INTRODUCTION
Comparatively with European or North-American populations, severe alcoholic hepatitis (SAH) has a very high mortality rate in Mexican population, being as high as 50 to 81% in those classified as Age-Bilirubin-INR-Creatinine score (ABIC) B or C; this is true in spite of specific treatment with steroids or pentoxifylline 1.
Recently, STOPAH trial demonstrated that neither steroid nor pentoxifylline treatment has a significant impact on the long-term mortality-rate of patients with SAH. But steroids can be helpful to improve 30-day survival in these patients 2.
Risk factors associated with early mortality in patients with SAH are: age, raise on serum creatinine, hyperbilirubinemia, leukocytosis, and alcohol intake > 120 g/day 1. One of the most important factors related to 30-day mortality is the development of acute renal failure (ARF); moreover, the amount of alcohol intake (median 219 g/day) is related to the development of ARF. The development of two or three simultaneous complications, such as ARF, hepatic encephalopathy, or variceal bleeding, increase the mortality risk in patients with SAH 3.
The liver failure is a condition that accelerates starvation; therefore, malnutrition is a common complication of liver disease. The prevalence of clinically significant malnutrition varies from 65% to 100% among patients with chronic liver disease 4. Malnutrition as a risk factor associated with mortality in patients with SAH has been evaluated in a few studies 5,6,7, but never was evaluated specifically in Mexican patients, a population with a high early mortality-rate 1,3.
The aim of this study was to explore which clinical factors are related to early mortality (at 30 days) in a population with a high mortality rate despite specific therapy for SAH, and to identify if malnutrition has influence in survival of patients with SAH.
SUBJECTS AND METHODS
TYPE OF STUDY AND SELECTION CRITERIA
A retrospective cohort study, which included patients with SAH, defined by a Maddrey's discriminant function ≥ 32, attended at tertiary care center, from January 2010 to July 2015. Patients with the following comorbidities were excluded: diabetes, viral hepatitis, patients who requested voluntarily their discharge from hospital, who were not treated with prednisone or pentoxifylline, co-infected with human immunodeficiency virus, or with diagnosis of hepatocarcinoma.
PROCEDURE
Demographic, clinical and biochemical data were collected. The following data were registered: amount of alcohol intake, development of ARF, hepatic encephalopathy, variceal bleeding, bacterial infections, suggestive changes of cirrhosis reported in the ultrasonography. The nutritional status determined through the global subjective assessment (GSA) 8 at patient admission classified patients in one of three different categories: well-nourished, at risk of malnutrition, or severe malnourished. Treatment with prednisone or pentoxifylline was also verified. Also, the outcome (death or survival) since the admission to hospital until a 30-day follow-up was registered.
STATISTICAL ANALYSIS
Quantitative variables were resumed with mean and standard deviation when their distribution was normal, or with median and range in case of non-parametric distribution. For qualitative variables proportions and percentages were employed. The characteristics between groups were compared using Student's t test for independent samples or Mann-Whitney U test in case of continuous variables, and through Chi-squared test of Fisher's exact test for categorical variables. For the survival analysis, Kaplan-Meier curves and the log rank test were used. The association between risk factors and 30-day mortality was determined through hazard ratios (HR) and their respective 95% confidence intervals were calculated using Cox regression models. All those significant variables with a p value ≤ 0.05 identified in the univariate analysis were included in the multivariate analysis. The SPSS version 19.0 (Chicago, Illinois, USA) was used.
RESULTS
Seventy six patients were included, 72 (94.7%) were male, mean age was 43 ± 9.1 year-old, and 58 (76.3%) had changes compatible with cirrhosis in the ultrasonography. According to the GSA, 38 (50%) had severe malnutrition, 22 (28.9%) were at risk of malnutrition, and 16 (21.1%) were well-nourished. The overall 30-day mortality in this cohort was 46 patients (60.5%). The characteristics of patients at admission to hospital according to their outcome at 30 days of follow-up are summarized and compared in Table I.
