Introduction
Cardiovascular diseases, mainly manifesting as heart failure, are the most common critical illness in the emergency department. Heart failure is the severe and terminal stage in the development of various cardiovascular diseases. It is the main cause of hospitalization and disability in the elderly, and the cause of one in nine deaths in the United States (1). Malnutrition is a common complication that affects the prognosis of elderly hospitalized patients. At present, there are few studies on the nutritional risk and nutritional support of patients with severe cardiac diseases. This study aimed to study the nutritional status and clinical nutritional support of patients with severe cardiac disease through the NRS2002 nutritional risk screening tool, to understand the relationship between nutrition-related factors of severe cardiac patients and the severity of cardiac function and prognosis.
METHODS
STUDY POPULATION
From January 2017 to December 2019 there were 209 patients with severe cardiovascular disease hospitalized in the emergency intensive care unit (EICU) of Qilu Hospital. According to the New York Heart Association (NYHA) Cardiac Function Classification and Killip Cardiac Function Classification, these patients were classified into 2 groups. In our study, we divided the 209 cases into the non-heart failure group (47 cases) and the heart failure group (162 cases). Among the 47 cases in the non-heart failure group, there were 9 cases categorized as NYHA grade I and 38 cases as Killip grade I. According to the Cardiac Function Classification, 10 cases of grade II, 25 cases of grade III, 41 cases of grade IV, a total of 76 cases were classified into the heart failure group. According to Killip's classification, 36 cases of grade II, 14 cases of grade III, 36 cases of grade IV, and a total of 86 cases were classified into the heart failure group. All patients with related treatments had signed an informed consent form.
RESEARCH METHODS
Sample size calculation
This study was a cross-sectional study, which used the formula n = K × Q / P. The allowable error of the research project was 15 %, so constant K = 178. n represents the number of people surveyed, P represents the probability of nutritional risk, 51 % (2). Q = 1 - P, so it could be calculated that n = K × Q / P = 178 × 49 % / 51 % = 171 cases. Considering a 20 % loss to follow-up rate (data insufficiency, etc.), there were 205 cases. A total of 209 cases were finally included in the sample size.
NRS2002 score
The initial evaluation of the NRS2002 scoring scale was completed in the inpatient system by doctors and nurses who had undergone intense professional training. On admission to hospital, to measure and calculate body mass index we used BMI = body mass (kg) / height2 (m2). (After admission, body mass and height were also measured: BMI = body mass [kg] / height2 [m2].) Patients with fluid retention are given adequate diuresis and have dry body mass measured to calculate the BMI index. For patients with obvious edema, ascites, pleural effusion, or unable to stand up, serum ALB < 30 g/L is > 3 points. Assessment was completed after the APACHE II score test data of the inpatient system was issued within 24 hours. Malnutrition was defined as hospitalized cardiac patients with BMI < 18.5, while BMI ≥ 24 was overweight, and BMI ≥ 28 was obesity. NRS2002 scoring standard: 0-2, no nutritional risk; ≥ 3 points, low nutritional risk; ≥ 5 points, high nutritional risk; among them, those with ≥ 3 points or more were defined as having malnutrition risk.
Specimen collection
After admission, all patients underwent radial artery blood sampling, using a bedside blood gas analyzer to detect blood glucose (BS), lactic acid (LAC), blood potassium (K+), blood calcium (Ca++), blood sodium (Na+) and other indicators. In the immediate resting state, venous blood was collected in the supine position, and the bedside immunofluorescence method was used to detect troponin I (CTNI), myoglobin (MYO), creatine phosphokinase and its isoenzymes (CK-MB), and N-terminal forebrain natriuretic peptide (NT-proBNP). All subjects were in a resting state in the early morning of the next day, and venous blood was collected from the supine position to determine hemoglobin (Hb), albumin (ABL), prealbumin (PA), triacylglycerol (TG), and cholesterol (TC), etc. The target dose of nutritional support was 20-30 kcal/(kg · d).
STATISTICAL ANALYSIS
The SPSS 25.0 statistical software was used for the analysis. Measurement data conforming to a normal distribution were represented as ± s. Data not conforming to a normal distribution was represented as M (P25, P75), and transformed into a normal distribution with the natural logarithm (Ln). Pairwise comparisons between groups used Student's t-test. One-way analysis of variance was used for comparison between multiple groups, and the SNK-q test was used for multiple comparisons between groups when the difference was statistically significant. The count data are expressed as number of cases or rate, and comparison between groups was performed through the chi-squared test. A p < 0.05 indicated that the difference was statistically significant.
RESULTS
The age of patients ranged from 14 to 90 years old, with an average age of 69.23 ± 13.42 years. There were 123 males (58.85 %) with an average age of 66.98 ± 13.51 years, and 86 females (41.15 %) with an average age of 72.45 ± 12.69 years in our study.
