INTRODUCTION
It has been more than one year since the first case of COVID-19 was reported in Wuhan (China), causing more than 85 million of infected cases and almost 2 million deaths worldwide (1). Spain has been one of the countries more affected by this viral disease, with more than one and a half million confirmed cases and up to 40,000 deceased people (1,2). As a new disease, the factors that may influence the severity or prognosis of this disease are yet to be well stablished. However, preliminary data have shown that most people with a worse prognosis have some specific comorbidities, such as obesity, chronic obstructive pulmonary disease, cardiovascular disease, hypertension, and also diabetes (3,4).
In this sense, diabetes, with more than 460 affected million adults worldwide in 2019, is a long-standing global epidemic (5). With such a great prevalence of this metabolic disease, it is mandatory to know better the relationship between diabetes and COVID-19 (3,6-11). Actually, type-2 diabetes (T2DM) is one of the most frequent comorbidities found in patients with COVID-19. In fact, the prevalence of diabetes among subjects with COVID-19 ranges from 5 to 11 % (12,13). Most of studies have been conducted in China, but similar results have been found in the few studies performed in the USA and Europe (12,14). Also, the prevalence of diabetes was almost three-fold greater in patients infected by SARS-CoV-2 with severe disease compared with those without severity criteria (4). Moreover, the incidence of COVID-19 patients who were admitted to an ICU was twofold greater among individuals with diabetes. Furthermore, mortality rates were also higher among subjects with diabetes and COVID-19, and ranged from 22 to 31 % according to different studies (12,14). The most widely accepted hypotheses for these negative outcomes among subjects with diabetes infected with SARS-CoV-2 would be a more severe acute inflammatory response and/or prothrombotic state (11-13,15).
What is more, it remains to be elucidated whether these negative outcomes among subjects with diabetes affected by COVID-19 are secondary to either acute or chronic poor glycemic control. In this sense, results have found contradictory results not only regarding the effect of glycated hemoglobin (HbA1c) on admission (13), but also the negative impact of acute hyperglycemia (16).
Also, most of these studies have been conducted in China and only a few of them in Western countries, with results being extrapolated to other ethnicities (14).
We aimed to study whether, in a Mediterranean sample, there were any differences in clinical, biochemical, or prognostic parameters among subjects with T2DM admitted to hospital due to COVID-19 compared with patients admitted for the same infection but without this chronic condition.
MATERIAL AND METHODS
SUBJECTS
This retrospective case-control study was performed in 90 patients with T2DM admitted to a tertiary hospital due to infection with SARS-CoV-2 from April to June 2020. All patients were confirmed with COVID-19 by PCR. Inclusion criteria were: patients older than 18 years with a diagnosis of T2DM for longer than 12 months; patients were excluded from the study if they had type-1 diabetes or gestational diabetes, as were individuals with a diagnosis of T2DM in the preceding 12 months and T2DM patients during pregnancy or lactation. This group of patients was compared with 50 gender-matched patients admitted due to infection with SARS-CoV-2 without T2DM. This study was conducted according to the World Medical Association Declaration of Helsinki. The study was approved by the Ethics Committee of the hospital.
CLINICAL CHARACTERISTICS, LABORATORY VALUES, AND ANTHROPOMETRIC MEASURES
The clinical parameters included were extracted from the electronic medical records. They included demographic characteristics, comorbidities, symptoms, and treatment related to COVID-19. The latest glycated hemoglobin (HbA1c) value, microangiopathic and macrovascular complications related to T2DM, and other cardiovascular risk factors (dyslipidemia, hypertension, obesity and tobacco use) were also recorded. Blood tests performed 24 hours after admission were also extracted from the electronic system. Blood tests included blood count, coagulation, inflammatory parameters, glycemic values, lipid and renal parameters, thyroid and hepatic profiles. The latest recorded height and pre-admission weight were registered. Body mass index (BMI) was calculated as weight divided by height squared.
STATISTICAL ANALYSIS
Initial analyses were descriptive and included calculation of mean and standard deviation (SD) for continuous variables, and frequencies for categorical variables. Paired Student's “t”, chi-squared, ANOVA, and Fisher's exact tests were used to compare values of variables between groups. Pearson's chi-squared test or Fisher's exact test were used to assess the association between each of the discrete parameters and patient nutritional status. A p-value < 0.05 on the two-tailed test was considered to indicate statistical significance. Data were analyzed using the SPSS version 22 statistical software (SPSS Inc., Chicago, IL, USA).
