INTRODUCTION
Swallowing difficulties are common in the elderly, especially among institutionalized people. Half of institutionalized individuals are estimated to suffer from oropharyngeal dysphagia (OD) (1,2). Malnutrition is one of the main consequences associated with OD. Although prevalence rates vary depending on the method used, over half of the institutionalized elderly are malnourished or at risk of suffering malnourishment (3,4). Besides, approximately 80 % of pneumonia cases in elderly people with swallowing disorders correspond to cases of aspiration pneumonia, one of the leading causes of death in this cohort (5).
Between 26 % and 67 % of the meals served in geriatric nursing homes are texture-modified diets (TMD) (6,7). The in-home production of TMD (hTMD) requires blending the food and then diluting it with water or broth, thus reducing its nutritional intake (8-11), and increasing variability between prepared meals (11). Up to 83 % of patients receiving hTMD do not meet the necessary nutritional requirements, leading to nutritional deficiency (12,13). Recently, the European Society for Clinical Nutrition and Metabolism (ESPEN) recommends providing enriched TMD to support adequate dietary intake in elderly with malnutrition or at risk of malnutrition and with signs of OD (14). Concentrated nutrient-dense commercial food products (cTMD) for adults with OD provide a suitable alternative to hTMD. Caloric and protein intake is significantly increased by cTMD, which improves the nutritional status of the patient (12,15,16).
It should be borne in mind that the high amount of handling required to prepare hTMD meals increases the risk of food poisoning (17-19), and is also labor-intensive, requiring significant investment in resources and time spent by the kitchen staff.
There are currently automatic food mixers that can automatically prepare cTMD (cTMD-Mix), with the potential to significantly increase time and resource savings, and to minimize microbiological risks.
Although there are studies that describe the nutritional differences between hTMD and cTMD, as far as we know this is the first study to evaluate the resources and costs associated with TMD preparation. This observational study aims to describe the nutritional, microbiological properties, and the cost of three types of TMD: hTMD, cTMD, and cTMD-Mix.
METHODOLOGY
STUDY DESIGN
A proof-of-concept study with a descriptive, observational design was carried out in three geriatric nursing homes. The nursing homes were selected based on: 1) availability of own kitchen (not an external catering service); 2) cook with experience in the preparation of TMD ≥ 6 months; 3) experience of the specialist prescribing the diet ≥ two years.
In each of the nursing homes TMD was prepared using a method according to its routine practice: 1) in-home TMD (hTMD); 2) concentrated nutrient-dense commercial food products (cTMD); 3) cTMD-Mix prepared using the MixxPro® automatic food mixer to produce blended meals (cTMD-Mix).
The study was led by a committee of four experts (an endocrinologist, a catering manager, a bromatologist, and a food technologist) who participated in preparing the Case Report Form (CRF) and in the correct interpretation of study results.
PATIENTS
The study included patients ≥ 65 years of age, who were receiving TMD at the start of the study, with a stable clinical condition and an estimated survival > 1 month, with an expected internment ≥ 30 days, with sufficient cognitive capacity to complete the questionnaires (as assessed by the specialist prescribing the diet) either alone or with the help of a caregiver, and who were not participating in any other clinical trial. The study excluded those patients who required a change in diet (oral, enteral, or parenteral) for more than two days.
The participants were identified by the healthcare professional who prescribed the TMD following a consecutive, non-random recruitment. Patients were followed up for 15 days.
The following tests were conducted for each participant: nutritional screening using the Mini Nutritional Assessment Short Form (MNA®-SF) (at baseline), risk of dysphagia assessment using the Eating Assessment Tool (EAT-10) (at baseline), and appetite determination using the Short Nutrition Assessment Questionnaire (SNAQ) (before the main course). Data of symptoms associated with swallowing during feeding (choking, fractional swallowing, throat clearing, coughing during and after ingestion) were also collected at each meal.
PREPARATION OF TEXTURE-MODIFIED DIETS (TMD)
For all three TMD types, the preparation methods of the meal's main course were evaluated for five different varieties: chicken, veal, fish, egg, or lentils.
The hTMD was prepared using traditional processing methods and further blending. The cTMD was based on Meritene® (Nestlé Health Science) commercial products in the instant puree range (chicken with rice and carrots, veal with vegetables, fish with rice, puréed eggs Provenzal style, and lentils with vegetables). This range of dehydrated products was reconstituted with water, either manually (cTMD) or mechanically using a MixxPro® automatic food mixer (cTMD-Mix).
