INTRODUCTION
Obesity is the most prevalent nutritional and metabolic disorder in the world. According to the World Health Organization (WHO), approximately 600 million adults are considered with obesity. It is estimated that these figures will double up to 2030 1.
In adolescents, severe obesity, especially when combined with associated diseases, causes these youngsters to present a high risk of premature mortality and morbidity in adult life 2.
Increased vitamin D deficiency (VDD) occurs together with obesity, and the association between these two conditions has been observed both in adults and in adolescents 3. It is estimated that one billion people in the world have some degree of VDD 4.
It has been reported that 25-hydroxycholecalciferol (25(OH)D) is inversely related to body fat, indicating that obesity is a risk factor for this deficiency. According to Fish et al., obese individuals feature double risk to develop VDD when compared to eutrophic individuals. This is possibly due to the presence of the vitamin D receptor (VDR) in the adipose tissue, which can cause its retention, thus reducing its availability to the tissues targeted 5.
The effects of the biologically active form of vitamin D (VD) (1,25(OH)2D or calcitriol) are mediated by VDR, which is present in the main sites of action of this vitamin, such as kidney, parathyroid glands, intestine, and bone. The discovery that VDR is expressed in almost all cells of the body suggests the involvement of VD in various other systems, in addition to the musculoskeletal tissues 6.
Calcitriol plays an important role in glucose homeostasis by improving insulin sensitivity in the target cells (liver, skeletal muscle and adipose tissue), in addition to increasing and improving the function of the pancreatic -cells 7.
A prospective evaluation showed a significant association between smaller serum concentrations of 25(OH)D with hypercholesterolemia 8. However, one must take into account that the results involving this vitamin and blood lipids may exhibit confusion factors, due to its relation with obesity 9.
There are reports that low concentrations of 25(OH)D are associated with the severity of nonalcoholic fatty liver disease (NAFLD). It is speculated that VDD can exacerbate nonalcoholic steatohepatitis (NASH), in part, through the regulation of the bioavailability of bile acids 10.
Metabolic syndrome (MS) is directly related to the development of atherosclerotic cardiovascular disease and some studies show a possible connection between VDD and MS 11.
The findings that identify serum inadequacy of 25(OH)D all over the world have aroused more and more interest in assessing the relationship of this vitamin with metabolic diseases. However, the information available up to the present time refers mainly to adults and the elderly and shows that studies addressing adolescents are scarce.
Considering that the time of exposure to obesity increases the chances of early development of metabolic diseases, this study aimed to assess the nutritional status of vitamin D and metabolic profile in adolescents and adults with obesity and the relationship between complications arising from severe class of obesity with vitamin D nutritional status and to compare the differences between these groups.
MATERIALS AND METHODS
This is a comparative observational study. The study population comprised adolescents with severe obesity (G1) in accordance with estimations by the WHO (2007) 12 and adults with class III obesity (G2) in accordance with estimations by the WHO (1998) 13. They were attended in a clinic specialized in the control of obesity in the municipality of Rio de Janeiro. Data collection was conducted from March 2011 to December 2013.
This was a convenience sampling comprising all patients who, in the collection period, met the following inclusion criteria: adolescents aged between ten and 19 years and eleven months with body mass index (BMI)/age in the percentile higher than 99.9, and adults aged between 20 and 60 years, with a BMI equal to or higher than 40 kg/m². Exclusion criteria were: prior malabsorptive and restrictive surgeries, malabsorptive intestinal syndromes, neoplasia, use of lipid-lowering drugs, use of hypoglycemic drugs, use of medication or vitamin supplement containing vitamin D, to be pregnant or a nursing mother, and to have kidney and liver diseases, except for hepatic steatosis.
