INTRODUCTION
Obesity is a global pandemic associated with increased mortality, morbidity and a poor quality of life 1. Many authors suggest an inverse relationship between the adverse effects of obesity and cardiorespiratory fitness (CRF) 2,3.
Many studies have linked CRF with insulin sensitivity in both healthy and obese subjects 4,5. At the same time, CRF has been described as an independent and strong predictor of insulin sensitivity 6. An adequate evaluation of insulin sensitivity and CRF gives us accurate information about the health status of this group of patients 7.
Oxygen maximal consumption (VO2max) is the gold standard in the evaluation of CRF. According to Fick's equation, the VO2max depends of stroke volume, heart rate and arteriovenous oxygen difference (a-vO2 diff) 8.
In turn, oxygen pulse (PO2) is defined as the total oxygen amount that can be extracted by the peripheral tissue in every heart beat 9 and has been inversely related to mortality risk in a more sensitive way than peak oxygen consumption in median age adults with cardiac insufficiency 10. In turn, the oxygen pulse (PO2) is defined as the total oxygen amount that can be extracted by the peripheral tissue in every heart beat 9. PO2 has been inversely related with a higher sensitivity to mortality risk over the peak oxygen consumption in median age adults with cardiac insufficiency 10. PO2 is the product between stroke volume and a-vO2 diff, therefore, in patients with cardiovascular disease it has been used as an indirect indicator of the stroke volume in maximal exercise intensities 11,12, assuming a normal arterial concentration of oxygen and a normal a-vO2 diff 11. We propose that in subjects with normal values of stroke volume, the alterations in PO2 could be an indicator of an impaired a-vO2 diff.
VO2max and PO2 depend on central and peripheral cardiovascular parameters. In the case of the VO2max the individual contribution of these variables is impossible to distinguish. However, if we assume a normal stroke volume, PO2 could indicate a peripheral alteration of a-vO2 diff, providing information about the metabolic compromise, evaluated through insulin sensitivity.
The goal of the present study is to evaluate the relation between PO2 and IR in sedentary women with obesity.
MATERIALS AND METHODS
STUDY DESIGN
This was a retrospective study approved by the Ethics Committee with a waiver of the need to obtain informed consent (register 15-267). All participants' data was obtained from our database at Obesity Treatment Center according to inclusion/exclusion criteria.
PATIENTS
Fifty-five women who met the criteria shown in Figure 1, which were selected in a non-probabilistic way, were identified.
BODY COMPOSITION
Height was measured with a stadiometer (0.5 cm precision) and weight with a Seca® digital scale (0.1 kg precision). Both assessments were performed without shoes and in light clothing. Body mass index (BMI) was calculated as weight∙height-2 (kg∙m-2). Lean and fat mass, in kilograms, was assessed by using octopolar multi-frequency bioimpedance (InBody 720®) in a four-hour fasting state, without menstruation and with at least 12 hours free of exercise.
CARDIORESPIRATORY FITNESS
An incremental cycle ergometer test was performed with gas analysis (Metalyzer 3B-R2, Cortex®). The participants were free of exercise, alcohol, coffee, drugs or other stimulant consumption in the previous 24 hours and in a six-hour fasting condition. Theoretical maximal load (Wt) was estimated by the Jones equation in watts 13. Protocol consisted of a three-minute rest period, then a three-minute warm up at 20% of Wt, followed by six-minute stages at 30, 40, 50 and 60% of Wt until a respiratory exchange ratio (RER) ≥ 1 was reached. Then one-minute stages were performed with an increase 10% of Wt until exhaustion. Verbal stimuli were allowed. The test was considered as maximal if a RER ≥ 1.1 was reached and/or if the maximal heart rate (HRmax) was greater or equal to the theoretical maximum predicted by the Morris equation for an ergometer cycle test 14. This protocol was adapted from the one proposed by Brun, Romain and Mercier 15. The next variables were calculated from the average of the final 30 seconds from the last completed stage (breath by breath): HRmax in beats∙min-1, maximal load in Watts (Wmax), maximal load expressed as a percentage of Wt (Wmax(%)) and relative to body weight in watts∙kg (Wmax rel).