STUDY VARIABLES
Four independent CRFs were designed to collect the study variables: 1) to be filled in by the specialist prescribing the diet, recording the patient's main socio-demographic and clinical variables; 2) to be filled in by nurses or healthcare assistants, collecting data on compliance and symptoms related to dysphagia occurring during the meal; 3) to be filled in by the patient, including data on appetite; and 4) to be filled in by the catering manager, including information on the kitchen and the resources used to prepare each diet variety (Table I).
Table I. Variables collected during the study; source and time of collection

*The time required for cleaning was estimated based on the time required to clean each utensil (by hand or machine) and the number of utensils used during the preparation of each diet variety.
The staff responsible for data collection received appropriate training in person. Additionally, if the staff required it, online training was available during the study.
An external laboratory conducted the microbiological and nutritional (estimation of kcal per portion) analysis.
STATISTICAL ANALYSIS
Data were analyzed with the STATA statistical package, version 14. The absolute and relative frequencies of qualitative variables were calculated. The mean, standard deviation (SD), and interquartile ranges were calculated for the quantitative variables.
The compliance of each patient was calculated based on: 1) the amount of TMD served during the 15 days: mean amount served (according to the five cooking records) x 15 days; and 2) the average compliance of the patient during the 15 days of follow-up data recorded in the nursing questionnaire.
The average calorie count per portion was obtained based on the average number of calories per portion, and the average amount served per portion. The mean number of calories consumed per portion was calculated from the mean calories served per portion, and the mean compliance.
The costs related to food preparation were calculated on the following basis: 1) the cost of each of the ingredients used (€/kg, €/volume, or €/unit) according to the reference prices on the wholesale markets (20-23) or to the prices of origin; 2) the cost of human resources required for each of the processes - pre-processing, processing, blending (if applicable), homogenization (if applicable), and cleaning) - based on the time spent on each process, number of employees and wages (according to professional category (24,25) and updated to €/2019 in line with the CPI (26)); and 3) the number of portions prepared.
The time spent cooking, baking, frying, grilling, and blending/homogenizing was considered to calculate energy costs. For each process, the cost/hour was applied based on electricity or gas energy consumption, estimating the average cost of the corresponding energy supply at the time of the data analysis (27,28). Given the variability extant in the energy used by different types of blenders, a conservative 200 W value was applied. For instance, for the MixxPro® automatic food mixer, a maximum consumption of 2000 W was assumed, and a working time of 1 min per portion. Gas consumption was calculated by means of a direct extrapolation of the minutes recorded and energy consumption. The same energy tariffs were applied to all three centers, and similar appliances were assumed to have the same energy consumption.
The amount served per portion in each center was different, so the standardized cost per 100 g was calculated as follows: cost/100 g = 100 g x cost per portion [€/portion / amount served per portion (g). Based on this result, the average cost per 100 g was obtained for each menu.
The average cost per 100 kcal portion was obtained from the average calories served per portion, and the cost per portion.
ETHICAL CONCERNS
The study was approved by the Clinical Research Ethics Committee at the Complejo Asistencial Universitario de León (E. OBS1676), and was conducted according to the principles of the Helsinki Declaration and good clinical practice (GCP). Patients were informed about the study and signed an informed consent. The data were duly anonymized.
RESULTS
PATIENT CHARACTERISTICS
Of the total number of patients starting the study (n = 64), two were excluded: one did not adjust to the diet, and one died. Finally, 62 patients, 65 % women, with a mean age of 88.3 (SD: 9.3) years completed the follow-up and were included in the analysis (hTMD, n = 20; cTMD, n = 20; and cTMD-Mix, n = 22). Only 3.2 % of participants were well nourished (MNA®-SF ≥ 12). Baseline patient characteristics are shown in table II.