Patients underwent anthropometric, biochemical and clinical evaluations. For anthropometric evaluation, body weight was measured with the aid of an electronic platform scale with a 300 kg capacity and a 100 g variation. Height was obtained with a stadiometer coupled to the scale, up to 200 cm long, with 0.1 cm accuracy, patient standing, barefoot, heels together, back straight position, and arms extended alongside the body. BMI was calculated through the ratio of body weight (kg) and the square of the height (m²). Waist circumference (WC) was assessed with a flexible and inelastic measuring tape, 200 cm long and with 0.1 cm variation. Measurement was carried out in the largest sagittal abdominal diameter, with the individual standing, relaxed abdomen, arms alongside the body, feet together and weight divided into both legs. Measurement was carried out at the end of the individual expiration. For adults, cut-off points were those estimated by the WHO (1998) 13. For adolescents, this cut-off point was based on the 90th percentile proposed by Freedman and et al. 14.
All measurements were made in duplicate by a single trained evaluator, 0.5 cm variations were accepted, and mean was calculated among the values.
The collection of material for the biochemical data analysis was conducted in a specialized laboratory which maintains an agreement with the clinic. The 10 ml blood samples were obtained by venipuncture, after a 12-hour fasting for the assessment of serum concentrations of 25(OH)D, lipid profile (total cholesterol, LDL-c, HDL-c and triglycerides), C-reactive protein (CRP), blood sugar, and fasting insulinemia.
VD analysis was made by 25(OH)D quantification. The method used was high performance liquid chromatography with ultraviolet detector (HPLC-UV), a method considered as the gold standard for this analysis 15.
VDD was defined as values lower than or equal to 20.0 ng/ml; insufficiency, between 21 ng/ml and 29 ng/ml; and sufficiency, between 30 ng/ml and 99 ng/ml 16.
For completing the evaluation of the nutritional status of VD, we conducted an evaluation of sun exposure of patients using a protocol translated into the Portuguese language and validated by Hanwell and et al. 17.
For determining fasting glucose, we applied the enzymatic colorimetric method and the cut-off point adopted for inadequacy was equal to or higher than 100.0 mg/dl for adults and adolescents, in accordance with the International Diabetes Federation (IDF) 18. The level of insulin resistance was calculated by the formula of the Homeostasis Model Assessment Insulin Resistance (HOMA-IR). The cut-off point adopted for obese adults and adolescents was higher than 2.5 19,20.
The concentrations of total cholesterol and triglycerides were analyzed by the enzymatic colorimetric method and the LDL-c and HDL-c fractions were analyzed by the selective inhibition method. The reference values adopted for adolescents and adults were in accordance with the V Brazilian Guideline of Dyslipidemia and Atherosclerosis Prevention (2013) 21.
The measurement of blood pressure was performed using the oscillometric technique with a semi-automatic digital arm device, validated and properly calibrated. The measurement was carried out after a five-minute rest and was repeated twice, with a one-minute interval between them. The mean of the two measurements was used. The reference adopted for the classification of high blood pressure in adolescents and adults was in accordance with the VI Brazilian Guidelines for Hypertension (2010) 22. For patients on antihypertensive drugs, the previous confirmed diagnosis of systemic arterial hypertension (SAH) was used for classification in the study, instead of the one-off measurement of blood pressure.
CRP was dosed by the nephelometry method. The cut-off point adopted for considering a high cardiovascular risk for adults was higher than 0.3 mg/dl 23, and higher than 0.5 mg/dl for adolescents 24.
For diagnosis of NAFLD, total abdominal ultrasound was used. The exam was conducted and interpreted by one single specialized doctor.
For diagnosis of MS, we applied the criteria proposed by the International Diabetes Federation (IDF) for adults and adolescents 25.
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) for Windows version 17.0. The Kolmogorov-Smirnov test was applied to evaluate the symmetry of the distributions of the continuous variables. For data analysis, the distribution type of the sample was assessed, and for each type of distribution statistical tests were performed later. When distribution was normal, the following tests were applied: the Student's t-test for comparison between continuous variables and the Pearson correlation coefficient. For non-normal distribution, the Mann-Whitney test was used. The Chi-square test was used to assess the association between the categorical variables. The significance level adopted was 5% (p < 0.05).
This study was approved by the Research Ethics Committee of the Hospital Universitário Clementino Fraga Filho (Research Protocol no. 011/06). Patients inclusion was carried out upon signing of the informed consent either by the patient or his/her legal guardian, in accordance with resolution no. 196 of the National Health Council (Conselho Nacional de Saúde).
