INTRODUCTION
Primary hypertension is a kind of cardiovascular syndrome caused by many complicated factors, and can potentially damage many target organs. It is one of the common diseases that afflict the elderly. Due to a long disease course and easy recurrence, there is no radical treatment for this disease currently. The patients need to take a lifelong course of drugs to control their symptoms, which easily leads to frailty symptoms in patients (1). The frail status of the elderly can easily result in decline of the function of many physiological systems, such as the nervous, metabolic, and immune systems, causing motor and cognitive impairment in patients, seriously affecting their independent living ability, increasing the pressure on medical resources and social investment, bringing serious economic burden to patient families, and exposing social pensions and the medical and health security system to more severe challenges (2). Frailty is preventable, and an accurate, effective assessment and identification of frail patients, ans well as timely intervention measures, can slow down or even reverse the process of frailty (3). Muscles are one of the earliest target organs showing frail symptoms. Harada et al. reported that muscle function directly affected the postoperative recovery of patients with acute coronary syndrome and relieved the frail status of their motor organs (4). Nichols et al. found that the frail status and muscle function of patients were closely related to the probability of adverse events in patients with such cardiovascular diseases as chronic cardiac failure and coronary heart disease (5). However, there are few reports on the correlation between patients› frail status and lower extremity function in elderly hospitalized patients with hypertension. In view of the lower extremity function of patients, the correlation between frail status and lower extremity function of elderly hospitalized patients with hypertension was studied herein, aiming to provide a new perspective for preventing frail diseases in the elderly and for clinical nursing.
MATERIALS AND METHODS
SUBJECTS
A total of 336 elderly patients with primary hypertension who were hospitalized for the first time in our hospital and were discharged from October 2012 to October 2014 were enrolled. Their average age was 77.85 ± 6.46 years. All patients or their family members were informed of the purpose of this study, volunteered to participate in this study, and signed the informed consent form. This study met the ethical requirements of the hospital and was reviewed and approved by the Ethics Committee.
Inclusion criteria (6): 1) patients meeting the diagnostic criteria of the 2010 Chinese guidelines for the management of hypertension, or those with systolic blood pressure/diastolic blood pressure < 140/90 mmHg, or those previously diagnosed with hypertension; 2) those with an age ≥ 65 years; 3) those who had no expression disorder and could communicate clearly and independently; 4) those who actively cooperated according to the needs of this study.
Exclusion criteria: 1) patients at the end stage or the acute development stage of the disease; 2) those with secondary hypertension caused by pheochromocytoma, kidney disease, primary aldosteronism or refractory hypertension; 3) those who had any consciousness disorder and were unable to communicate normally; 4) those who were severely disabled and unable to cooperate; 5) those with a length of hospital stay < 2 days or > 30 days; 6) those who underwent valvular replacement, coronary artery bypass grafting, or pacemaker implantation, or had a history of lower limb surgery in the past year.
METHODS
On the one hand, the medical records of the elderly inpatients were checked, and the basic information of such patients, including age, gender, nutritional status, blood pressure, body mass index (BMI), lifestyle, and sleepiness status was collected. On the other hand, unified assessment forms were formulated, and standardized and uniform training was conducted for the assessing physicians. The degree of frailty and lower extremity function of the enrolled patients were assessed, recorded, and statistically analyzed.
Frailty was assessed according to the Frail scale proposed by the International Association of Nutrition and Aging in 2008, mainly through questions on the following 5 aspects (7) — 1) Fatigue: In the past month, did you feel tired? 2) Resistance: Can you walk upstairs alone? 3) Aerobic exercise: Do you have any difficulty walking for 5 minutes or 500 meters continuously? 4) Illness: Are you suffering from five or more chronic diseases? 5) Loss of weight: In the past 6 months, have you lost more than 5 % of your body weight? Each item was scored with 1 or 0 points, and the patients› frail status was evaluated according to the total score. A total score of 0 points indicated non-frailty, a total score of 1-2 points indicated pre-frailty, and a total score ≥ 3 points suggested frailty. According to frail status, the patients were divided into a frail group, pre-frail group, and non-frail group.
