INTRODUCTION
The "developmental origins of health and disease" hypothesis explains that an adverse environment during a critical period of growth and development may have lifelong consequences on organ development and mental health status, and may increase the risk for certain non-communicable diseases (NCDs) in the mid and long term (1-3).
In 2015, 20.5 million newborns were registered worldwide, and 14.6 % of them had low birthweight (LBW < 2500 g). In that year in Mexico, it was estimated that 5-10 % of newborns had LBW (4). Furthermore, the incidence of high birthweight (HBW > 4000 g) varies across different regions of the world, depending on the cut-off value of minimum weight. Worldwide estimates range from 3 % to 10 % of all newborns, while in Mexico 4.8 % of newborns have HBW (7). Both LBW and HBW are risk factors for certain NCDs.
Currently, the association between birthweight, components of the metabolic syndrome (MetS) and mental illness remains controversial. Results are inconsistent, with some studies showing strong associations while others do not (6-20). Regarding birthweight and MetS, a recent cross-sectional study in Chinese and Spanish adolescents reported that HBW is associated with hyperglycemia, low high-density lipoprotein-cholesterol (HDL-C), hypertriglyceridemia, and abdominal obesity (7). HBW is associated with early development of insulin resistance, type-2 diabetes mellitus (T2DM), obesity, and MetS (6,7). Regarding high blood pressure, several studies have shown an inverse relationship between birthweight and blood pressure (BP) (8,9). LBW in combination with a positive family history for T2DM in the maternal branch is a risk factor for MetS, independently of weight status (6,10). Previous reports indicated a J-shape or U-shape relationship between birthweight and fat mass later in life (6).
A recent study indicates that LBW, used as a proxy for intrauterine growth retardation, is causally related to increased susceptibility to coronary artery disease and T2DM. The authors reported that this relationship was not mediated by adult obesity or hypertension (11). Also, childhood cardiometabolic risk exhibits specific patterns for race and gender. For example, birthweight and high waist circumference (WC) in black children follow a U-shaped relationship, as well as high systolic blood pressure (SBP) in Mexican and Hispanic children. LBW with high SBP and low HDL-C appears to be more prominent in boys, while an inverse association with high HbA1c is more evident in girls (12).
All these findings differ from those presented by Dos Santos et al., who reported that birthweight is not a risk factor for the development of MetS during adolescence (13), and those presented by de Rooij et al., where LBW is not associated with an increased prevalence of MetS in adulthood (14).
Few studies have evaluated the potential association between birthweight and mental illness. There is evidence that LBW increases the risk for psychiatric problems such as stress, major depressive disorder (MDD), and anxiety disorders when compared with infants weighing > 3500 g at birth (15). Other studies show a U-shape relationship between birthweight, mental disorders, and insomnia. HBW and LBW adolescents have a higher risk for mental problems and sleep disorders (6,16). A recent study refuted the hypothesis from observational studies about the association between birthweight and mental disorders with Mendelian randomization - a novel method that tests causality on the basis of genetic data (17).
Some studies show a correlation between mental problems and development of cardiovascular diseases (CVD) later in life (18,19). A recent study with primary care patients found that depression and anxiety disorders were associated with an increased risk for arterial hypertension, obesity, and hyperlipidemia (20).
To our knowledge, there is no data about the relationship between birthweight, depression, and CVD risk factors among Mexican young adults; therefore, we decided to investigate the possible association between these three variables in young adult students.
MATERIALS AND METHODS
STUDY POPULATION
Participants were selected from the 2009 UP AMIGOS cross-sectional study (Universities of San Luis Potosí and Illinois: A Multidisciplinary Investigation on Genetics, Obesity, and Social Environment). This was a cross-sectional study of young adults aged 17 years 6 months and one day to 25 years, applicants to a public university in Mexico, who were seeking admission for the 2010 school cycle between February and July of 2009.
As part of the university application process, all participants were submitted to a health screen at the university clinic. The health screen consisted of: 1) anthropometric measurements, including height, weight, WC, and BP; 2) a medical interview and physical exam conducted by a physician; 3) a blood draw following an overnight fast for biological markers; and 4) the self-reported depressive symptoms questionnaire Center for Epidemiological Studies Depression Scale (CESD-10) (21). Individuals willing to participate were apprised of study goals and their rights before signing the informed consent form. The Institutional Review Boards of both the Autonomous University of San Luis Potosí and the University of Illinois at Urbana-Champaign approved the study protocol.