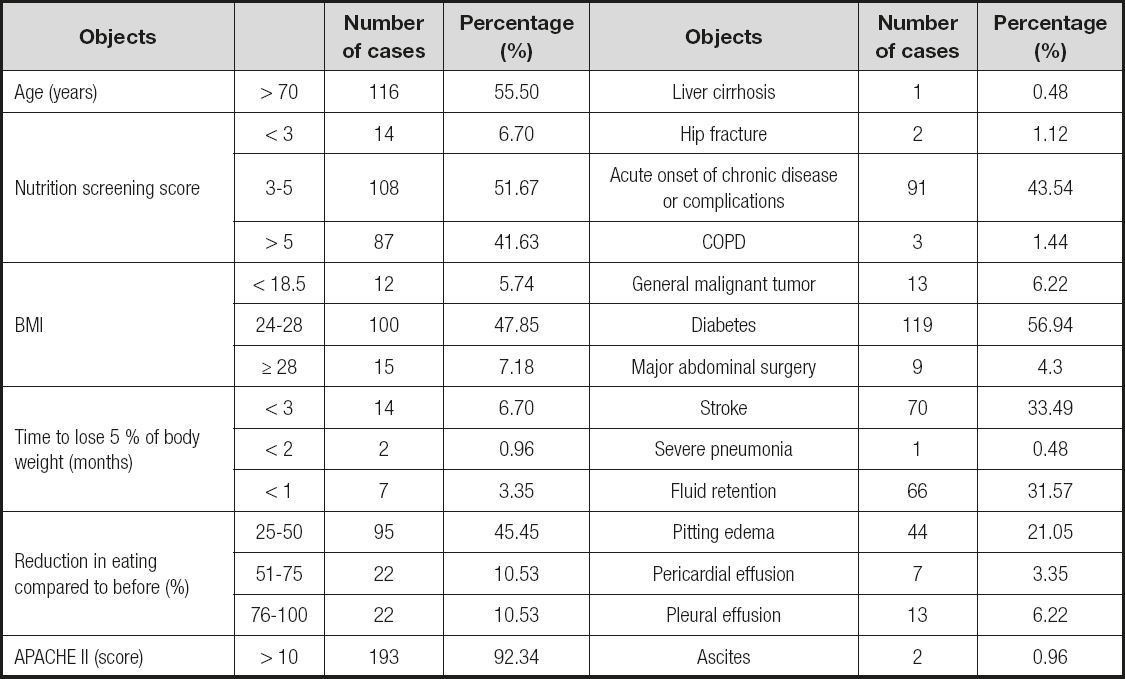
The results of the NRS2002 nutritional risk screening are shown in table I. The degree of aging of patients with severe cardiac diseases was high, of which 144 cases (68.90 %) were ≥ 65 years old, and 116 cases (55.50 %) were over 70 years old. There were 14 cases (6.70 %) that were not at nutritional risk, 195 cases (92.34 %) were at nutritional risk, and 87 cases (18.18 %) were at high nutritional risk— among them, 83 patients (97.65 %) with NYHA classification had nutritional risk, as was also the case with 112 patients (90.32 %) with Killip classification. Among them, 12 cases (5.74 %) were malnourished. In addition to malnutrition, overweight accounted for 47.85 %, and obese accounted for 7.18 % of the sample. There were 139 cases (66.51 %) with abnormal food intake at the time of admission, of which 117 cases (55.98 %) had a weight decrease of 25 % to 75 %, and 22 cases (10.53 %) had a weight decrease of 76 % to 100 %. Twenty-three patients (11.00 %) had had a weight loss of 5 % in the past 3 months. There were 66 cases (31.57 %) with fluid retention. There were 193 cases (92.34 %) with APACHE II score > 10 points.
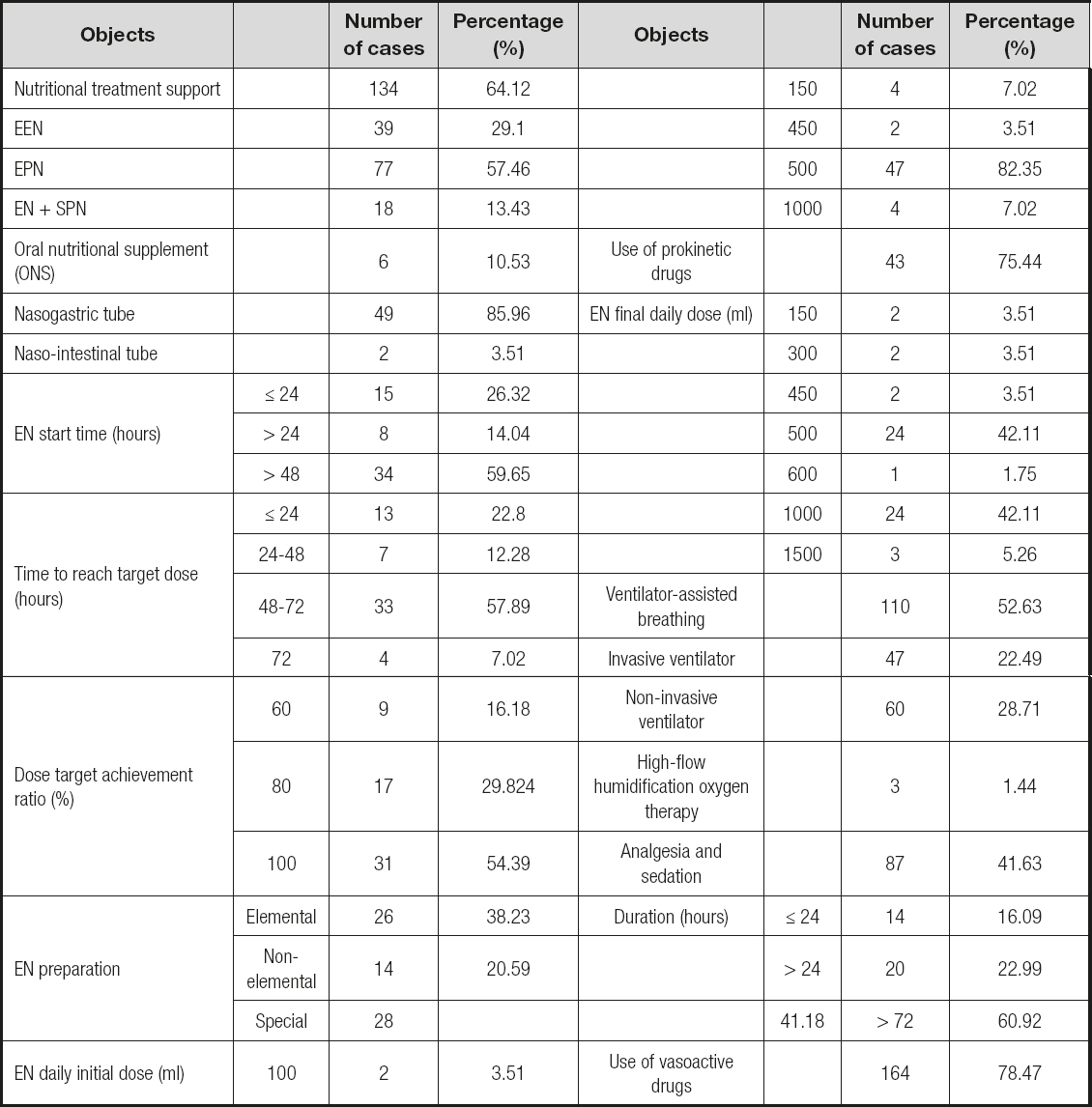
