INTRODUCTION
Approximately, 30 % of children and 60 % of adults worldwide are estimated to have vitamin D deficiency (1). In Mexico, studies on newborns and infants report a prevalence of vitamin D deficiency of 23 % to 98 % (2-4). Infants are vulnerable to vitamin D deficiency because they depend on maternal reserves, which last eight weeks on average (5); they usually have less exposure to sunlight (6); and breastmilk is low in vitamin D, indicating that exclusively breastfed infants, with no vitamin D supplementation, are at higher risk (7).
Vitamin D receptors can be found in more than 36 tissues in the human body, including the endothelium and vascular smooth muscle. Additionally, vitamin D is involved in the activation and regulation of more than 200 genes affecting different systems of the human body, including the cardiovascular system (8,9). The presence of cardiovascular risk factors (abnormal blood lipids, high BMI, high intima-media thickness, among others) in early life can predict and enhance the onset of cardiovascular disease in adulthood (8,10,11). Different studies have already identified an association between low levels of 25(OH)D and cardiovascular risk factors in children and adolescents (12-14). Because vitamin D deficiency during human growth and development can affect the cardiovascular system, and infants are at higher risk for vitamin D deficiency, the primary aim of the present study was to identify whether there is a correlation between serum 25(OH)D levels, blood lipids, and aortic and carotid intima-media thickness in infants aged 3 to 9 months. Our secondary aim was to evaluate the correlations between vitamin D and blood lipids, according to feeding method.
MATERIALS AND METHODS
A cross-sectional study was conducted in 129 healthy, full-term infants of both sexes, between 3 and 9 months of age, who had their routine check-ups at the Regional University Hospital in Colima, Mexico, between March and December 2019. The infants were included by convenience sampling, when the parents agreed to participate. Twenty infants were excluded because they left the study. Infants that were premature, had low birth weight, or presented with congenital heart disease or endocrine disorders were not included. An ad hoc questionnaire was applied by the lead researcher to obtain information on feeding method (exclusive breastfeeding, breastmilk substitutes, or partial breastfeeding), vitamin D supplementation, and the infant's exposure to sunlight.
The study variables were total cholesterol, HDL-cholesterol, non-HDL-cholesterol, aortic intima-media thickness (a-IMT), and carotid intima-media thickness (c-IMT). Weight was measured on a pediatric scale (SECA), with as little clothing as possible, and length was measured to the nearest 0.5 cm on a portable infantometer (Pharma-Insight). BMI/Age Z-score was obtained through the WHO Anthro software, version 3.2.2 (Department of Nutrition, WHO). Sun exposure was assessed by the solar index (4,15), which is determined by the minutes of sunlight exposure per week multiplied by the percentage of body surface area (%BSA) exposed, based on the Lund and Browder chart (15). Infants were placed in the exclusively breastfed group if they were fed only breastmilk; into the partially breastfed group if they received breastmilk and any amount of a breastmilk substitute at the same time; and into the exclusively breastmilk substitute-fed group if they received no breastmilk and were fed only breastmilk substitutes.
A blood sample was collected by venipuncture from the dorsal area of the infant's hand and placed in a vacutainer tube with separating gel. It was then centrifuged at 1600 g to obtain the blood serum, which was frozen at -70 °C until measured. 25(OH)D was determined by the enzyme-linked immunosorbent assay (International Immuno-Diagnostics, Foster City, CA, USA), using a microreader (Bio-Rad Laboratories Inc, Shinagawa, Tokyo, Japan) for absorbances. The Endocrine Society cut-off points were used to classify 25(OH)D levels, considering deficiency at < 20 ng/mL, insufficiency at serum levels between 21 and 29 ng/mL, and sufficiency at ≥ 30 ng/mL (16). Total cholesterol and HDL cholesterol level determination was performed using a colorimetric enzymatic technique (Spinreact, CHOD-POD, Sant Esteve de Bas, Spain), and a spectrophotometer (Ultrospec 1000, Pharmacia Biotech Lt, Cambridge, England) to measure absorbances. Non-HDL-cholesterol determination was obtained by subtracting HDL-cholesterol from total cholesterol, taking < 120 mg/dL as the baseline values for children and adolescents, as established by the National Heart, Lung, and Blood Institute (10).
The a-IMT and c-IMT measurements were performed using B-mode high-resolution ultrasound equipment (H60, Samsung) with a 14-MHz linear transducer; a-IMT and c-IMT were assessed in 81.6 % of the total sample (89/109). The measurement was performed in a dark, temperature-controlled room with the infant placed in the supine position. The abdominal aorta was initially identified in the upper abdomen with a linear transducer, and then followed distally until the aortic bifurcation was reached. The a-IMT was measured in a straight, non-branched, 1-cm longitudinal segment of the more distal wall of the abdominal aorta (17-19). For c-IMT measurement, the proximal part of the carotid bulb of the right carotid artery was identified, and the closest 1 to 2 cm segment of the common carotid artery was scanned (20). The c-IMT was identified 10 mm below the distal wall of the common carotid artery, within 2 cm of the carotid bifurcation (21). All measurements were made by the same radiologist, who was unaware of the participants' 25(OH)D levels.