Table II. Baseline characteristics of study patients
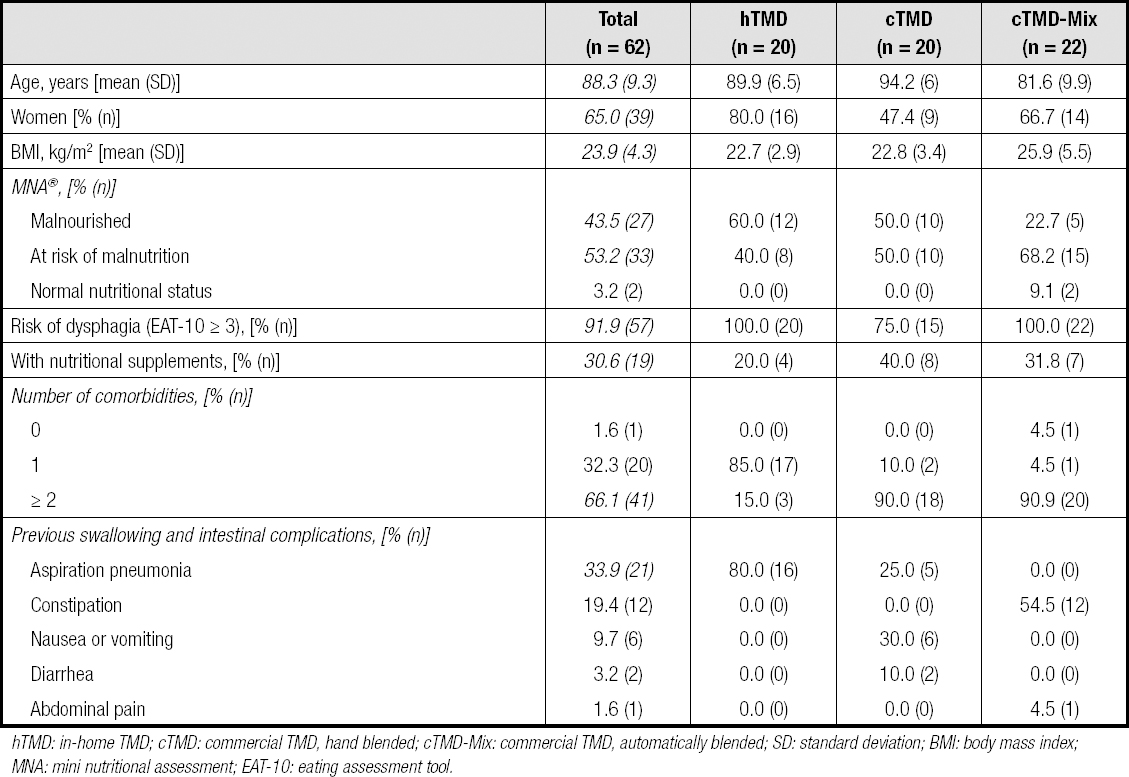
hTMD: in-home TMD; cTMD: commercial TMD, hand blended; cTMD-Mix: commercial TMD, automatically blended; SD: standard deviation; BMI: body mass index; MNA: mini nutritional assessment; EAT-10: eating assessment tool.
A total of 79.0 % of patients had a good appetite (SNAQ ≥ 14 points) during follow-up [hTMD: 100.0 %; cTMD: 75.0 %; cTMD-Mix: 63.6 %].
Overall, compliance with the diet was good. On average, the proportion of food eaten was above 80 %: hTMD: 95.5 % (SD: 10.7); cTMD: 89.2 % (SD: 15.9); cTMD-Mix: 80.3 % (SD: 21.4). Regarding compliance and the mean amount served per portion, patients receiving hTMD, cTMD, and cTMD-Mix ingested a daily mean of 197.7 g (SD: 21.6), 284.6 g (SD: 49.6), and 281.9 g (SD: 73.4), respectively. Similarly, considering the calories served, the calories consumed per portion were 88.2 (IQR: 72.2-122.3) for hTMD; 288.5 (IQR: 253.5-325.1) for cTMD; and 287.5 (IQR: 276.2-298.8) for cTMD-Mix.
The mean number of symptoms associated with swallowing during feeding (choking, fractional swallowing, throat clearing, coughing during and after ingestion) was 68 (hTMD), 46 (cTMD), and 10 (cTMD-Mix) for every 100 meals served, respectively.
CHARACTERISTICS OF PROCESSED MEALS
The average number of TMD served per portion, as well as the energy intake, differed in the three nursing homes: 207.0 g (SD: 9.0) and 92.4 kcal (IQR: 75.6-128.1) for hTMD; 319.2 g (SD: 35.4) and 323.4 kcal (IQR: 284.2-375.3) for cTMD; and 351.0 g (SD: 0.0) and 358.0 kcal (IQR: 344.0-372.1) for cTMD-Mix (Fig. 1). Greater variability was observed for those meals requiring higher levels of food handling for their processing: 56.1 % (hTMD), 26.1 % (cTMD), and 7.8 % (cTMD-Mix).