RESULTS
Among the 90 patients with T2DM included, 57.1 % were men with a mean T2DM duration of 7.2 ± 5.7 years. Fasting plasma glucose was 142.2 ± 58.2 mg/dl and HbA1c was 6.9 ± 1.4 %. Regarding macrovascular complications related to T2DM, 24.2 % and 9.9 % had coronary and cerebrovascular disease, respectively. When taking into account microangiopathic complications, 12.9 % had diabetic nephropathy, 7.9 % suffered from diabetic retinopathy, and 14.9 % had peripheral neuropathy.
Subjects with T2DM were older than their counterparts (73.3 ± 12.4 vs 53 ± 15.7 years; p < 0.0001). Conversely, when taking into account cardiovascular risk factors, tobacco use was more frequent among subjects without T2DM (24 % vs 6.6 %: p = 0.007). Regular alcohol consumption was also more frequent among subjects without T2DM (48 % vs 0 %: p < 0.0001). However, the frequency of subjects with obesity, hypertension and dyslipidemia was greater among subjects with T2DM than among patients without it (65.9 % vs 40 %, 83.5 % vs 52 %, and 74.7 % vs 28 %; p = 0.004, p < 0.0001 and p < 0.0001, respectively).
Moreover, either coronary disease or cerebrovascular disease were more prevalent among subjects with T2DM (24.2 % vs 10 % and 9.9 % vs 0 %; p = 0.04 and p = 0.03, respectively). Also, both chronic kidney disease and depression were more frequent among subjects with T2DM compared with their counterparts (39.6 % vs 6 %; p < 0.0001, and 40.7 % vs 20 %, p = 0.02, respectively).
BMI at the time of the evaluation was significantly greater among subjects with T2DM compared with those without T2DM (33.5 ± 6.1 vs 27.1 ± 6.6 kg/m2; p < 0.0001). Also, either systolic or diastolic blood pressure were higher among patients with T2DM (137.8 ± 21.6 vs 127.1 ± 20.5 mmHg; p = 0.007, and 77.6 ± 13.6 vs 72.1 ± 14.5 mmHg; p = 0.02, respectively). Besides, the proportion of subjects with proper glycemic control during hospitalization regarding the American Diabetes Association recommendations was significantly lower among subjects with T2DM compared with those without the condition (49 % vs 82 %; p = 0.001) (Table I).
Table I. Comparison of sociodemographic features, toxic habits, anthropometric variables and cardiovascular risk factors among subjects hospitalized due to COVID-19 with and without T2DM
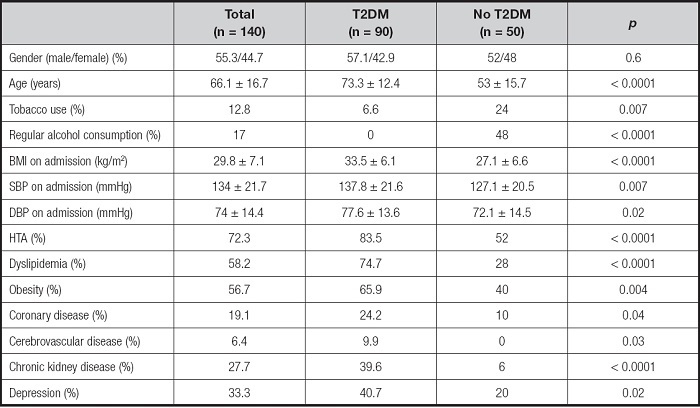
Data are mean ± SD or %. BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure.
Regarding symptoms related to COVID-19 and compared with patients with T2DM, more patients without diabetes presented fatigue (96 vs 51.6 %, p < 0.0001), headache (44 vs 17.6 %; p = 0.001), pectoralgia (58 vs 23.1 %; p < 0.0001), diarrhea (90 vs 35.2 %; p < 0.0001), nausea (52 vs 11 %; p < 0.0001), anosmia (28 vs 13.2 %; p = 0.05), and dysgeusia (50 vs 11 %, p = 0.001). No differences between the two groups were seen regarding fever, cough, dyspnea, vomiting dermatological lesions or the presence of pneumonia. On the other hand, length of stay was higher among subjects with T2DM compared with those without it (11.7 ± 7.7 vs 9.7 ± 8.6 days; p = 0.01). However, both groups were comparable regarding both the proportion of subjects with admission to ICU (16.5 vs 8 %; p = 0.1) and mortality (11 % vs 4 %; p = 0.2). Both the frequency of thrombosis and of ADRS were comparable between the group with T2DM and those without T2DM (9.9 % vs 2 %; p = 0.09, and 11 % vs 10 %; p = 0.9, respectively). Corticosteroid treatment was more frequently prescribed among patients admitted with T2DM (25.3 % vs 8 %; p = 0.01). These data are summarized in table II.