The information on the nutritional support is shown in table II. There were 134 cases (64.12 %) of critically ill patients receiving nutritional support, EN 39 cases (29.10 %), EPN 77 cases (57.46 %), EN + SPN 18 cases (13.43 %); 23 cases (40.35 %) had EN start time in 48 h, 34 cases (59.65 %) were over 48 h; 31 cases (54.39 %) met the 100 % target. Among the enteral nutritional preparations, 42 cases (61.76 %) were non-elemental and special preparations. The initial dose was ≤ 500 ml (93.22 %), the final dose was 500 ml in 24 cases (41.38 %), and 1000 ml in 24 cases (41.38 %), of which 43 (EN and EN + SPN) (75.44 %) used prokinetic drugs. In this group of patients, 110 cases (52,63 %) used ventilator-assisted ventilation, 87 cases (41.63 %) used analgesia and sedation, and 164 cases (78.47 %) used vasoactive drugs.
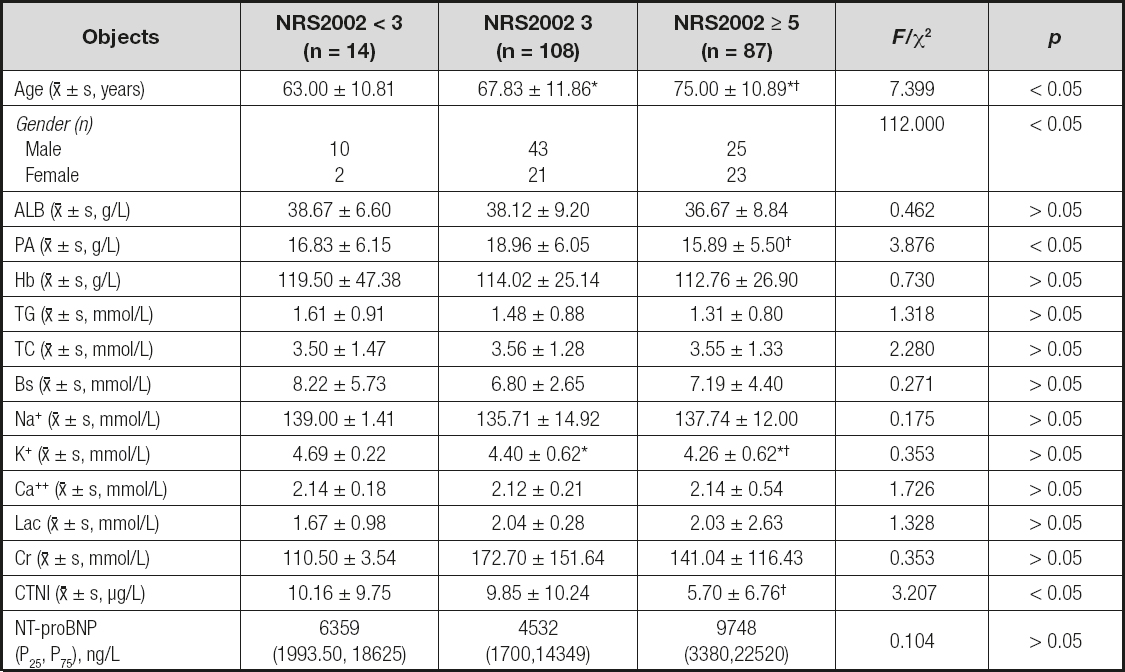
A comparison of the basic data of different patients with NRS2002 score is shown in table III. According to the table, we found that the nutritional risk of patients with severe cardiac disease increased significantly with age. The Cr and NT-proBNP values of NRS2002 low-nutrition and high-risk patients were higher than those of non-risk patients; the lower the TC value, the higher the nutritional risk, and the difference between low-risk patients and non-risk patients was statistically significant. In addition to the above indicators, there was no statistically significant difference in other related nutritional indicators among different nutritional risk groups.