The same methodology was used for determining CRF from the measurements of VO2max. This was expressed as an absolute value in l∙min-1 and as a percentage of the maximum estimated (VO2max(%)), according to the Wasserman and Hansen weight algorithm 16. The peak oxygen pulse (PO2) expressed in ml∙beats-1 and calculated as VO2max∙HRmax-1, PO2 relative to corporal weight (PO2rel) calculated as PO2∙weight-1 and the PO2 relative to lean mass (PO2rel lm) calculated as PO2∙lean mass-1, both expressed in ml∙kg∙beats-1. All percentage variations were calculated considering 100% of the group was non-insulin resistant (non-IR).
INSULIN RESISTANCE
The homeostatic model assessment of insulin resistance (HOMA-IR), proposed by Mathews et al. 17, was used. Patients were considered as IR if they had a HOMA-IR value greater or equal to 2.5 according to the existent literature 18,19.
STATISTICAL ANALYSIS
The sample was categorized into two groups according to the presence of IR (IR group and non-IR group). Distribution of the variables was assessed using the Kolmogorov-Smirnov test. Variables with normal distribution are presented as mean and standard deviation and those without normal distribution are shown as median and 25-75 percentile. For comparing means between both groups a Student's t-test for independent samples was used. In variables with normal distribution and in non-normally distributed variables, a Wilcoxon test was used. Since all the variables to be correlated had a non-parametric behavior, a Spearman correlation coefficient was used for correlations. For association of IR with oxygen pulse, a stepwise logistic regression analysis was performed, adjusted by age and BMI accordingly.
Data is presented as odds ratio and confidence interval of 95%. Goodness of fit was evaluated with a Hosmer-Lemeshow test. The significance level was set as < 0.05. Statistical analysis was performed with the computational statistics program STATA 12 (Stata Corp., College Station, TX).
RESULTS
BODY COMPOSITION
IR group presents a higher weight (81.5 [78.4-88.8] vs 73.4 [69.1-80.8] kilos, p = 0.004), BMI (32.8 [30.3-34.8] vs 29.0 [27.7-31.5], p = 0.001), fat mass (39.3 ± 7.5 vs 32.9 ± 8.3, p = 0.002) and body fat percent (46.7 ± 4.9 vs 42.8 ± 8.6, p = 0.020), and a lower lean mass percentage with respect to body weight (50.2% [46.8-53.1] vs 53.9% [51.7-57.4], p = 0.004) in contrast to the non-IR group. No differences were found between both groups in height (158.9 ± 5.7 vs 161.1 ± 7.6 cm, respectively) and in fat free mass (40.7 [39.3-45.9] vs 40.9 [37.8-44.1] kg, respectively).
INSULIN RESISTANCE
The IR group showed higher values of HOMA (4.1 [3.2-5.8] vs 2.1 [2.0-2.5], p < 0.001), fasting glycaemia (87 [83-94] vs 84 [82-89] mg/dl, p = 0.044) and fasting insulinemia (19.2 [15.0-28.9] vs 10.2 [8.9-11.9] mg/dl, p < 0.001) in contrast to the non-IR group.
CARDIORESPIRATORY FITNESS
Table 1 shows differences in CRF between both groups. The VO2max% was a 7.1% lower in the IR group. At the same time, the PO2rel and the PO2rel lm were lower in the IR group in a 12.7% and a 6.5%, respectively. A negative correlation between HOMA-IR and PO2rel was also found (Fig. 2) in all the subjects. Table 2 shows logistic regression models for association of IR with PO2, PO2rel and PO2rel lm, adjusted by age. Models b) and c) were statistically significant and both are valid according to Hosmer-Lemeshow goodness of fit test (p = 0.446 and p = 0.289, respectively).