Table II. Comparison of symptoms related to COVID-19 and percentage of patients with corticosteroid treatment among subjects hospitalized due to COVID-19 with T2DM compared with those without T2DM

Data are mean ± SD or %. ICU: intensive care unit; ADRS: acute distress respiratory syndrome.
As shown in table III, numerous biochemical parameters were significantly different between patients with T2DM and those without. Either the absolute count of lymphocytes (1.1 ± 0.6 vs 1.3 ± 0.7 x 109/L; p = 0.005) or hemoglobin level (11.9 ± 1.6 vs 13.1 ± 2.1 g/dL; p < 0.0001) were significantly lower among subjects with T2DM. C-reactive protein and procalcitonin levels were greater among subjects with T2DM compared with those without the condition (91.9 ± 71.2 vs 70.1 ± 63.3 mg/L; p = 0.002 and 0.8 ± 0.3 vs 0.4 ± 0.1 ng/mL; p < 0.0001, respectively). Plasma albumin levels were lower among patients with T2DM compared with those without T2DM (3.4 ± 0.5 vs 3.8 ± 0.5 g/L: p < 0.001). When taking into account hepatic parameters, total bilirubin (0.9 ± 0.3 vs 0.6 ± 0.3 mg/dL; p < 0.0001), alkaline phosphatase (86.2 ± 72.3 vs 70.6 ± 69.5 U/L; p = 0.003) and LDH (309.4 ± 176.9 vs 269.1 ± 134.3 U/L; p = 0.04) were higher among subjects with T2DM. Creatinine levels (1.2 ± 0.9 vs 1.6 ± 1.2 mg/dL; p = 0.02) and glomerular filtration rate (66.4 ± 29.3 vs 88.9 ± 22.8 mL/min; p < 0.0001) were lower among patients with T2DM when compared with those without T2DM, whereas urea values were greater (51.5 ± 31.9 vs 36.2 ± 16.8 mg/dL; p = 0.002). No differences were seen between the two groups in the other biochemical parameters evaluated.
DISCUSSION
Our study found that patients with T2DM admitted to hospital due to COVID-19 were older and had more comorbidities than patients without it. Moreover, these subjects with T2DM had worse nutritional parameters and more acute phase reactants compared with their counterparts. However, although length of stay was greater among subjects with T2DM, either the frequency of admission to the ICU or mortality was comparable between patients with diabetes and those without this disease.
Since COVID-19 is a new disease, knowledge about prognostic factors that could affect outcomes or mortality is still incomplete and continuously evolving. Actually, many studies on COVID-19 have concluded that T2DM is associated with a severe clinical course and increased mortality. However, to date, these data are still conflicting. On one hand, most of the single studies as well as the meta-analyses published so far have included Asiatic populations, with very few studies referring to Caucasian subjects (14,17). In a meta-analysis performed by Li and colleagues, T2DM accounted for 11.7 % of ICU/severe cases and 4 % of non-ICU/severe cases. These results indicated a greater proportion of T2DM in the ICU/severe group, but did not reach statistical significance (17). Also, in another meta-analysis by Kumar et al., who included 8 studies with more than 46,000 patients, the odds ratio of severe COVID-19 was not significantly greater among subjects with T2DM (14). On the contrary, Bode et al. published a retrospective observational study including more than 1,100 patients, and found that among hospitalized subjects with COVID-19, T2DM and/or stress hyperglycemia had a negative impact on both median length of stay and mortality rate (16).
However, T2DM is more frequent among the elderly, and age, along with comorbidities, are considered to be the main risk factor for increased risk of poor outcomes and/or death among subjects with COVID-19 (13-18,19).
Besides, patients with T2DM constitute a highly heterogeneous population in terms of duration of the disease, glucose control, related comorbidities, and presence of micro or macrovascular complications, among others. Therefore, a relevant point to find out would be which of all these different factors could have an influence on the prognosis of patients with T2DM admitted due to SARS-CoV-2 infection.