Table III. Comparison of basic data of patients with different scores in NRS2002
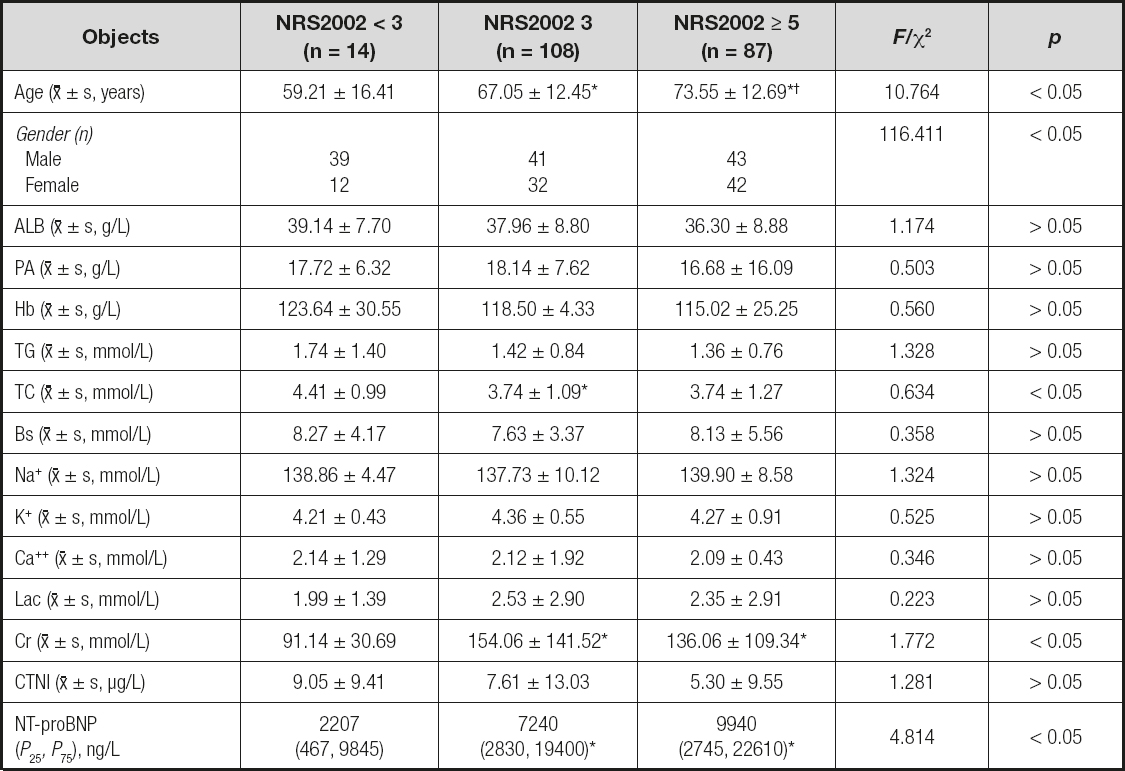
Compared with NRS2002 without risk, *p < 0.05; compared with NRS2002 of low-risk group, †p < 0.05.
A comparison of the basic data of patients with different scores in the Killip classification in NRS2002 is shown in tables IV and V. Killip-graded cardiac patients with severe cardiac function had a worsened nutritional risk, and the differences between groups, including the non-heart failure and the heart failure groups, were statistically significant. The PA value of the nutritional high-risk group was significantly lower than in the other groups. The CTNI value was negatively correlated with nutritional risk, and the comparison between the high-risk group and low-risk group was statistically significant. The higher the NT-proBNP value, the higher the nutritional risk of patients, and the comparison between the three groups was not statistically significant.
Table IV. Comparison of basic data of patients with different scores in Killip grading of NRS2002
Compared with NRS2002 without risk, *p < 0.05; compared with NRS2002 low risk, †p < 0.05.