Table I. Characteristics of patients at admission to hospital and comparison according to outcome at 30-day follow-up
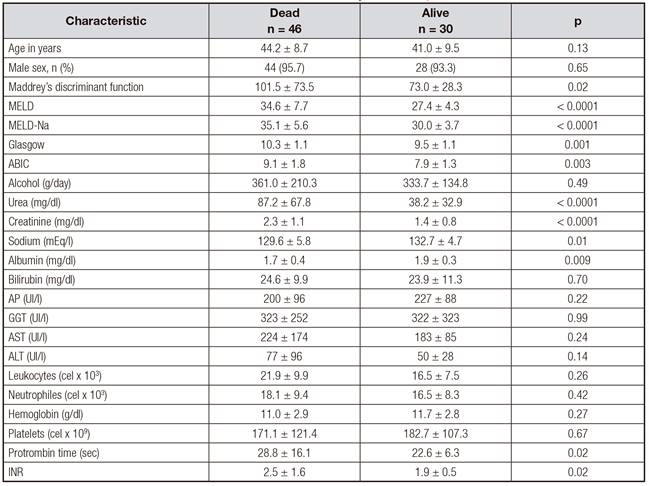
ABIC: age-bilirubin-INR-creatinine; ALT: alanine aminotransferase; AP: alkaline phosphatase; AST: aspartate aminotransferase; GGT: gamma glutamiltransferase; INR: international normalized ratio; MELD: Model for End-stage Liver Disease; MELD-Na: Model for End-stage Liver Disease-Sodium. t de Student, Chi-squared: statistical significance p < 0.05.
In the univariate analysis, the following variables were associated with 30-day mortality: concomitant cirrhosis (OR = 2.3; 95% CI: 1.5-3.4; p < 0.0001), development of hepatic encephalopathy (OR = 5.6; 95% CI: 2.5-12.5; p < 0.0001), development of ARF (OR = 6.2; 95% CI: 2.5-15.6; p < 0.0001), variceal bleeding (OR = 4.4; 95% CI: 1.7-11.3; p < 0.0001), bacterial infection (OR = 2.7; 95% CI:1.3-5.8; p = 0.004), at risk of malnutrition according to the GSA (OR = 2.0; 95% CI: 1.2-3.3; p = 0.01), and severe malnutrition according to the GSA (OR = 5.8; 95% CI: 2.0-16.4; p < 0.0001). Neither therapy with prednisone nor therapy with pentoxifylline improved survival in patients with SAH. Neither was difference between the treatment groups (Table II).
Table II. Univariate analysis comparing the clinical characteristics of surviving versus non-surviving patients during the 30-day follow-up

ARF: acute renal failure; GSA: global subjective assessment; HE: hepatic encephalopathy; OR: odds ratio; USG: ultrasonography; VB: variceal bleeding. §Comparison using Chi-squared between * and †. ǁComparison using Chi-squared between * and ‡. Statistical significance p ≤ 0.05.
When all significant variables in the univariate analysis were adjusted in a multivariate analysis, only severe malnutrition was associated with 30-day mortality (OR = 6.4; 95% CI: 1.9-22.1; p = 0.003) (Table III and Fig. 1).
Table III. Multivariate analysis to identify risk factors associated with early mortality in patients with severe alcoholic hepatitis
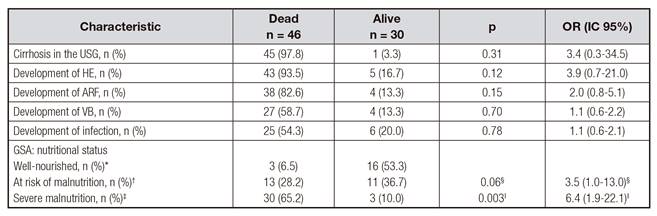
ARF: acute renal failure; GSA: global subjective assessment; HE: hepatic encephalopathy; OR: odds ratio; USG: ultrasonography; VB: variceal bleeding. Cox regression model. §Comparison between * and †. ǁComparison between * and ‡. Statistical significance p ≤ 0.05.
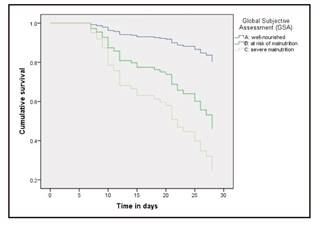
Figure 1. Kaplan-Meier curves showing 30-day survival according to nutritional status in a cohort of patients with severe alcoholic hepatitis. Cox regression, p = 0.008. Adjusted model for the following co-variables: development of hepatic encephalopathy, variceal bleeding, acute renal failure, infection, concomitant cirrhosis on the ultrasonography.
DISCUSSION
In Mexico, mortality related to chronic liver disease is among the main causes of general mortality, occupying the fourth place 9, making it one of the countries with the highest rates of liver-related mortality 10. The Ministry of Health estimated an average of 25,000 deaths from cirrhosis between 2000 and 2010 11. In Mexico, alcohol is the leading cause of cirrhosis, followed by hepatitis C and non-alcoholic steatohepatitis. In addition, when patients seek medical attention, they are often at advanced stage of the disease (Child-Pugh C) with obvious manifestations of decompensation, and they often continue to intake alcohol despite the diagnosis of liver disease. All these factors contributed to high mortality at productive age 12,13.