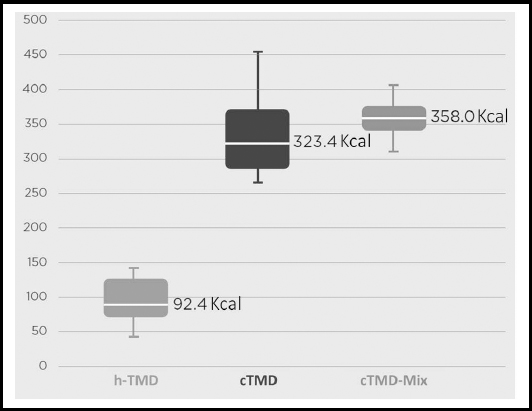
Figure 1. Kilocalories served per ration: interquartile ranges (hTMD: in-home TMD; cTMD: commercial TMD, hand blended; cTMD-Mix: commercial TMD, automatically blended).
The mean temperature of meals after blending was 80.6 °C (SD: 1.6) for hTMD, 88.2 °C (SD: 1.02) for cTMD, and 85.0 °C (SD: 0.0) for cTMD-Mix; while at the time of serving to patients, it was 54.3 °C (SD: 1.22) for hTMD, 58.7 °C (SD: 0.31) for hTMD, and 75.0 °C (SD: 0.0) for cTMD-Mix.
No microorganisms were detected in any of the analyzed samples.
USE OF RESOURCES AND COSTS ASSOCIATED WITH FOOD PREPARATION
The number and type of kitchen employees involved in food preparation varied between nursing homes (Table III).
Table III. Use of resources and time spent in meal preparation

hTMD: in-home TMD; cTMD: commercial TMD, hand blended; cTMD-Mix: commercial TMD, automatically blended; SD: standard deviation; Min: minutes.
In each kitchen, 69 % (hTMD), 81.8 % (cTMD), and 53.8 % (cTMD-Mix) of the total number of prepared meals (including non-blended types) were TMD. The mean number of portions prepared during the study period was 28.8 (SD: 2.9) for hTMD, 26.0 (SD: 1.4) for cTMD, and 70.0 (SD: 0.0) for cTMD-Mix. The average time spent in preparing each portion was 11.2 min (SD: 3.89) for hTMD, 1.7 min (SD: 0.28) for cTMD, and 1.6 min (SD: 0.00) for cTMD-Mix (Table III).
The total cost per portion (human resources, ingredients, and energy consumption) amounted to €2.33 (SD: 0.63), €2.01 (SD: 0.39), and €2.00 (SD: 0.33) for hTMD, cTMD, and cTMD-Mix, respectively. In the nursing home employing hTMD the main cost component was associated with human resources, whereas in the centers using cTMD and cTMD-Mix the main cost was related to raw materials (Fig. 2).

Figure 2. Breakdown of cost per ration (hTMD: in-home TMD; cTMD: commercial TMD, hand blended; cTMD-Mix: commercial TMD, automatically blended).
The average cost per 100 g was €1.12 (SD: 0.29) for hTMD, €0.65 (SD: 0.18) for cTMD, and €0.57 (SD: 0.09) for cTMD-Mix. Finally, the average cost per 100 kcal was €2.80 (SD: 1.32) for hTMD, €0.62 (SD: 0.18) for cTMD, and €0.58 (SD: 0.13) for cTMD-Mix.
DISCUSSION
TMD is recommended for patients who have difficulty swallowing. To facilitate its intake, the texture of the original food is modified by blending, and very often water or broth is added, which can lead to nutritional deficiency in the prepared meal and greater variability between portions (15). In line with previous studies (11), our work has demonstrated a lower energy intake and a higher variability associated with hTMD meals.
The need to blend food to adapt it to a patient's swallowing requirements can also modify its organoleptic qualities and be associated with suboptimal intake (8,29). In our study, the percentage of food eaten, as compared to food served, was high (> 80 %), and it was higher in patients receiving hTMD than in those receiving cTMD or cTMD-Mix. However, this difference may be accounted for because the portions served in the nursing homes serving hTMD (approximately 200 g) were smaller than those served in the centers offering commercial diets (approximately 350 g). In fact, the total amount of ingested foor per portion was about 30 % higher in the homes serving commercial meals. This fact, together with the lower caloric intake of hTMD, could diminish the feeling of fullness, and explain the greater appetite observed in patients with hTMD. Similarly to our study, Rubio et al. compared the intake of an hTMD with a hyperproteic and hypercaloric powdered preparation (cTMD), observing that the total amount ingested by the patient was lower in the cTMD group, with a higher energy and protein intake (30). Other studies have described that in both institutionalized elderly patients and elderly outpatients with swallowing difficulties, a higher energy and protein intake was achieved with cTMD as compared with hTMD (31,32). Similarly, our results show that, although compliance was higher in the nursing home with hTMD, the final kilocalories ingested were much higher in the patients receiving cTMD or cTMD-Mix than in the patients receiving hTMD.