Table V. Comparison of NRS2002 scores in patients with Killip classification of cardiac function
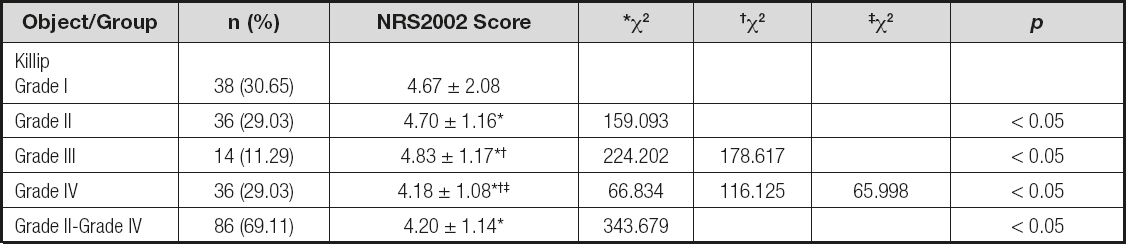
Compared with grade I, *p < 0.05; compared with grade II, †p < 0.05; compared with grade III, ‡p < 0.05.
A comparison of basic data of the NYHA-graded patients with different scores in NRS2002 is shown in tables VI and VII. The nutritional risk of patients with severe cardiac diseases in the NYHA classification increases with age, and the worse the heart function, the higher the nutritional risk. The nutritional risk of the non-heart failure group was lower than that of the heart failure group, and the differences between the different nutritional risk groups were statistically significant. Besides, we also found that the higher the CTNI value and NT-proBNP value, the higher the nutritional risk of patients, and the comparison between the three groups was not statistically significant.
Table VI. Comparison of basic data of NRS2002 patients with different NYHA grades
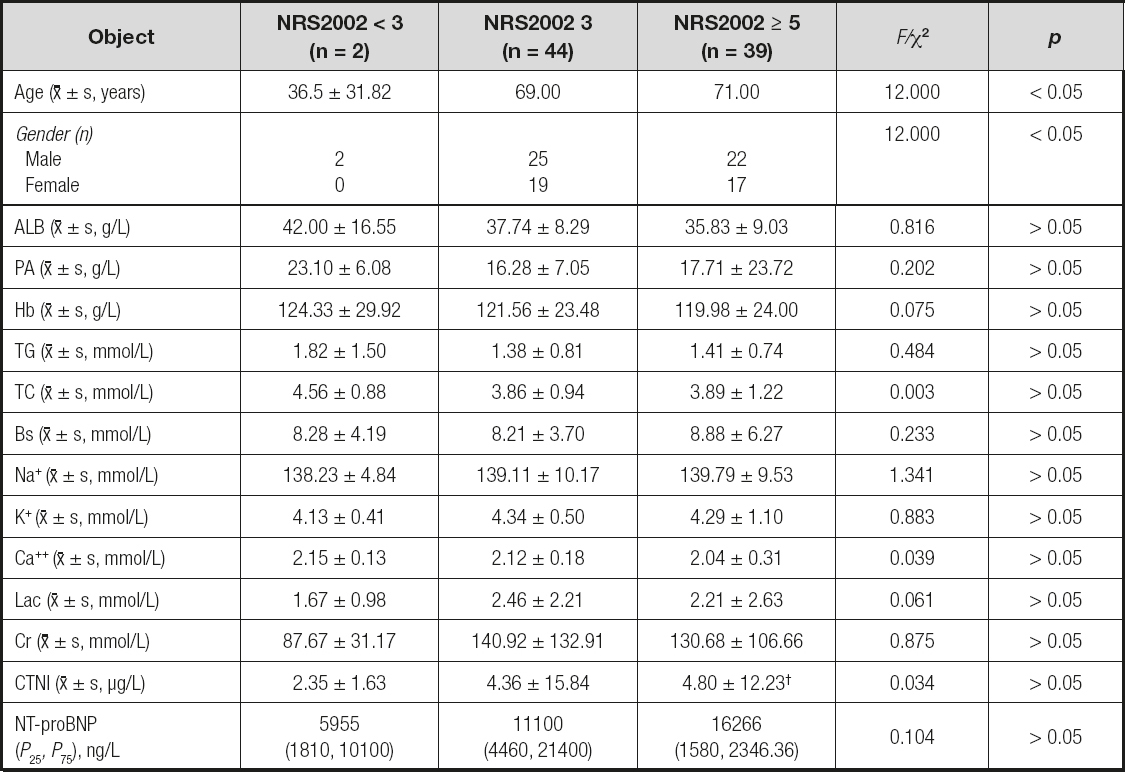
Compared with NRS2002 without risk, *p < 0.05; compared with NRS2002 low risk, †p < 0.05.
Table VII. Comparison of NRS2002 scores of patients with NYHA classification of cardiac function
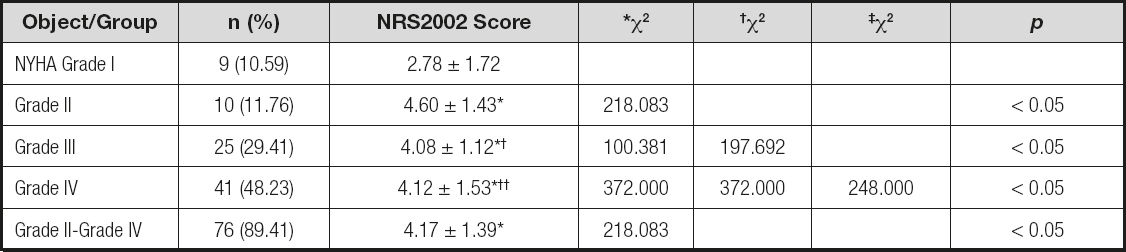
Compared with NRS2002 without risk, *p < 0.05; compared with NRS2002 low risk, †p < 0.05.