The patients' lower extremity function was assessed with the Short Physical Performance Battery (SPPB) (8), which included the chair sit-to-stand test, three-posture balance test, and 6-meter gait speed test. 1) Chair sit-to-stand test: 4 points were for ≤ 11.19 s, 3 points were for 11.20-13.69 s, 2 points were for 13.70-16.69 s, 1 point was for > 16.69 s, and 0 points was for > 60 s or failing to complete the test. 2) Three-posture balance test: in the feet-side-by-side test, 1 point was for > 10 s, and 0 point was for ≤ 10 s. In the semi-tandem test (side of the heel of one foot touching the big toe of the other), 1 point was for > 10 s, and 0 point was for ≤ 10 s. In the full tandem test (heel of one foot in front of and touching the toes of the other foot), 2 points were for > 10 s, 1 point was for 3-10 s, and 0 points was for < 3 s. 3) Six-meter gait speed test: 4 points were for < 4.81 s, 3 points were for 4.82-6.20 s, 2 points were for 6.20-8.70 s, 1 point was for > 8.70 s, and 0 points was for failing to complete the test. The total score of SPPB was 12 points; 0-6 points indicated a poor lower extremity function, 7-9 points suggested a mildly poor lower extremity function, and 10- 12 points suggested a good lower extremity function.
The patients' nutritional status was evaluated with the Mini Nutritional Assessment (MNA) tool (9), which involved 1) basic parameters such as height, weight, calf circumference, upper arm circumference, and weight loss during the last 3 months; 2) a comprehensive assessment mainly consisting of pain, mental and psychological activities, etc.; 3) a dietary assessment mainly on appetite, self-feeding, meal times, and protein and vegetable intake, and 4) a subjective assessment, which was the patient's self-assessment of their own health and nutritional status. The total score of MNA was 30 points; < 17 points indicated malnutrition, 23.5 to 17 points indicated risk of malnutrition, and ≥ 24 points suggested a normal nutritional status.
The degree of sleepiness was assessed using the Epworth Sleepiness Scale (ESS) (10). The frequency of sleepiness (0 point for never sleepy, 1 point for occasionally sleepy, 2 points for sometimes sleepy, and 3 points for frequently sleepy) was rated while the patients were engaged in the below activities: 1) watching TV; 2) sitting and reading: 3) riding as a passenger in a car for an hour; 4) sitting at a public place; 5) sitting in a car, stopped for a few minutes in traffic; 6) lying down to rest in the afternoon when circumstances permitted; 7) sitting quietly after a lunch without alcohol; and 8) talking with someone. An ESS score ≥ 6 indicated sleepiness.