Table I. Cardiorespiratory fitness

VO2max: maximal oxygen consumption; VO2max(%): percentage of the theoretical maximum oxygen consumption; HRmax: maximal heat rate; PO2: maximal oxygen pulse; PO2rel: maximal oxygen pulse relative to weight; PO2rel lm: maximal oxygen pulse relative to lean mass; Wmax: maximal workload; Wmax%: percentage of the theoretical maximum workload. Wmax rel: maximal workload relative to weight. Values are expressed as mean (±) standard deviation.
*Student's t-test for independent samples: p < 0.05.
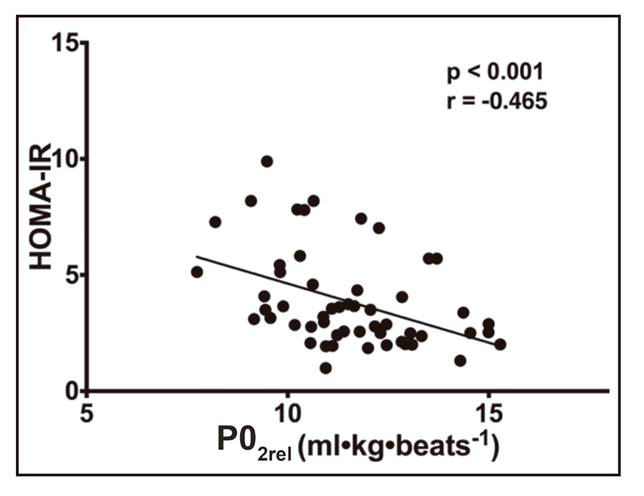
Figure 2. Correlation between insulin sensitivity (HOMA-IR) and oxygen pulse relative to weight (PO2rel) in all subjects.
DISCUSSION
In this study it was found that patients with insulin resistance had lower values of PO2 relative to weight and lean mass. In addition, an association between these variables was observed that could indicate a possible protective role against IR.
Several studies have shown that patients with higher weights and BMI have higher stroke volumes 20,21. From this, if we consider that PO2 depends directly on stroke volume and a-vO2 diff (peripheral oxygen extraction during exercise) 8,9, the IR group (with higher weight and BMI) should have had higher PO2 values. However, this was not the case and, when normalized by weight or fat free mass, the IR group presents lower values in comparison to the non-IR group.
The above could be explained considering that peripheral metabolic compromise is capable of nullifying the possible impact of stroke volume increase (related to weight) on PO2, so there are no differences in net values. At the same time, if the values of PO2 are normalized by weight or fat free mass, the impact of these variables on stroke volume and, in turn, on PO2 are annulled, allowing to detect the impact of peripheral metabolism on this variable.
There are some articles that have related the decreases in muscle mitochondrial oxidative capacity with the decreases in muscle insulin sensitivity 22 23 24-25. These variations in mitochondrial metabolism could explain the decreases in peripheral oxygen utilization during exercise, although more studies are needed to verify this relationship.
From these results, PO2 relative to weight or to fat free mass could be a useful parameter to estimate the peripheral metabolic status in patients with overweight and/or sedentary, whenever no stroke volume alterations exist. Further studies are necessary to elucidate the factors that allow us to differentiate the physiopathological context in which the PO2 is a better reflex of the stroke volume or of the arteriovenous oxygen difference.
One of the main limitations of the study is the utilization of HOMA-IR instead of the hyperinsulinemic euglycemic clamp, which is considered as the gold standard for the determination of IR. In addition, it is necessary to evaluate the arteriovenous oxygen difference and stroke volume in these patients for a better understanding of the impact of these variables in the IR diagnosis. For future studies, it would be interesting to consider the variation in time of PO2 and IR and to relate the variations of both variables after an exercise intervention.
CONCLUSION
In conclusion, this study demonstrates a relation between IR and PO2. Our results suggest that PO2 could be a protective factor against insulin resistance. Further studies should be oriented to the treatment of IR through improvement in peripheral variables of physical fitness, such as PO2. The evaluation of the impact of exercise in the PO2 variations and their relationship with the improvements on insulin sensitivity is necessary.
