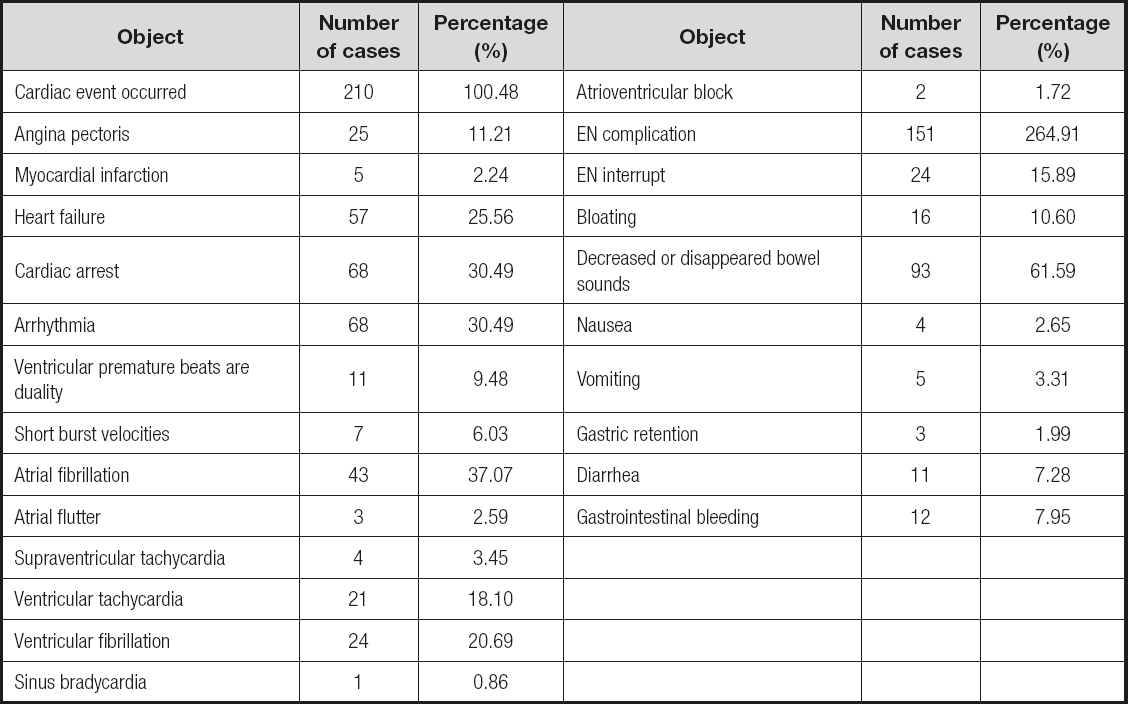
The comparison of hospital outcome indicators for severe cardiac patients is shown in table VIII and table IX. There were 223 cases (155.33 %) of major adverse cardiac events during the hospitalization of severe cardiac patients, and 193 cases (86.55 %) of cardiac arrest, arrhythmia, and heart failure were the main ones. Among arrhythmias, 43 cases of atrial fibrillation (37.07 %), 24 cases of ventricular fibrillation (20.69 %), and 21 cases of ventricular tachycardia (18.10 %) stood out. What is more, there were 151 cases (72.25 %) of gastrointestinal complications, and 133 cases (40.62 %) were mainly caused by weakened or disappeared bowel sounds, abdominal distension, and interruption of EN. The incidence of major adverse cardiac events in EN patients was 37 cases (64.91 %), and the incidence of enteral nutrition complications was 31 cases (54.39 %). The higher the nutritional risk, the higher the incidence, and the difference between risk groups was statistically significant. The in-hospital mortality rate of patients with severe cardiac disease was 28.23 %. The higher the nutritional risk, the higher the mortality rate, and the difference between risk groups was statistically significant. The higher the nutritional risk of patients with severe cardiac diseases, the longer the average length of hospital stay, but the difference between the groups was not statistically significant.