STATISTICAL ANALYSIS
The SPSS 22.0 software was utilized for the statistical analysis. The numerical data were represented as [n (%)] and examined using the χ2 test. The quantitative data were expressed as mean ± standard deviation (x ± s), and the independent t-test was employed for comparisons between two groups. Spearman's correlation analysis was used for correlation between frailty score and lower extremity function score. A receiver operating characteristic (ROC) curve was plotted to analyze the values of such factors as lower extremity function in predicting the frailty of patients. A p < 0.05 suggested that a difference was statistically significant.
RESULTS
BASELINE CLINICAL DATA
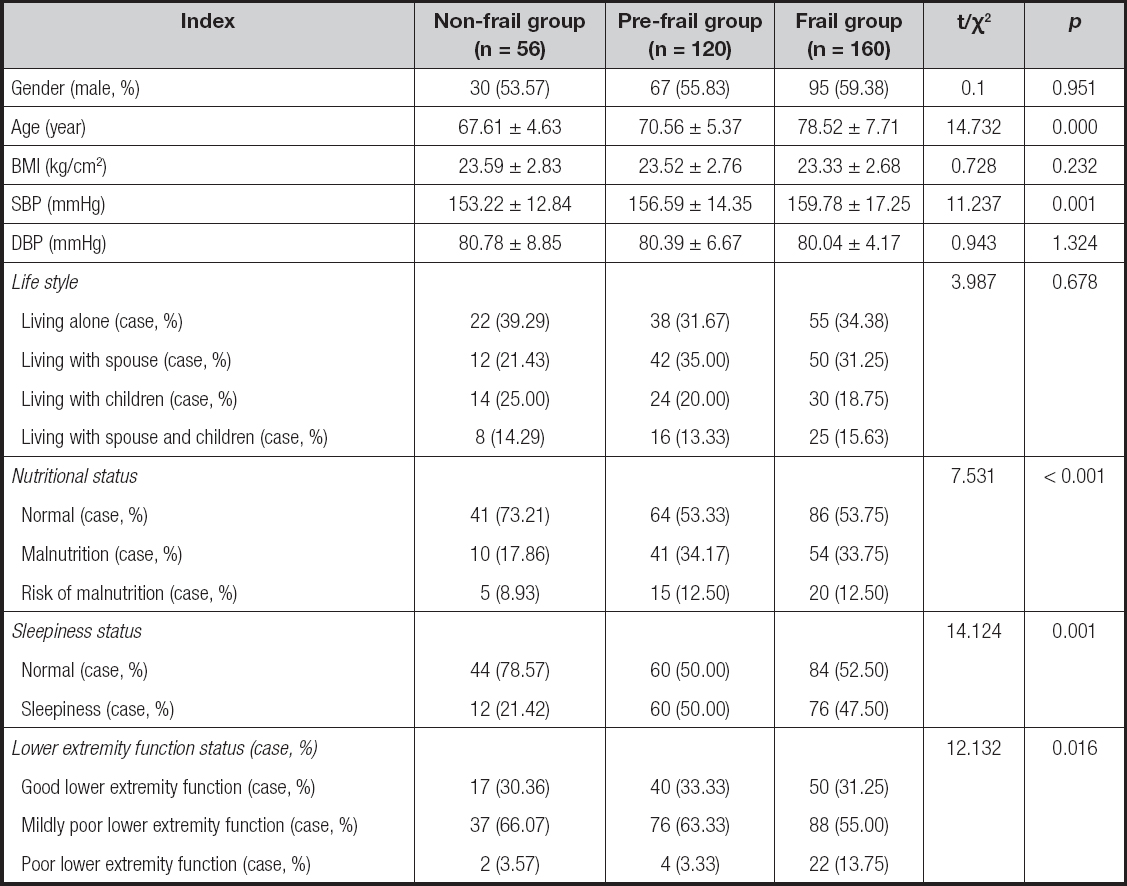
After the basic information of all 336 patients enrolled was statistically analyzed, 56 (16.67 %) patients were assigned to the non-frail group, 120 (31.71 %) were in the pre-frail group, and 160 (47.62 %) were in the frail group. There were statistically significant differences in age, SBP, nutritional status, sleepiness status, and lower extremity function between the three groups (p < 0.05), while no statistically significant difference was observed in gender, BMI, DBP, or lifestyle among them (p > 0.05). Compared with those in the non-frail group, age and SBP were higher, the proportion of malnutrition and sleepiness status increased significantly, and lower extremity function was significantly poorer in both the frail group and the pre-frail group (p < 0.05) (Table I).
COX MULTIVARIATE REGRESSION ANALYSIS
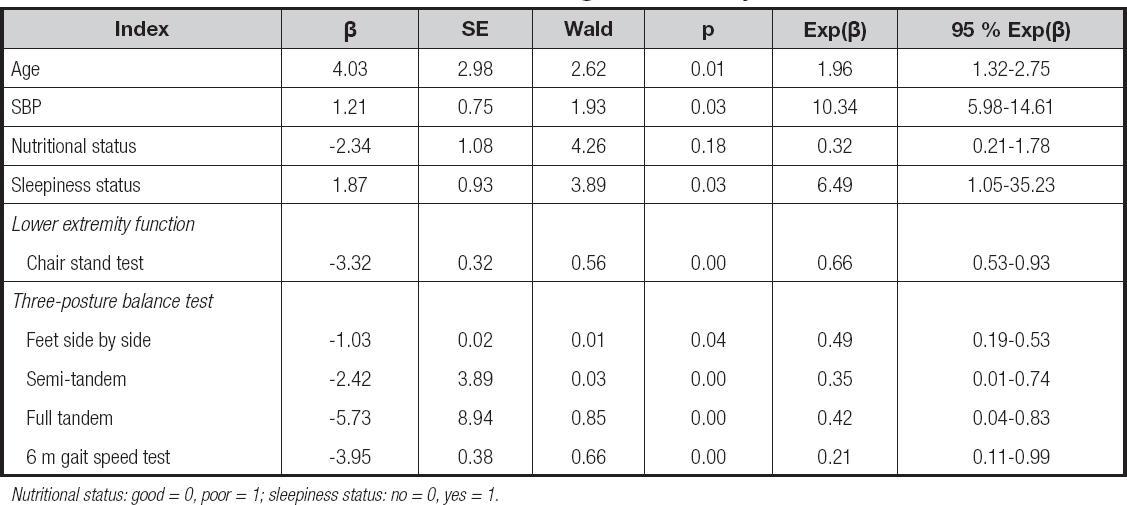
Age, SBP, nutritional status, sleepiness status, and lower extremity function parameters were incorporated into the COX regression equation for analysis. The results showed that age, SBP, and sleepiness status were independent risk factors of frailty in elderly hospitalized patients with hypertension (p < 0.05), and lower extremity function parameters were independent protective factors against frailty in them (p < 0.05) (Table II).