Data were reported in medians and interquartile ranges (25-75) due to the nonparametric distribution found when applying the Kolmogorov-Smirnov test. The comparison between groups was evaluated by the Mann-Whitney U-test and the Kruskal-Wallis test, as needed, whereas the chi-square test was used for qualitative variables. Spearman's correlation test was performed to assess the relationship between variables. Linear regression was used to confirm significant correlations. For all statistical analyses, a p-value < 0.05 designated a significant difference.
The protocol was approved by the Ethics Committee of the Regional University Hospital, with registration number CI/2018/02/CR/PED/066. In accordance with the Declaration of Helsinki, a written informed consent was obtained from the parents or legal guardians agreeing to participate in the study; participant privacy was protected, and data were handled confidentially.
RESULTS
A total of 109 infants from 3 to 9 months of age participated in the study; 50.5 % (n = 55) were girls and 49.5 % (n = 54) were boys. When classifying 25(OH)D levels according to the cut-off values suggested by the Endocrine Society, only 3 infants (2.8 %) had vitamin D deficiency, with a median of 17 ng/mL; 11 of them (10.1 %) had insufficiency, with a median of 26 ng/mL; and 87.1 % of participants (n = 95) had vitamin D sufficiency, with a median of 47 ng/mL.
Table I shows all the variables by comparing 25(OH)D levels as inadequate (deficient and insufficient) and adequate. It should be noted that 92.8 % of the infants with inadequate vitamin D levels were under 6 months of age. Only 30.3 % were exclusively breastfed, and merely a quarter of the total sample (25.7 %) took a vitamin D supplement. In addition, 39.4 % of breastfed infants were being supplemented with vitamin D.
Table I. All variables according to inadequate and adequate vitamin D levels
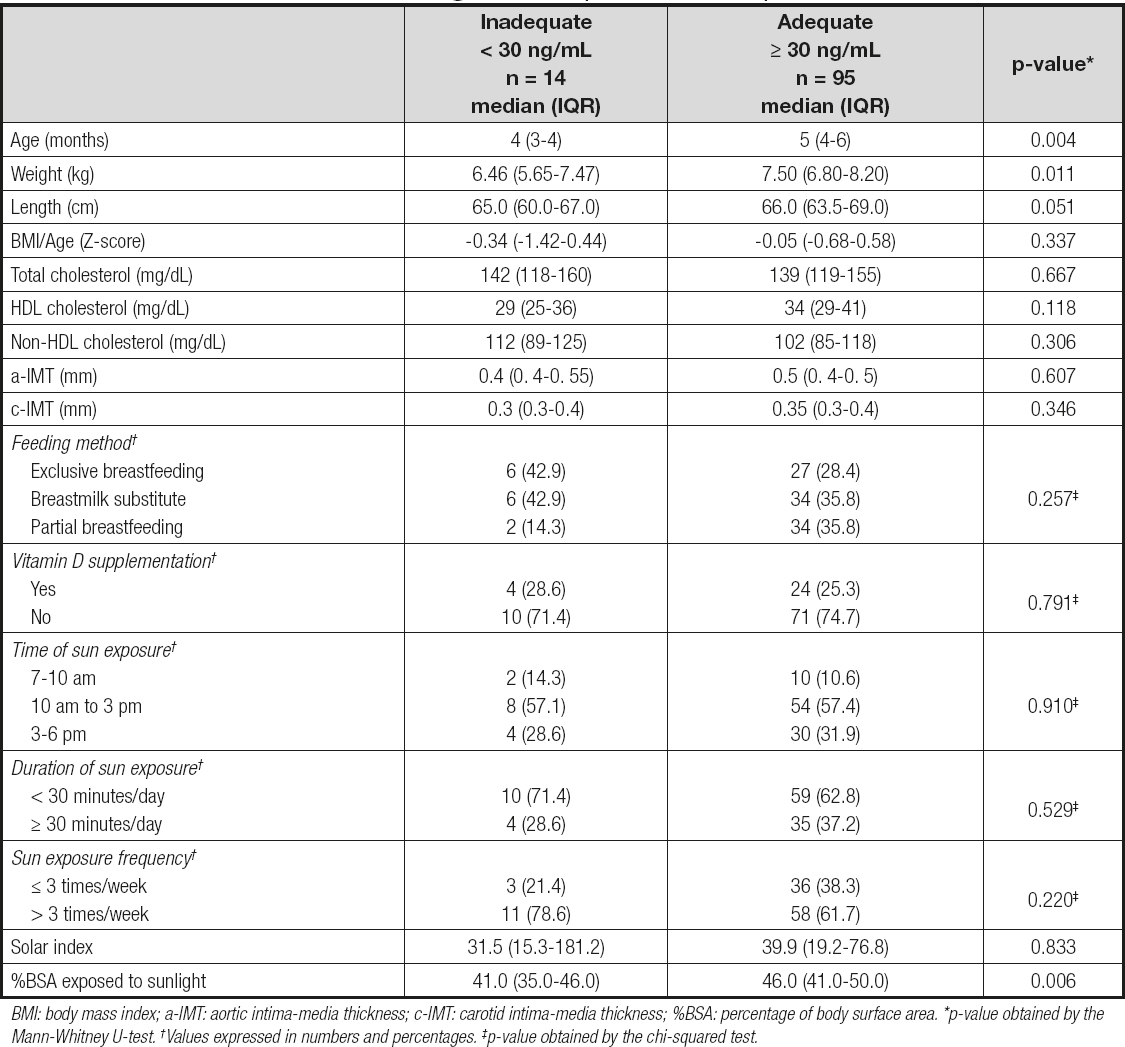
BMI: body mass index; a-IMT: aortic intima-media thickness; c-IMT: carotid intima-media thickness; %BSA: percentage of body surface area. *p-value obtained by the Mann-Whitney U-test. †Values expressed in numbers and percentages. ‡p-value obtained by the chi-squared test.