Table IX. Comparison of outcome indexes of inpatients with severe heart disease
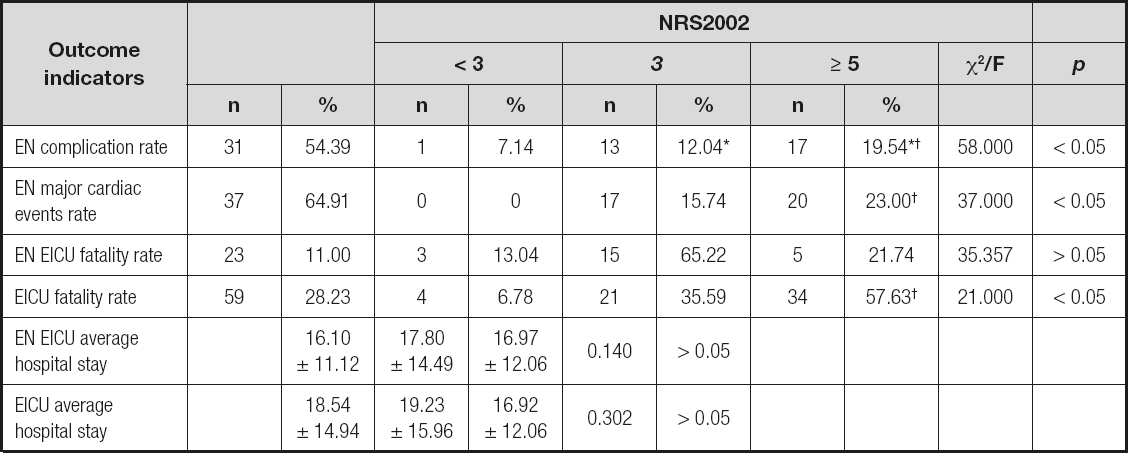
Compared with NRS2002 low risk (< 3), *p < 0.05; compared with NRS2002 medium risk (3), †p < 0.05.
DISCUSSION
The incidence of nutritional and metabolic disorders in critically ill patients with heart failure is high. Chronic heart failure, gastrointestinal dysfunction, insufficient nutrient intake and increased consumption can easily lead to malnutrition risks. Malnutrition is a common complication in patients with heart failure and an independent predictive risk factor for death. Obesity is an important risk factor for heart failure (3).
Adequate nutrition, which has an established role in the prevention of heart failure, is known to promote health-related quality of life by addressing malnutrition and promoting optimal functioning among older adults (4). NRS-2002 is a reliable screening tool in an in-patient sample with chronic heart failure (5). In our study, 68.90 % of patients in this group are ≥ 65 years old, with an average age of 69.23 ± 13.42 years. The overall nutritional status of patients with severe cardiac disease is manifested as nutritional disorders. The ratio of nutritional risk is 92.34 %, which is significantly higher than the 37.6 %-51.41 % reported by Zhu MW. The incidence of malnutrition of 5.26 % is lower than that of 10 %-20 % reported in other studies (2-6), which may be related to a 52.80 % of patients with first-onset acute heart failure admitted to the emergency department. Among them, there were 3 cases (25 %) with Killip classification grade I (25 %), 9 cases (75 %) with Killip classification and NYHA classification grades III and IV (75 %); 115 cases (55.02 %) were overweight and obese. The proportion of patients whose diet was reduced by 25 % to 100 % compared with before accounted for 66.51 %, while the proportion of patients who had lost 5 % of weight in the past 3 months accounted for 11.00 %, and that of fluid retention was 31.57 %. Complex nutritional status requires a higher and more refined balance of nutritional support and energy requirements, fluid management and heart load.
The high nutritional risk rate is related to the serious condition of patients with severe cardiac diseases. The APACHE II score in this group of cases > 10 points accounted for 92.34 %, of which acute onset of chronic diseases and complications, diabetes, and stroke accounted for 90.61 %. Acute attacks in patients with severe cardiac disease often have infections, which increase the risk of malnutrition (7). The mechanism is that heart failure with gastrointestinal congestion and ischemia lead to poor appetite, decreased serum protein production in liver congestion, and gastrointestinal dysfunction leading to insufficient nutrient intake, digestion, and absorption. Besides, the release of inflammatory factors participates in ventricular remodeling, muscle atrophy and other aggravations of malnutrition. What is more, the application of mechanically-assisted positive-pressure ventilation therapy, analgesic and sedative drugs, and vasoactive drugs has increased the difficulty of nutritional therapy support (8). In this group of patients, invasive mechanical assisted ventilation was used for 52.63 %, analgesic and sedative drugs were used for 41.63 %, and vasoactive drugs were used for 78.47 % of subjects.