Another reason for prescribing TMD is to reduce the risk of choking and prevent aspiration pneumonia. Up to 70 % of institutionalized people may suffer from choking during meals (33). Evidence of symptoms related to swallowing (such as choking) associated with hTMD vs. cTMD is minimal; moreover, results on the effectiveness of TMD to prevent aspiration pneumonia are inconclusive (34,35). In the present study, the number of swallowing-related symptoms observed was higher in patients receiving hTMD, decreasing with the diets requiring lower levels of manipulation during preparation, as was the case of cTMD-Mix. These results would be consistent with the fact that patients with hTMD reported more aspiration pneumonia (before study initiation) than patients receiving cTMD and cTMD-Mix. However, due to the study's nature, these results are neither representative nor conclusive enough to establish a cause-effect relationship.
During diet elaboration, food needs to reach a temperature above 65 °C, and should not be exposed to temperatures between 15 °C and 45 °C to guarantee microbiological safety (12). The three types of diet studied showed a good safety profile. In all cases, microbiological safety temperatures (> 65 °C) were reached during preparation, and the presence of microorganisms was not detected in the analysis. It should be noted that only cTMD-Mix remained above 65 °C until the time of serving.
As far as we know, this is the first study conducted in geriatric nursing homes to evaluate the use of resources and costs of TMD production for patients with dysphagia or mastication difficulties using natural and commercial foods, and three different processing methods ( (hTMD, cTMD, cTMD-Mix).
Raw material costs were lower for hTMD when compared to cTMD and cTMD-Mix. However, the time required to prepare each portion was much lower in the latter. Approximately, 1.5 minutes for commercial diets and 11 minutes for hTMD were required. Considering the resources needed to prepare the diets, the cost per portion and the cost per 100 g served were lower for the commercial diets than for the home-made ones.
Previous studies suggest that patients who switch from hTMD to fortified TMD (13,31) or cTMD (32) experience significant weight gain improvements. Additionally, two observational studies showed that cTMD-Mix was a simple and effective way to improve nutritional status in elderly institutionalized residents with swallowing disorders (36,37). The scope of our study was not to assess the nutritional status of patients. Considering that most of our participants were already receiving TMD before the study started, our results appear to be in line with the above studies. In this respect, the percentage of patients with malnutrition was higher in the nursing home serving hTMD and lower in the nursing home serving hTMD-Mix.
Our study presents some limitations. The first one relates to the study population, as patient recruitment was made according to convenience, and the number of participants was relatively low, preventing a robust statistical analysis. Despite the small sample size, since study participants include elderly residents with a high level of dependence, we can assume that the study population is representative of nursing home residents. Similarly, the study involved a reduced number of kitchens, each one with specific characteristics and peculiarities, so their practices may not be representative. However, it is important to keep in mind that the study objective was descriptive rather than comparative. Some participants might have required help to eat; however, since such data were not collected, it cannot be established whether having support influenced the amount of food consumed. Finally, since the nursing home staff collected the data, there may be inter-staff variability in measurements. In order to reduce this possible bias, the staff responsible for data collection received appropriate training, both in person and online; a graduated scale widely used in observational studies was used to assess the amount ingested; only objective symptoms related to dysphagia disorders such as choking, fractional swallowing, throat clearing, coughing during and after ingestion were reported. Despite these limitations, the study provides useful information for future analyses of the potential benefits and costs of TMD as prepared using different processes.
In conclusion, in patients with dysphagia and/or chewing difficulties, concentrated, nutrient-dense food products (Meritene®, Nestlé Health Science), particularly those produced using the MixxPro® automatic food mixer, ensure a high caloric intake, even in subjects with lower compliance rates. Moreover, they allow quick and safe food preparation, reducing both kitchen workload and production costs. Further studies with a larger sample of patients and centers are needed to obtain representative results and establish whether there is any cause-effect of such diets on patient nutritional status.