RESULTS
The sample consisted of 128 individuals. A total of 60 participants comprised the adolescent group (G1), being 63.3% female and 36.7% male, with a mean age of 17.32 ± 1.35 years. A total of 68 participants comprised the adult group (G2), being 75% female and 25% male, with a mean age of 39.31 ± 9.45 years. Table 1 shows the general characteristics of the sample.
Table I. Mean values of the anthropometric, biochemical and clinical variables of 128 Brazilian adolescents and adults with severe obesity

SD: standard deviation; HDL-c: high density lipoprotein; HOMA-IR: Homeostasis Model Assessment -Insulin Resistance; BMI: body mass index; LDL-c: low density lipoprotein; WC: waist circumference; CRP: C-reactive protein.
*Values with statistical significance (p ≤ 0.005).
†Student's t-test, Mann-Whitney test.
Table 1 also shows the time of sun exposure presented by the individuals studied, with a record of 17 ± 1.27 minutes/day and 13 ± 1.46 minutes/day for adolescents and adults, respectively.
There were no significant differences between the groups in relation to body weight, BMI and WC. The only variable with significant differences between the groups was HOMA-IR, with higher means in adults (p = 0.000). There was also a trend of higher means of blood glucose in adults (p = 0.070).
The percentage of inadequacy of VD (deficiency and insufficiency) was observed in 90% and 79.4% in G1 and G2, respectively. The percentage of deficiency and insufficiency of 25(OH)D in G1 was 43.3% and 46.7% and in G2 it was 35.3% and 44.1%, with no significant differences between the groups, as shown in Table 2.
Table II. Classification of biochemical and metabolic variables according to the age group of 128 Brazilian adolescents and adults with severe obesity

NAFLD: non-alcoholic fatty liver disease Chi-square test.
*Values with statistical significance (p ≤ 0.005).
The duration of sun exposure was 17 minutes in G1 (17 ± 1.27) and 13 minutes in G2 (13 ± 1.46), with significant differences between the groups (p = 0.000).
With respect to NAFLD, prevalence of 80% and 79.4% were observed in G1 and G2, respectively. High blood pressure was found in 65% of the individuals in G1 and in 60.3% in G2, and MS was present in 60% of adolescents and in 63.2% of adults, as shown in Table 2.
The analysis of the prevalence of metabolic disorders according to VD nutritional status showed 80% vs 78% of NAFLD, 67% vs 60% of high blood pressure, 56% vs 61% of MS, 63% vs 57% of hypercholesterolemia, 46% vs 31% of hypertriglyceridemia and 72% vs 87% of insulin resistance in adolescents and adults, respectively, with inadequate nutritional status of VD (insufficiency and deficiency) as shown in Figure 1 and Figure 2. It was observed that the prevalence of metabolic alterations in adolescents and adults is high regardless of the nutritional state of the VD; however, when comparing the groups, it is observed that adolescents present higher prevalence of these when VD inadequacy was present than adults in the same situation (p = 0.040).
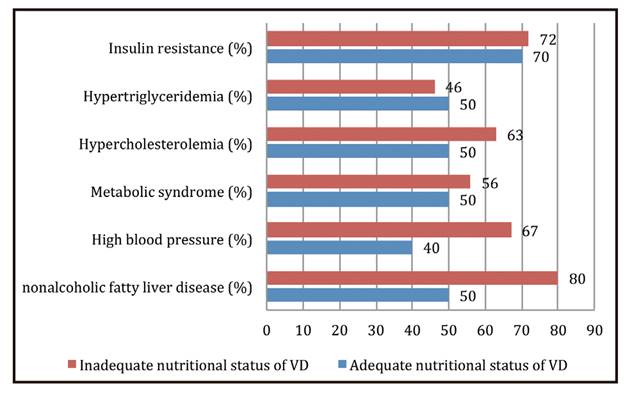
Figure 1. Prevalence of metabolic disorders of 60 Brazilian adolescents with severe obesity according to the nutritional status of vitamin D.