It is important to point out that the patients with T2DM included in our sample had a very good glycemic control pre-hospitalization, with a mean Hba1c value below 7 %. Therefore, the prevalence of chronic complications secondary to T2DM was also low. In this sense, Bode et al. found that, among 1,122 patients hospitalized due to COVID-19, the mortality rate was four-fold higher among subjects included in the group with diabetes and/or uncontrolled hyperglycemia (28.8 %) compared with COVID-19 inpatients without evidence for diabetes or uncontrolled hyperglycemia (6.2 %). Actually, in a subset analysis of outcomes within the T2DM and/or uncontrolled hyperglycemia group, they found that 75 % of deaths occurred in patients with a diagnosis of uncontrolled hyperglycemia (16). These results could mean that, rather than T2DM, it would be poor glycemic control, either acute or chronic, that negatively could influence prognosis in these patients.
On the contrary, the CORONADO study, which was a large-scale French nationwide observational study in patients with T2DM admitted due to COVID-19, found different results when they published an intermediate analysis with 1,317 participants included. The aim of such study was to determine the risk factors that could contribute negatively to the prognosis of subjects with T2DM and COVID-19. It seems that previous glucose control does not influence negatively the severity of COVID-19 subjects with T2DM who require hospitalization. Actually, HbA1c values were not related to either the composite primary outcome or death rate. However, these preliminary results should be taken with caution as HbA1c measurements were missing in one-third of the studied population (20).
This hypothesis would make sense given the fact that a hyperglycemic state, but not T2DM per se, increases the virulence of pathogens, lowers interleukin production in response to infection, and reduces phagocytic activity and polymorphonuclear leukocytes (21,22). Moreover, the innate immune system, the first line of defense against SARS-CoV-2, is compromised mainly among patients with uncontrolled T2DM (11,23).
Patients with T2DM had lower albumin, creatinine, and hemoglobin levels compared with those without T2DM, reflecting a risk for malnutrition. Actually, the prevalence of malnutrition among subjects admitted to hospital is high, especially among the elderly. Li et al., in a cross-sectional study, evaluated the nutritional status of elderly inpatients with COVID-19 using the Mini Nutritional Assessment (MNA). They found that of a total of 182 patients included, 52.7 % had criteria for malnutrition and up to 27.2 % were at risk for malnutrition (24). Even though there is lack of evidence concerning nutritional status and COVID-19 prognosis, previous research focused on other respiratory viruses has shown that an adequate nutritional support is positive. Actually, underweight adults with any respiratory viral infection have a four times higher risk of hospitalization compared with normal-weight adults (18,24-26).
On the other hand, the clinical spectrum of COVID-19 has been shown to be heterogeneous. We found that subjects without T2DM reported more symptoms, either typical or less common, than patients with T2DM. To date, the few Asiatic studies reporting these data have not found any differences regarding COVID-19 symptoms between subjects with and without T2DM (15,18).
Moreover, acute inflammatory markers such as procalcitonin and CRP were higher among patients with T2DM. Also, bilirubin, LDH, urea, and alkaline phosphatase were higher among patients with COVID-19 and T2DM, which could indicate injury of organs other than the lungs, such as the liver or kidney. All these biochemical findings, along with older age, higher BMI, and greater prevalence of comorbidities should have increased either the proportion of patients admitted to an ICU or the mortality rate among subjects with T2DM. However, our results showed comparable outcomes in the two groups. One possible explanation could be that glycemic control among the patients included with T2DM was optimal. As mentioned before, it seems that acute hyperglycemia, more than HbA1c, could mediate the association between COVID-19 and diabetes (16).
This study has several limitations that are worth noting. It was a study conducted in a single center with a relatively small number of patients. Also a retrospective method was used in our study. Due to the isolation of these patients, capillary blood glucose determinations were irregular among all patients admitted due to COVID-19, and much of this information is lacking. However, almost all studies previously published have been conducted in Asiatic populations and, therefore, their results have been extrapolated to Caucasians. We are aware the main findings of our results are contradictory to what has already been published, but, as we pointed out, the difference could be related to glycemic control more than T2DM per se. As knowledge of this infection is still in process, heterogeneity in the results encourages future research.
In conclusion, in a Mediterranean sample, despite of age, comorbidities, nutritional status and inflammatory markers, subjects with T2DM with proper glycemic control admitted due to COVID-19 had similar prognostic outcomes than patients without this metabolic condition. Future research should focus on whether chronic glycemic control or acute hyperglycemia has any impact on the prognosis of SARS-CoV-2 infection in the Caucasian population.