Briefly, a total of 6,400 samples and valid questionnaires were collected. Only 778 were found to be eligible on the basis of the selection criteria with complete demographics, lipid profiles, and birthweight data. Birthweight was registered and categorized as < 2500 g, 2500 to 4000 g, and > 4000 g.
ANTHROPOMETRIC MEASURES
All measures were taken by trained health professionals at the university clinic. For all measurements, students were barefoot and wearing light clothes. Height was measured using a stadiometer to the nearest 0.5 cm, and weight was measured on a calibrated scale and recorded to the nearest 0.1 kg (Torino, Mexico). Weight and height were measured twice and the mean of the two values was reported. For the body mass index (BMI) calculation, weight (kg) was divided by the square height (m2) and classified in accordance with the World Health Organization's international classification: underweight (≤ 18.49 kg/m2), normal weight (18.50-24.99 kg/m2), overweight (25.00-29.99 kg/m2) and obese (≥ 30.00 kg/m2). WC was measured using a flexible, non-stretching nylon tape at the level between the last rib and iliac crest following normal expiration, with the subject in the standing position, and was recorded to the nearest 0.1 cm. WC risk level for MetS was determined according to the International Diabetes Federation (IDF)/American Heart Association (AHA) population- and sex-specific joint definition: at risk males (≥ 90 cm) and at risk females (≥ 80 cm) (22).
BLOOD PRESSURE
BP was measured by trained and certified healthcare providers according to a protocol adapted from the procedures recommended by the American Heart Association. BP was taken on the dominant arm after at least a 5-min rest while participants were in a sitting position. Arms were bare and supported at heart level, and we used appropriately sized Welch Allyn cuffs. According to the harmonized definition, high blood pressure was defined as SBP ≥ 130 mmHg and/or DBP ≥ 85 mmHg (22).
FAMILY HISTORY
The family history of CVD and T2DM was assessed during the medical interview, including family members (sisters, brothers, parents, grandparents) known to have the disease.
ASSESSMENT OF DEPRESSIVE SYMPTOMS
Participants completed the CESD-10 questionnaire. Items evaluate depressed affect, positive affect, somatic complaints, and interpersonal problems. In a previous Mexican study, the CESD-10 tool showed good psychometric properties with Cronbach's a = 0.72 (23). Participants rated how often they experienced each symptom during the past week using 4 response options from "Rarely or none of the time" (less than 1 day) to "All of the time" (5-7 days). Positive items were reversed, and responses assigned numeric values (0 to 3) before being summed. Possible scores range from 0 to 30, with a score of 10 or higher considered a positive screen for depression (21,24).
BIOCHEMICAL MEASUREMENTS
Blood samples were collected after an overnight fast (≥ 8 hours). All samples were measured in the Alcyon 300 autoanalyzer (Abbott, Illinois, USA, with reagents from BioSystems, Mexico). Fasting blood glucose (FBG) was determined according to the glucose oxidase peroxidase method. Impaired fasting glucose (IFG) was defined as a FG ≥ 100 mg/dL (22). Serum total cholesterol (TC), HDL-C, and triglycerides (TG) were determined by standard methods at the Clinical Research Laboratory, Chemistry School, UASLP in Mexico. Low-density lipoprotein-cholesterol (LDL-C) and very-low-density lipoprotein-cholesterol (VLDL-C) were calculated using Friedewald's equation. Hypertriglyceridemia was defined as a TG concentration ≥ 150 mg/dL, hypercholesterolemia as TC ≥ 200 mg/dL, high LDL-C as a concentration > 130 mg/dL, and low HDL-C was defined as ≤ 40 mg/dL in males and ≤ 50 mg/dL in females (25).
STATISTICAL ANALYSIS
Participants' general characteristics were categorized separately by birthweight category. A one-way analysis of variance (ANOVA) with post-hoc test was performed to evaluate significant differences in quantitative variables, and the c2 test was used for qualitative characteristics. Mean values for CV risk factors, such as serum lipid profile and glucose levels, as well as BP, were reported by using the ANOVA (post-hoc test) approach across the different categories of birthweight. Statistical analyses were performed using the SPSS for Windows software (version 26.0. SPSS, Chicago, IL, USA), and p-values < 0.05 were considered statistically significant.