LOWER EXTREMITY FUNCTION
Compared with that in the non-frail group, the lower extremity function score was significantly lower in the frail group, and the difference was statistically significant (p < 0.05) (Table III), indicating that patients with low scores in lower extremity function parameters are more prone to frailty.
CORRELATION BETWEEN FRAIL STATUS AND LOWER EXTREMITY FUNCTION
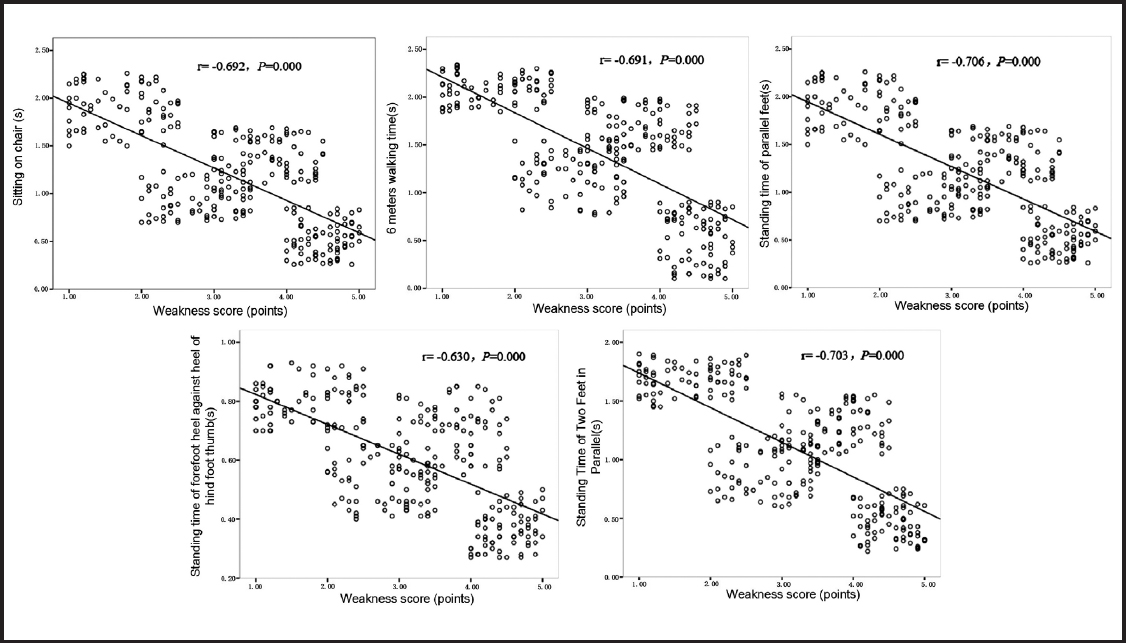
It was found through Spearman's correlation analysis that there were negative correlations between the patients' frail status and lower extremity function parameters (p < 0.05) (Fig. 1).