Figure 2. Prevalence of metabolic disorders of 68 Brazilian adults with severe obesity according to the nutritional status of vitamin D.
When the relationship of 25(OH)D with the metabolic profile of the individuals was assessed, a negative and significant correlation of BMI in G2 with the values of 25(OH)D was observed (r = -0.244; p = 0.045). This correlation showed no statistical significance in the adolescent group.
We found that individuals with inadequacy of the nutritional status of VD showed higher values both in the adolescent group (p = 0.000) and in the adult group (p = 0.000). In addition, a strong significant negative correlation was also observed between the means of 25(OH)D and CRP in G1 (r = -0.871; p = 0.000) and in G2 (r = -0.811; p = 0.000).
In relation to glucose, we observed a tendency to association of elevated values with inadequacy of vitamin D in adolescents (p = 0.080). This association was not found in adults (p = 0.171).
HOMA-IR showed a significant negative correlation with 25(OH)D in G1 (r = -0.832; p = 0.000) and in G2 (r = -0.589; p = 0.000). In addition, it was observed that individuals with inadequacy of VD showed higher values of HOMA-IR (G1: p = 0.000/ G2: p = 0.000).
When evaluating the lipid profile, it was observed that the deficiency of VD showed association with high total cholesterol in G1 (p = 0.029). Individuals with deficiency of this vitamin also showed higher values of LDL-c in G2 (p = 0.003), which was a trend in the adolescent group (p = 0.055). No statistically significant association was observed between VD with HDL-c and triglycerides.
No statistically significant association was observed in VD with HS, high blood pressure and MS.
DISCUSSION
A high prevalence of inadequacy of 25(OH)D was observed in both groups, which corroborates data from other studies that also reported inadequacy of this vitamin in subjects with obesity 26,27.
Individuals with obesity have twice the risk of developing VDD when compared to eutrophic individuals. It has been observed that these individuals tend to be less exposed to ultraviolet rays due to the increased use of clothing, limited mobility and use of sunscreen 28. In addition, it is worth highlighting a study that reported that individuals with obesity showed an attenuated response to solar radiation when compared to eutrophic individuals, thus impairing the synthesis of 25(OH)D 29. In the present study, the amount of time of sun exposure was 17 ± 1.27 minutes/day for adolescents and 13 ± 1.46 minutes/day for adults.
As regards the association of 25(OH)D with BMI, a negative and significant correlation of these variables was observed only in the adult group. Publications on adults with obesity present strong evidence that body fat mass is inversely related to the serum concentrations of 25(OH)D 30. A study that assessed the relationship between BMI and 25(OH)D through information of 21 adult cohorts (42,024 participants) noted that each increase of 1 kg/m² in BMI was associated with reduction of 1.15% of the concentration of 25(OH)D 9.
In the present study it was found that CRP showed high negative correlation with concentrations of 25(OH)D and, in addition, individuals with inadequacy of VD showed higher values of CRP with respect to the adequacy of this vitamin, both in G1 and G2. CRP is a sensitive marker of inflammation and is positively correlated with BMI and abdominal fat, and is closely related to the increased risk of cardiovascular events 31.
A double-blind study conducted in adults with NAFLD reported that patients receiving supplementation of VD showed significant reduction of serum CRP values when compared to individuals in the placebo group 32. Another publication, focusing on hypertensive adults, reported that the correction of VDD with supplementation showed no significant effect on the concentrations of CRP 33.
With regard to adolescents with obesity, an intervention study in 35 subjects with VDD showed that supplementation of VD, for six months, improved the nutritional status of this vitamin, but no significant change in inflammatory markers occurred, including CRP 30.
In the present study, we only observed a trend of association of elevated blood glucose with the inadequacy of 25(OH)D in the adolescent group. However, when evaluating the marker of insulin resistance (HOMA-IR), a significant negative correlation with the 25(OH)D was observed in both groups and the inadequacy of 25(OH)D was also associated with high values of HOMA-IR in G1 and G2. In a systematic review comprising 21 prospective studies with a total of 76,220 participants, Song et al. reported a reduction of 38% in the relative risk in the incidence of type 2 diabetes mellitus (DM2) among individuals with higher plasma concentrations of 25(OH)D, compared to individuals with lower concentrations 34.
