11.26], p < 0.001). Additionally, a higher rate of deficiency in the height/age index was also observed in the preschool aged subjects (12.7%) than in the schoolchildren (4.2%) (OR = 3.33 [95% CI 1.42-7.80], p = 0.006).
Table V Frequency and percentage (%) of anthropometric indexes (Z-score) by age group,

Chi-squared test: *weight/height, p = 0.004; †weight/age, p < 0.001; ‡height/age, p < 0.001; §head circumference, p < 0.001. Some missing values for unnecessary and/or lack of measurements.
When examined according to BMI, the prevalence of acute malnutrition (moderate/severe) was more frequent in pathologies of: gastroenterological origin (26.7%), internal medicine (19.7%), pneumology diseases (15.2%), those without clear diagnosis (15.9%) and to a lesser extent, surgical (12.8%), infectious (8.3%), neurological (8%) and oncological (7.2%) pathologies. Additionally, low BMI was more frequent in patients with gastrointestinal diseases than in those with oncological (p = 0.011) or neurological diseases (p = 0.033). Deficit in the height/age index was higher in patients with pneumological diseases than surgical pathologies (p = 0.016).
Table VI shows four logistic binary regression models with BMI and height/age index (low vs normal) that included personal, demographic and education variables of families that predict the risk of malnutrition.
Table VI Logistic binary regression models with BMI (z) and height/length for age (z) as dependent variables and socio-demographic and educational data as covariates in the whole population, n = 761

OR: odds ratio; CI: confidence interval. *Single, cohabiting with a partner, widow. †Extensive or composite families or single parents. BMI: father's age < 20 years (OR = 3.5, CI 95% 1.8-6.7, p < 0.001) and mother's elementary education (OR = 2.2, CI 95% 1.4-3.6) were independently associated with < -2 SD z-score for BMI but could not be included in either of the two logistic regression models. Length- or height-for-age: marital status was independently associated (OR = 1.5, CI 95% 1-2.4, p = 0.05) but could not be included in either of the two logistic binary regression models.
DISCUSSION
This study included 761 patients, of whom infants were the predominant age group, as is common in other studies 11,23. Most parents were cohabiting couples, though a small percentage were married by civil and religious laws, or civil laws alone, which is increasingly happening in Mexico 24. These data confirm that a major fraction of the Guadalajara metropolitan population has significantly changed their lifestyle and way of living as a couple compared to what was occurring some years ago 9,25. Approximately 60% of families included in the study were nuclear and the remaining families were extended or composite, consistent with other findings made in the Guadalajara metropolitan area (Strategic Plan of the Metropolitan Area of Guadalajara, 2010). It is likely that the economic situation of young families today influences the observed family structures. For example, the monthly family income was 2.4 ± 0.22 minimum wages (MW $ 70.10 per day), equivalent to $ 3.9 USA dollar per day (in 2014, average annual peso: dollar ratio was 17.9:1).
By dividing the study population according to hospital length of stay (stays less than seven days and stays seven days or longer), it was observed that rates of both acute and chronic malnutrition were significantly higher in children with hospital stay of seven days or more. Especially infants were the most likely to have both acute and chronic malnutrition. In another study 10, similar results were observed, with 40% of infants showing some degree of malnutrition.
The pediatric population that was admitted to the hospital showed particular anthropometric characteristics. In infants, the prevalence of acute, moderate and severe malnutrition (BMI) was high (27.3%). Contrastingly, in preschool children the prevalence of acute, moderate and severe malnutrition was measured to be 7%. This prevalence increased to 9.6% in schoolchildren and 12% in adolescents. Moreover, chronic malnutrition is common in infants (28.5%), significantly lower in preschool children (13%) and lower still in schoolchildren (4.2%). An interesting finding was that between 26% and 28% of children and adolescents were overweight/obese. This high prevalence of overweight/obesity in hospitalized children reflects the nutrition transition and the high prevalence of overweight and obesity in children and adolescents in the general Guadalajara metropolitan area 8. It also reflects the nutrition transition happening in the Mexican population, with the simultaneous presence of acute and chronic malnutrition and obesity within the same community 9,23,26. This phenomenon has also been observed in hospitalized Canadian children 11, with a prevalence of 6.9% acute malnutrition, 13.4% chronic malnutrition and 30.8% overweight/obesity. Similarly, in Brazilian hospitalized children 17), 16.1% of the study population showed under nutrition and 19.17% had overweight/obesity.
It was observed that males had a higher frequency of acute and chronic malnutrition than females. This trend would explain the differences found in the anthropometric measurements, which would be a result of frequent infections in the "windows" of more active physical growth 27. It has been suggested that early life morbidity and mortality is more common in males than in females 26,28. However, this finding does not coincide with findings observed by other authors, who have shown that acute and chronic malnutrition is more common in girls than in boys 29, especially in extremely poor and/or indigenous populations.
The pathologies that led to hospitalization were varied, so it was difficult to interpret the potential impact of any particular pathology on nutritional status. However, both acute malnutrition and chronic malnutrition occurred in patients with pneumological, gastroenterological and internal medicine pathologies. One explanation for this could be that the gastroenterological and pneumological patients were generally infants and preschool children with relatively severe acute diseases as well as secondary insufficient feeding. It should be noted that in older children (school children and adolescents), the severity of the pathology at the time of admission significantly affected their nutritional status during their hospital stay.
The first binary logistic regression model presented, which used individual profiles of the participants, showed that when patients remained in the hospital for more than seven days, they were most likely to be male and under six years of age, and they had 2-3 times the probability of low BMI as an expression acute malnutrition. The second binary logistic regression model showed that participants whose parents were not united by civil and/or religious laws, with a maternal age less than 23 years and with only basic paternal education, had a 1.2-2 times higher probability of having a low BMI. The third binary logistic regression model showed that the odds of a deficit in the height/age index were 1.6-4.1 times higher in children under six years of age, whose mothers received only basic education, who were hospitalized for more than seven days and who came from non-nuclear families. Finally, the last binary logistic regression model showed that the odds of deficit in the height/age index were 1.7 to 2.3 times higher in patients whose fathers were under 20 years of age and whose mothers were under 23 years of age and had only an elementary education.
One strength of this study is its duration (nine continuous months between April and December), which limits seasonal biases. Additionally, the sample size was quite large and included virtually all children who were hospitalized during the study duration. A potential limitation of the study was that children admitted for severe malnutrition or severe burns, children admitted directly to the Intensive Care Unit, patients with chronic renal disease and replacement therapy (hemodialysis and/or peritoneal dialysis) and children with cerebral palsy were not included. We believe that such patients require very special and selective assessment of the nutritional status and a specific dietary management.
In conclusion, it should be emphasized that nutritional status assessment upon admission to the hospital is very important because if there is some degree of malnutrition, it is likely that it will be exacerbated during hospitalization and could thus increase the risk of complications or even death. It is also important to consider that the type of pathology prompting hospital admission as well as the hospital length of stay can expose pediatric patients to greater risk for worsened nutritional status, particularly if they are infants, toddlers or, as shown in this study, males. Additionally, it was clear that regardless of the characteristics of the patients and their pathologies, there were social, demographic and educational family risk factors that also potentially influence both acute and chronic malnutrition.