PREDICTIVE VALUE OF LOWER EXTREMITY FUNCTION FOR FRAIL STATUS IN ELDERLY HOSPITALIZED PATIENTS WITH HYPERTENSION
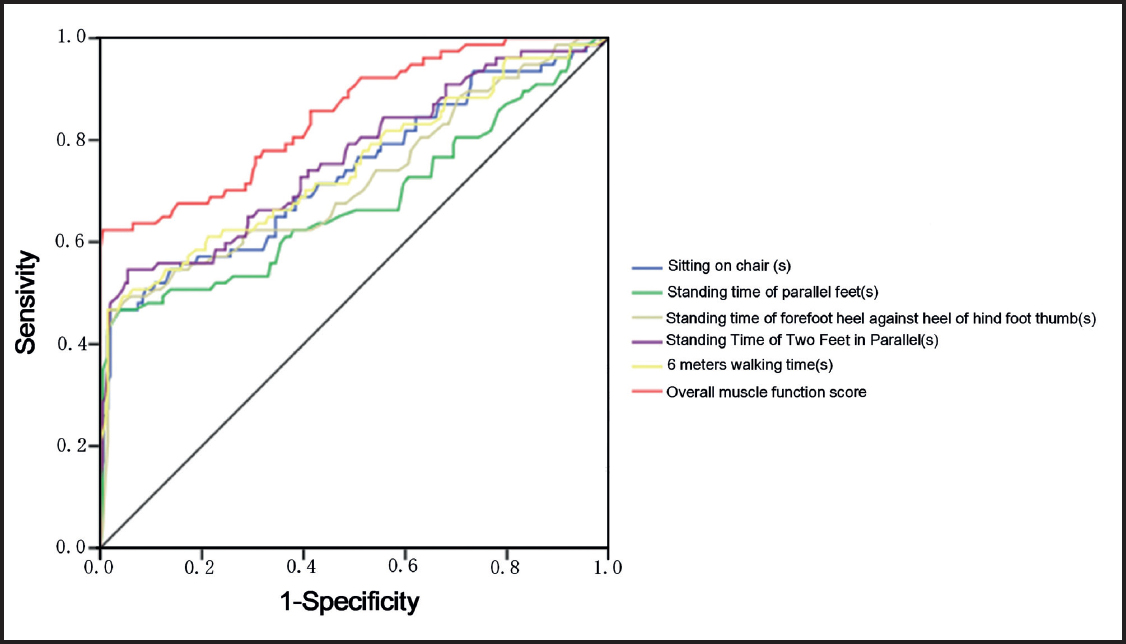
The results of the ROC curve analysis revealed that the lower extremity function of elderly hospitalized patients with hypertension had a higher value for predicting their frail status (Fig. 2 and Table IV).
DISCUSSION
With increasing population aging, frailty has become one of the research hotspots in geriatrics and nursing. The occurrence of frailty is closely related to the prognosis of cardiovascular diseases such as coronary heart disease and heart failure in elderly patients (11). The frail status of elderly hospitalized patients with hypertension is a high-risk factor for predicting fracture, fall, hospitalization, disability and death (12). Taking effective action measures can delay or reverse the development of frailty in patients (13). Hence, timely prediction of the frail status of elderly hospitalized patients with hypertension, and early intervention are of great significance for the clinical treatment and prognosis of the disease.
Frailty is an aging syndrome caused by degenerative changes or chronic diseases in which the physiological reserve of the elderly is reduced or the function of multiple systems and organs is abnormal. The mechanism of frailty in the elderly is rather complicated, which is a result of the joint effects of various factors such as body function and daily habits (14). According to the study of Jindal et al. (15), age, social support, and lifestyle of the elderly directly affected their mental state. The Frail scale is currently one of the internationally recognized criteria for assessing frailty in the elderly (16). In this study, after the basic information of patients was compared, they were divided into three groups according to their degree of frailty. Among the 336 patients selected, 56 (16.67 %) were in the non-frail group, 120 (31.71 %) were in the pre-frail group, and 160 (47.62 %) were in the frail group, indicating that there was a high proportion of elderly hospitalized patients with hypertension in this study. It was found through further investigation that compared with those in the non-frail group, age and SBP increased significantly, the proportion of malnutrition and sleepiness rose significantly, and lower extremity function declined significantly in both the frail group and the pre-frail group (p < 0.05). Besides, the patients had similar gender, BMI, DBP, and lifestyle (p > 0.05), suggesting that the difference in lower extremity function was statistically significant.
The human body performs various motions through the movement of joints and bones driven by the contraction and relaxation of 639 muscles. The muscle function of human bodies begins to decline from the age of 40, and it decreases gradually as age advances (17). Declined muscle function is prevalent in the elderly, and it is closely related to adverse events of cardiovascular disease (18). SPPB, a widely recognized scale for assessing lower extremity function in the elderly, can be used to evaluate their ability to perform daily activities (19). Herein, the results of the SPPB suggested that the lower extremity function of the enrolled elderly inpatients with hypertension was at a lower-middle level. It was found through Spearman's correlation analysis that the frailty score was negatively correlated with the lower extremity function score, that is, the lower the lower extremity function score, the higher the degree of frailty. The results suggested that the frail process of elderly patients can be delayed through intervention consisting of muscle function training (20).
There were still some limitations in this study. It was an observational study, the research subjects were too old, the number of cases was small, the observation period was short, and the patients were not followed up after discharge. However, this study paves the way for further in-depth research.
To sum up, lower extremity function is negatively correlated with the frail status of elderly inpatients with hypertension, which is a protective factor against frailty in them, and can be used to predict their frail status. In the future, it is necessary to further study the mechanism of lower extremity function on the frail status of elderly inpatients with hypertension.