A meta-analysis involving 3,612 cases and 55,713 controls suggested that the future risk of DM2 can be reduced by 41% with serum concentrations of 25(OH)D higher than 32 ng/ml, compared to serum concentrations lower than 19.5 ng/ml 35.
In a randomized trial about adolescents with obesity with inadequacy of VD receiving vitamin D3 supplementation or placebo for six months, it was observed that the patients supplemented showed increased serum concentrations of 25(OH)D (19.5 ng/ml compared to 2.5 ng/ml in the placebo group; p = 0.001), fasting insulin (26.5 un/ml compared to 1.2 un/ml in the placebo group; p = 0.026) and HOMA-IR (21.36 compared to 0.27 in the placebo group; p = 0.033). These authors concluded that the correction of the inadequacy of VD through supplementation can be an effective complement to the standard treatment of obesity with associated IR 30.
In the present study, it was observed that VDD showed association with some components of the lipid profile, such as high total cholesterol in adolescents and increased values of LDL-c in adults, as well as a trend of the latter in the adolescent group.
A prospective evaluation showed a significant association between lower concentrations of VD with hypercholesterolemia 8. Another study showed that there was an association between concentrations of 25(OH)D and hypertriglyceridemia and dyslipidemia, even after an adjustment for several confusion factors, such as BMI, suggesting that the nutritional status of 25(OH)D can play an important role in lipid profile 3.
In this study, high prevalence of VDD and NAFLD was found in both groups. However, no statistically significant association was observed between the two groups. There are some findings which report that low concentrations of 25(OH)D are associated with more severe histological changes of NAFLD 7. VD may induce CYP3A4, an enzyme essential for the catabolism of bile acids, indicating a potential role in the absorption of lipids. Therefore, it is speculated that VDD can exacerbate nonalcoholic steatohepatitis, in part, through the regulation of the bioavailability of bile acids 10. The presence of HS, frequent in subjects with obesity, also contributes to the reduction of serum concentrations of 25(OH)D, since its formation depends on the hydroxylation of cholecalciferol in the liver 36.
A study developed by Cordeiro et al. (2017) showed high prevalence of serum 25(OH)D inadequacy in individuals with class III obesity, which worsens as the stage of liver disease progresses diagnosed by liver biopsy 37. The present study evaluated only the presence of what is considered as an early stage of NAFLD, without evaluating the staging of the disease, which can be considered to be a limitation of this study. This may have been an aspect that contributed to the absence of an association with VDD.
In this study, no relationship between VD and high blood pressure was observed in any of the groups evaluated. Blood pressure may be inversely associated with VD and the possible mechanisms include the activity of the renin-angiotensin-aldosterone system, the effect on the improvement in the endothelial function and prevention of secondary hyperparathyroidism 38.
Moreover, no association of VD with the diagnosis of MS in adolescents and adults was found. The results of other studies are controversial in relation to association between concentrations of 25(OH)D and MS 12,13.
Visceral obesity and insulin resistance appear to be the most important factors for developing MS. The accumulation of visceral fat is related to increased secretion of pro-inflammatory cytokines from the adipose tissue 39. VDR expression in visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) positively relates with VAT and SAT inflammation, while, surprisingly, as inflammation negatively interferes with insulin signaling, only VDR expression in VAT positively predicts impairment of glucose metabolism regulation in obesity, where dysregulation of its expression occurs in VAT 40. An association of VD was not found with the diagnosis of MS, but an association with HOMA-IR was found, which is related to the development of this syndrome.
High prevalence of deficiency and insufficiency of VD associated with metabolic changes, both in adults and adolescents with obesity, were observed. Considering that the time of exposure to obesity interferes with the progressive worsening of associated complications, we suggested that it is necessary to develop strategies for the prevention and control of obesity and for the fight against the inadequacy of the nutritional status of vitamin D.