RESULTS
The number of women and men included in the present study was 469 (60.2 %) and 309 (39.7 %), respectively. The means and standard deviations (SDs) of general characteristics, CESD-10 scores, and family history across birthweight categories are shown in table I. Both groups with birthweight > 4000 g had the highest amount of weight and BMI (p < 0.05). No significant relationships were found between CESD-10. However, a significant relationship was found only for WC in men and for height in women.
Table I. General characteristics, CESD-10 score, and family history of participants according to birthweight (g) categories
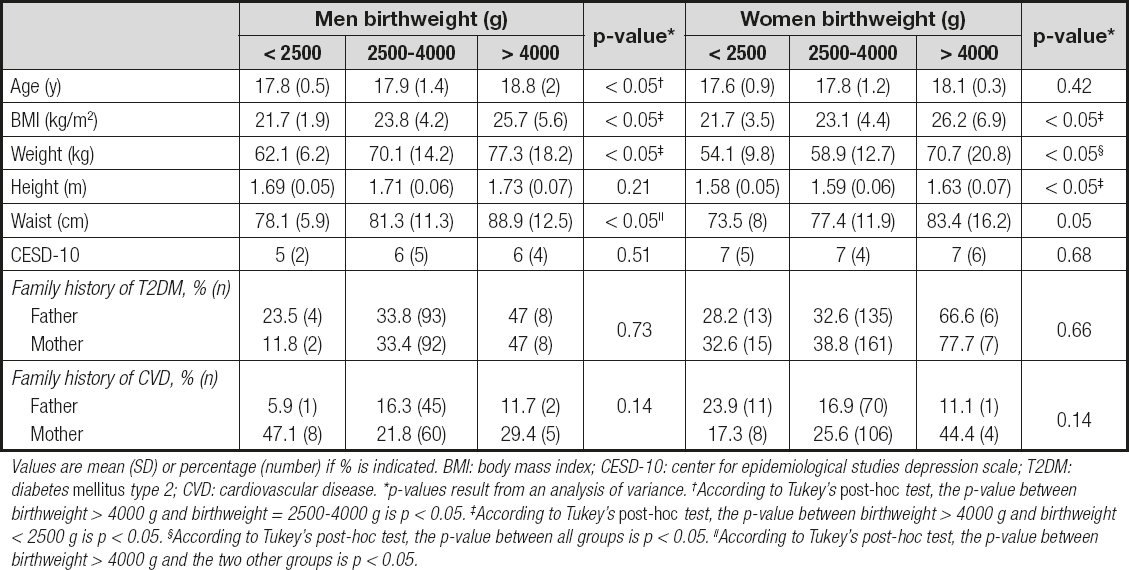
Values are mean (SD) or percentage (number) if % is indicated. BMI: body mass index; CESD-10: center for epidemiological studies depression scale; T2DM: diabetes mellitus type 2; CVD: cardiovascular disease. *p-values result from an analysis of variance. †According to Tukey's post-hoc test, the p-value between birthweight > 4000 g and birthweight = 2500-4000 g is p < 0.05. ‡According to Tukey's post-hoc test, the p-value between birthweight > 4000 g and birthweight < 2500 g is p < 0.05. ¦According to Tukey's post-hoc test, the p-value between all groups is p < 0.05. ||According to Tukey's post-hoc test, the p-value between birthweight > 4000 g and the two other groups is p < 0.05.
Means and SDs for BP, lipid profile, and serum glucose levels according to birthweight categories are shown in table II. There was a significant association between SBP and DBP, but only DBP had statistical significance across birthweight categories. Participants with birthweight > 4000 g, had higher means for DBP (p < 0.05).
Table II. Blood pressure, lipid profile, and serum glucose level (mean [SD]) according to birthweight categories

SBP: systolic blood pressure; DBP: diastolic blood pressure; TC: total cholesterol; TG: triglycerides; HDL-C: high density lipoprotein-cholesterol; LDL-C: low-density lipoprotein-cholesterol; VLDL-C: very low density lipoprotein-cholesterol; FBG: fasting blood glucose. *p-values result from the analysis of variance. †Statistical significance according to p-value but no difference between groups in Tukey's post-hoc test. ‡According to Tukey's post-hoc test, the p-value between birthweight > 4000 g and the two other groups is p < 0.05.