Considering the clinical harm of nutritional risks for patients, we should screen patients for nutritional risk as soon as possible. Subsequently, we can choose the appropriate nutritional pathways and nutritional preparations, and implement personalized nutritional support treatment. If enteral nutrition is difficult to implement, you can start with light enteral nutrition to gradually improve tolerance, improve nutritional status, and improve body stress protection (9). High energy-density nutritional preparations can not only improve the nutritional indicators of patients with severe heart failure, but also reduce their level of inflammatory factors to improve heart function, which is more in line with the needs of fluid intake restriction management (7,10). Resting energy expenditure (REE) is currently considered to be the gold standard for measuring human energy expenditure, especially in elderly patients (11). Studies have pointed out that the REE of hospitalized patients with different body mass index (BMI) is not the same: the average REE of patients with a BMI lower than 21 kg/m2 is 21.4 kcal/kg · d, while the average REE of patients with a BMI higher than 21 kg/m2 is 18.4 kcal/kg · d. For critically ill patients with overweight, obesity, and poor tolerance to cardiac function, nutritional support based on individual needs is more conducive to risk control. That is to prevent, manage, treat diseases and optimize health through personalized nutrition support treatment of human beings. Daily negative balance for patients to keep weight loss per week at about 0.45-0.9 kg is 500-750 kcal; in other words, that is to control daily intake at 1200-1500 kcal for women or 1500-1800 kcal for men. Especially those with BMI ≥ 35 kg/m2 need control to reduce body weight by 5 %-10 % (6). The nutritional preparations of this group of patients are mainly non-elemental and special-application high-energy density preparations accounting for 61.76 %. An 84.22 % of the achieved dose was concentrated in 500 ml-1000 ml. Promoting gastrointestinal motility drugs and probiotics can improve the control of enteral nutrition complications and promote enteral nutrition to achieve the dose target. In the choice of nutritional support for this group of patients, parenteral nutrition and supplemental parenteral nutrition accounted for 42.54 %, while only 40.35 % of patients started enteral nutrition within 48 hours. The delay in the implementation of early enteral nutrition is not conducive to the protection of intestinal barrier function, and increases the risk of intestinal bacterial translocation and infection.
The nutritional risk of patients with severe cardiac disease is positively correlated with age, and the older the age, the higher the risk (12). Malnutrition and nutritional risks are mainly manifested as hypoproteinemia, anemia, and high capacity load accompanied by deterioration of heart and kidney function, which leads to a higher prognostic risk for patients (13). In this study, the Cr and NT-proBNP values of the malnutrition risk group were higher than those of the no-risk group. B-type natriuretic peptide (brain natriuretic peptide, BNP) and N-terminal B-type natriuretic peptide precursor (NT-pro BNP) as biological markers for the diagnosis of cardiac insufficiency are widely used in clinical practice. They are important indicators for judging the severity of heart failure, risk stratification and prognosis, and to evaluate the effect of treatment. Ventricular myocytes produce amino acid residue-containing precursor B-type natriuretic peptide (pre-pro BNP) under the pathological conditions of increased ventricular pressure and volume load, and then divide it into amino acid-containing B-type natriuretic peptide precursor (pro BNP), which is cleaved into two parts under the action of endonuclease. The biologically active BNP containing amino acids and the non-biologically active NT-pro BNP containing amino acids are secreted into the blood circulation by the cardiomyocytes in equal numbers of molecules. BNP can accurately reflect the degree of cardiac insufficiency, while NT-proBNP is affected by renal insufficiency and changes more significantly (14). TC is one of the main variables that stably predicts the death of long-term hospitalized patients with heart failure (15). In this study, the TC value of the nutritional risk group was lower than that of the no-risk group, and the difference between the no-risk group and the low-risk group was statistically significant. Blood TC levels are affected by many factors such as diet, drug control, and lifestyle. Fat, cholesterol, especially saturated fatty acids, can increase blood cholesterol levels; plant-based dietary patterns, dietary fiber, plant sterols, etc., can affect the absorption of cholesterol or reduce blood cholesterol levels (16). Insufficient exogenous intake and endogenous regulatory synthesis disorders in disease states can cause blood levels to drop.
Killip's heart function classification and the NYHA classification are used to evaluate heart function — the worse the heart function, the higher the nutritional risk. Cardiac function classification can be used as a predictor of nutritional risk (13). In the subgroup with Killip cardiac function classification, the higher the nutritional risk, the lower the PA value, and the difference between the high-risk and low-risk groups is statistically significant. Lourenço et al. (17) found that patients with PA ≤ 15 mg/dL have a higher disability and mortality rate than patients with heart failure and PA > 15 mg/dL. CABASSI et al. (18) proposed that PA is a more accurate predictor of death in elderly heart failure patients with increased BNP, and is of great significance in screening and identifying high-risk heart failure patients with high nutritional risk.
In 1/3-1/2 of patients with heart failure, especially chronic heart failure combined with renal insufficiency, poor gastrointestinal function entails a risk of enteral nutrition intolerance and complications (19). The amount and rate of nutritional support and heart function influence each other. In this study, the incidence of major adverse cardiac events in severe EN cardiac patients reached 64.91 %, and the incidence of enteral nutrition-related complications was 54.39 %, which was between 36.7 % and 95.1 % in related reports (20-22). The overall hospital mortality rate of patients with severe cardiac disease is 28.23 %. The higher the nutritional risk, the higher the mortality rate, which is positively correlated with nutritional risk. The in-hospital mortality rate of EN patients with severe cardiac disease was 11.00 %, and the difference between risk groups was not statistically significant. This may be related to the small sample size, and further research is needed.
CONCLUSION
Patients with severe heart disease have a high nutritional risk with complex conditions, and the worse the cardiac function, the higher the nutritional risk. The high incidence of EN support-related complications is positively correlated with nutritional risk, and EN is difficult to implement. Early nutritional assessment and selection of appropriate individualized nutritional treatment support methods are required. Close observations should be made to strengthen the monitoring of high-risk factors and the identification and treatment of complications; to improve the quality and effect of nutritional support, and to achieve the treatment goal of improving patient outcome.