A positive and significant correlation between 25(OH)D levels and both total cholesterol (rho = 0.243, p = 0.011) and non-HDL-cholesterol (rho = 0.251, p = 0.009) was identified (Table II), but when those correlations were stratified by feeding method, the correlation between 25(OH)D levels and non-HDL-cholesterol only remained significant in the infants who consumed breastmilk substitutes (rho = 0.600, p < 0.001) or in those who were partially breastfed (rho = 0.371, p = 0.026); the correlation between 25(OH)D levels and total cholesterol was found only in the infants receiving breastmilk substitutes (rho = 0.618, p < 0.001); and a negative but nonsignificant correlation was found for total and non-HDL-cholesterol in the exclusively breastfed group [(rho = -0.235, p = 0.188) and (rho = -0.213, p = 0.234), respectively] (Figs. 1 and 2). A positive and significant correlation was also found between 25(OH)D levels and age, weight, length, and %BSA exposed to sunlight, whereas no significant correlation was found between 25(OH)D levels and a-IMT, c-IMT, or HDL-cholesterol (Table II). The linear regression model considered only the variables with a significant correlation and the feeding method, noting that only age and non-HDL-cholesterol were significant (Table II). When rerunning the model by the stepwise method, age (β = 0.350, p < 0.001) was a better predictor for vitamin D than non-HDL-cholesterol (β = 0.224, p = 0.013).

Figure 1. Correlation between 25(OH)D and total cholesterol levels, stratified by type of feeding. Spearman's correlation.

Figure 2. Correlation between 25(OH)D and non-HDL cholesterol levels, stratified by type of feeding. Spearman's correlation.
Table II. Binomial correlation between 25(OH)D levels and all the variables studied and the linear regression model with vitamin D as the dependent variable

a-IMT: aortic intima-media thickness; c-IMT: carotid intima-media thickness; BMI: body mass index; %BSA: percentage of body surface area; CI: confidence interval; β: beta standardized regression coefficient. Italic font indicates statistical significance.
DISCUSSION
In the present study we expected to find a negative correlation of serum 25(OH)D levels with blood lipids and both aortic and carotid intima-media thickness in the entire study group, but we found the opposite. There was a positive, statistically significant correlation between total cholesterol, non-HDL-cholesterol, and 25(OH)D levels. When analyzing the feeding method, said positive correlations were found in the infants that only received breastmilk substitutes or in those who were partially breastfed. In the group that was exclusively breastfed there was a negative correlation between total cholesterol, non-HDL-cholesterol, and 25(OH)D levels that was not statistically significant.
To the best of our knowledge, only two studies have evaluated the relationship between vitamin D and blood lipids in infants. Kew et al. (22) found no correlation between those variables in 12-month-old infants, whereas Arnberg et al. (23) found a negative correlation between total cholesterol and vitamin D in 9-month-old infants. The results of the study by Arnberg et al. were similar to ours with respect to the exclusively breastfed group, which had a negative correlation with total cholesterol and 25(OH)D levels that was not statistically significant. Neither of those studies measured non-HDL-cholesterol, nor did they compare correlations by feeding method.