SAH is characterized by the rapid onset of jaundice and coagulopathy in patients with active and chronic alcohol intake 14. The reported mortality, as well as the response to therapy with steroids or pentoxifylline, is extremely variable among different populations. Some authors report mortality greater than 50% at two months without specific treatment (steroids) 15,16,17. In France, treatment with prednisolone has been shown to be effective reducing mortality to 35% at six months of follow-up 18,19,20. Nevertheless, up to 40% of patients do not respond to steroid therapy, and particularly in these non-responder patients, mortality has been reported greater than 75% 16,21. On the other hand, several studies in Mexican population have found high mortality-rate and failure to steroid and pentoxyfilline treatments. A cohort study in Mexican population found that near to 90% of patients with SAH were non-responders to steroid therapy according to the Lille model (Lille score value > 0.45 after seven days of treatment with prednisone) 22. A retrospective study by Garrido-García et al. found a mortality-rate as high as 59.9% at 28 days of follow-up, despite treatment with prednisone 23. In English population, the STOPAH trial, which included the greatest number of patients with SAH in a clinical trial, did not show usefulness of steroids or pentoxifylline; however, mortality-rate at 28 days in all groups was extremely low: 17% in the p lacebo group, 14% in the prednisolone group, 19% in the pentoxifylline group, and 13% in the prednisolone plus pentoxifylline group 2.
Several studies have tried to explain which factors are related to a higher mortality in patients with SAH. The development of ARF is one of the most important mortality predictive factors 24. Interleukin-2 has been identified as a factor related to steroid treatment resistance 25. The amount of alcohol intake > 120 g/day has been also related to higher mortality-rate 1. Other factors associated with higher mortality-rate are age, raised serum creatinine, hyperbilirubinemia, leukocytosis, and also the synergistic effect of the development of two or three simultaneous complications as ARF, hepatic encephalopathy, or variceal bleeding 1,3. In the univariate analysis, our study confirmed ARF, variceal bleeding, hepatic encephalopathy, and infection are clinical factors related to a higher mortality-rate in patients with SAH.
Malnutrition is a prevalent comorbid condition in Mexican alcoholic patients. The prevalence of malnutrition and its degree correlates with the severity of chronic liver disease and its complications 26. But, until now no study has previously evaluated the impact of malnutrition on mortality of Mexican patients with SAH. Our study shows that severe malnutrition is a determinant factor which explains the high mortality-rate in Mexican patients with SAH. As the Kaplan-Meir curves and the multivariate analysis show, malnutrition resulted to be the most important risk factor related to high early mortality in these patients.
The prevalence of malnutrition in patients with cirrhosis is widely variable; it has been reported from 25% to 80%, depending on the clinical severity of the disease and the specific evaluation method used 27,28,29.
The European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines recommend clinical methods, as the GSA, to evaluate the nutritional status in patients with liver diseases 30,31. The GSA is a routinely used tool in our hospital to evaluate nutritional status in patients with liver diseases. In our study, a high frequency of severe malnutrition was found, which is in agreement with previous findings reported by other authors 27,28,29.
The liver participates in the caloric homeostasis regulation 32. Patients with liver disease are susceptible to malnutrition due to several factors such as poor ingestion, fat malabsorption, intestinal loss of proteins, decreased protein synthesis, hypermetabolic state, symptoms as nausea, vomiting, early satiety, insulin resistance, gastroparesis, ascites, bacterial overgrowth 33. There is also over-regulation of inflammatory mediators that interfere with appetite, such as the tumor necrosis factor-alpha 34, which is significantly elevated in patients with SAH 14.
Sarcopenia is a common complication in patients with chronic liver disease and it worsens as chronic liver disease worsens 35,36; likewise, malnutrition is a predictor of morbidity and mortality in patients with chronic liver disease 34. Similarly to our finding about the association between malnutrition and higher mortality at 30 days, other authors have found in different populations a relationship between malnutrition and higher mortality-rate at 30-day, 6-month and 12-month follow-up in patients with SAH 5,6,7.
The American Association for the Study of Liver Disease and the European Association for the Study of the Liver recommend enteral nutrition with the objective of preserving the integrity of the intestinal barrier and avoiding the pathological increase in intestinal permeability, as well as to prevent the risk infection due to bacterial translocation infection, promote the anabolism to preserve muscle mass and prevent sarcopenia, and restore deposits of glutathione, a potent cellular antioxidant which is severely depleted in SAH 37.
CONCLUSIONS
This study confirms that nutritional status is an important factor associated with early mortality (first 30 days) in patients with SAH. Severe malnutrition clearly explains the high mortality observed in Mexican patients with SAH. The evaluation of nutritional status is essential as part of the initial assessment of patients with SAH since it behaves as a prognostic factor. Strategies to prevent nutritional deterioration are crucial in order to improve the survival of these patients.