DISCUSSION
The gestational stage and early childhood represent a window of phenotypic plasticity, and represent a sensitive period as related to cardiometabolic risk programming. Maternal weight status, lipid profile, smoking habit, gestational diabetes mellitus, or hypertensive disease during pregnancy condition birthweight and gestational age (26-29).
All these prenatal factors, along with postnatal factors like breastfeeding and rapid weight gain during childhood, are associated with cardiometabolic risk later in life (29-33). Genetic factors and epigenetic mechanisms play an important role in programming the genes correlated to cardiovascular and mental disease (34,35).
There are very few studies in developing countries that review the association between birthweight, components of MetS, and mental illness. We decided to investigate the possible association between these three variables in young Mexican adults. Our results are quite similar to those of previous studies (3). In the present study only HBW had an association with overweight and obesity. The reviewed studies demonstrated a J- or U-shaped relationship between these two variables (6,7). We also observed, in men only, a significant association between birthweight and central obesity (p < 0.05), which was only marginally identified among women (p = 0.05).
We found that SBP had statistical significance but was inconclusive at the post-hoc test. Only HBW was associated with high DPB. The results from studies examining the associations between HBW and hypertension are inconsistent. Several studies showed an inverse relationship between birthweight and BP (8,9). Nevertheless, a recent study in adolescents showed a positive association between HBW and hypertension (36).
There are studies that support the statement that cardiovascular risk factors are related to the transmission of mitochondrial DNA (6,37). Our study did not find a significant p-value for a family history of diabetes or cardiovascular disease in the maternal branch, but it could have been otherwise with more cases.
Other CVD risk factors and components of MetS, including low HDL-C, and high levels of LDL-C, TC, TG, SBP and FBG, had no significant association with birthweight categories. Also, in this study we observed no association between birthweight categories and CESD-10 score (17).
We mentioned above that Dos Santos et al. found that birthweight was not a risk factor for the development of MetS during adolescence (13). This result was probably conditioned by the small size of their Brazilian cohort (n = 172), a possible bias in the selection of participants, or methodological differences in the evaluation of adiposity. Nevertheless, a study with a Mendelian randomization analysis studied 7 single nucleotide polymorphisms (SNPs) independently contributing to birthweight at genome-wide significance to estimate the effect of birthweight on risk of coronary ischemic disease, and they concluded that there was no strong evidence between birthweight, coronary disease, and lipid profile (38).
Despite this inconsistency among studies, there is a need to develop public health policies that adopt preventive measures to promote adequate maternal-fetal and child development, and enable an early diagnosis of metabolic abnormalities (28), as well as Improvements in the policies related to healthy eating, demanding proper food labeling, promotion of exclusive breastfeeding for at least 6 months, and community-based primary prevention programs regarding lifestyle, among other measures (29,39). A study reveals iron supplementation in children with LBW as a measure to reduce systolic blood pressure on childhood (40). That is a novel observation suggesting that CVD risk factors like hypertension might be reduced with early interventions.
A low number of cases is the main limitation of this study. We only had 778 patients who fulfilled the selection criteria, 689 cases of NBW, 63 cases (8 %) of LBW, and 26 cases (3.3 %) of HBW, which corresponds to the percentages of LBW and HBW in the Mexican literature. The observed results have to be carefully analyzed. Other prenatal confounders like maternal obesity, smoking habit, and gestational diabetes mellitus, and postnatal confounders like breastfeeding duration, socioeconomic status, complementary feeding, catch-up growth, diet and physical activity, were not available and were not considered in the analysis. Due to the cross-sectional design we were unable to determine causality.
In conclusion, the findings of this population-based study revealed a positive relationship between birthweight categories and some CVD risk. Young adults that were born with HBW had association with high DPB, weight, and BMI. Depression was not related to birthweight categories.
CONCLUSIONS
The findings of this population-based study (young Mexican adults) revealed that depression was not related to birthweight. However, a positive relation between birthweight categories and some CVD risk factors such as DBP, weight, and BMI was shown in both genders. Furthermore, WC and height had a relationship with birthweight in men and women, respectively.