Few studies have evaluated the relationship between vitamin D and a-IMT, an early marker of subclinical atherosclerosis that has been highlighted as a tool for assessing cardiovascular risk from the earliest stages of life. Some authors have reported that people with vitamin D deficiency and insufficiency have higher a-IMT values (20,24). A study conducted in Turkey by Arman and Çetiner (20) in healthy newborns found that those with severe (< 10 ng/mL) and moderate (11-20 ng/mL) vitamin D deficiency had higher means and maximum a-IMT values when compared to those listed as insufficient and sufficient, but no correlation with c-IMT was found. In the present study, the median value for 25(OH)D was 43 ng/mL, only three infants were classified as deficient, and none had severe deficiency. The relation between those variables was observed when vitamin D levels were very low or when deficiency was prolonged, which could explain why we found no negative correlation between a-IMT and 25(OH)D. On the other hand, the earliest pathological evidence of atherosclerosis presents in the abdominal aorta, whereas alterations in the carotid occur over a longer period (25). Therefore, the fact that there were no alterations in a-IMT explains the lack of an association between c-IMT and 25(OH)D, findings which are similar to those reported in the study by Arman & Çetiner (20).
A positive and significant correlation was found between vitamin D and age. Infants 6 months of age or older had a higher median value of 25(OH)D than those younger than 6 months. That is consistent with a study conducted in Japan, where younger infants (0-5 months) had significantly lower serum 25(OH)D levels than older infants (6-48 months), at 19 ng/mL vs 30 ng/mL, respectively. The authors also reported that younger infants had similar 25(OH)D levels throughout the year, unlike older infants, who had significantly higher levels of vitamin D during the summer and fall. Consequently, a possible explanation for that difference is lower exposure to sunlight in the younger group (26). Insufficient sun exposure and depletion of vitamin D reserves at around 3 months of age are factors that increase the risk of vitamin D deficiency in younger infants (6,27). Moreover, as infants grow, fortified solid foods and breastmilk substitutes are commonly introduced in the diet and are enriched with vitamins and minerals, including vitamin D (28). Therefore, those dietary patterns can contribute to older infants having higher serum 25(OH)D levels. Even though we found no significant differences between 25(OH)D levels and feeding method, infants that were fed with breastmilk substitutes and received vitamin D supplements had a higher median value of 25(OH)D (58 ng/mL) than infants who were exclusively breastfed, with or without vitamin D supplementation (42 ng/mL and 48 ng/mL, respectively).
To date, there are no vitamin D supplementation policies in Mexico during pregnancy, lactation, or infancy (2). However, infants aged 0 to 12 months should receive a daily supplement of 400 IU of vitamin D, regardless of feeding method, as is recommended by the European Academy of Paediatrics (29). However, only a quarter of our study sample consumed vitamin D supplements and 30 % of the infants were exclusively breastfed. Nevertheless, the frequency of vitamin D deficiency and insufficiency in the present study was low (2.8 % and 11.9 %, respectively).
In exclusively breastfed infants, Meena et al. (15) reported that exposing 40 % of their BSA to sunlight for at least 30 minutes per week was sufficient for reaching adequate levels of 25(OH)D. The participants in our study were exposed to sunlight over 46 % of their BSA, for a median of 90 minutes per week. Colima is a city characterized by a sub-humid warm climate, with an average annual temperature of 27.4 °C, unlike cities in Northern and Central Mexico (2-4) that have lower temperatures and a drier climate (30), with reports of vitamin D deficiency in infants. That could be a possible explanation for the low frequency of vitamin D deficiency and insufficiency in the present study. Despite their not receiving vitamin D supplementation, our study infants received sufficient sun exposure to maintain adequate levels of 25(OH)D.
Contrary to other studies (22,28,31,32), we found no association between 25(OH)D levels, feeding method, and vitamin D supplementation. The infants in our study that had a higher risk for vitamin D deficiency (exclusively breastfed infants) were either being supplemented or had adequate sun exposure, because the exclusively breastfed infants with no vitamin D supplementation had a higher sun index than those that were breastfed and supplemented (57.4 vs 25.2 ng/mL, p = 0.065).
The main limitations of the present study were the small size of the sample selected by convenience, the low prevalence of vitamin D deficiency and insufficiency, which limited group comparisons, and the cross-sectional design of the study, which prevented causality identification. Ours is the first study to evaluate the relation of blood lipids, a-IMT, and c-IMT to vitamin D levels in younger healthy infants in Mexico, as well as in Latin America, with adequate control of intervening variables, providing an overview of different factors that can affect serum 25(OH)D levels during the early stages of life.
In conclusion, a positive and statistically significant correlation between the levels of 25(OH)D, total cholesterol, and non-HDL-cholesterol was found in infants fed with breastmilk substitutes. In breastfed infants the correlation was negative, but not statistically significant. Perhaps the relation between lipid levels and 25(OH)D levels in infants who received breastmilk could be another protective factor against the development of chronic, noncommunicable diseases such as cardiovascular disease in later stages of life. Nonetheless, more studies are needed to clarify and corroborate those correlations.














