INTRODUCTION
Patient non-adherence to medical treatment recommendations from healthcare professionals is a major concern requiring additional research that would guide the implementation of strategies aimed at improving the level of patient compliance and commitment with the instructions they receive (1).
In 2003, the World Health Organization defined adherence as “the extent to which a person's behaviour —taking medication, following a diet, and/or executing lifestyle changes— corresponds with agreed recommendations from a health care provider” (2). Although nutritional therapy and lifestyle recommendations were included in this definition, current literature examining the degree of patient adherence or compliance with these recommendations is scarce (3).
Studies on medication non-adherence have identified certain patient-related characteristics that have an impact on this lack of adherence, such as age, level of education, social environment, and difficulties in understanding instructions for the management of their disease (4). Additionally, lack of communication between patients and healthcare professionals, limited consultation times, and message complexity have a negative effect on adherence (4).
The incidence of complications associated with defunctioning stoma formation in surgical patients is high (5). Dehydration and malnutrition are among the most common complications and are both intimately associated with high output stomas (HOS). Although a short self-limited high output during the first postoperative days is normal (6), an unremitting or continuous occurrence of this process requires a specific management given the associated complications, which involves identifying the cause and performing a series of actions to control it adequately (7). However, the cause is often not easy to identify. HOS triggering factors that have been described include the development of short bowel syndrome resulting from extensive intestinal resections, a flare of inflammatory bowel disease, diabetes, sudden discontinuation of drugs such as opioids or corticosteroids, or the use of prokinetics (8). Abdominal infections or obstructions have also been described as triggering factors. Furthermore, in their endeavour to establish models to predict the risk of readmissions from HOS, Chen et al. (5) identified age ≥ 65 years, female sex, arterial hypertension, and short postoperative hospital stay as predictive factors.
Many interventions aimed at reducing the incidence of HOS and improving patient nutritional status (9), such as scheduling early postoperative visits performed by multidisciplinary teams or implementing aggressive educational programmes, have been developed. These measures have been reported to have had positive outcomes on the reduction of associated readmission rates in certain studies (9).
However, not all interventions have achieved the objective of reducing readmission rates through the implementation of educational programmes, emphasizing the need for new educational strategies (10). This, together with the scarcity of published evidence on the evaluation of the level of understanding and compliance with dietary recommendations in this type of patients, highlights the need to design validated tools to assess the impact of educational interventions on health outcomes.
The objective of our study was, firstly, to evaluate the level of understanding of ostomy patients regarding lifestyle, diet, and high output stoma management recommendations provided by healthcare professionals during a nutritional consultation and, secondly, to analyse the impact of the level of understanding on the occurrence of this type of ostomy-related complications.
MATERIALS AND METHODS
PATIENTS
The study population consisted of ≥ 18 year-old patients who had undergone bowel resection with ostomy.
STUDY DESIGN
A prospective study to follow up ostomy patients at nutritional consultations in a 350-bed hospital was designed.
Based on our centre's clinical guidelines, all patients undergoing gastrointestinal resection requiring a defunctioning stoma were registered and followed up during the postoperative period to facilitate diet progression and detect potential alterations in stoma function (11). At discharge, all patients tolerated a low-residue diet. However, given the complexity of adapting to the diet after surgery and the high risk of developing complications, our hospital has defined and implemented a nutritional protocol for ostomised patients which consist of a comprehensive follow-up in outpatient clinics following hospital discharge to rapidly identify and treat any electrolyte and/or nutritional problems that may appear.
The follow-up process was performed early after hospital discharge and again one month later, as follows:
− The first follow-up visit was performed 7-10 days after hospital discharge. The patients' nutritional history was obtained and their nutritional status and dietary progression evaluated.
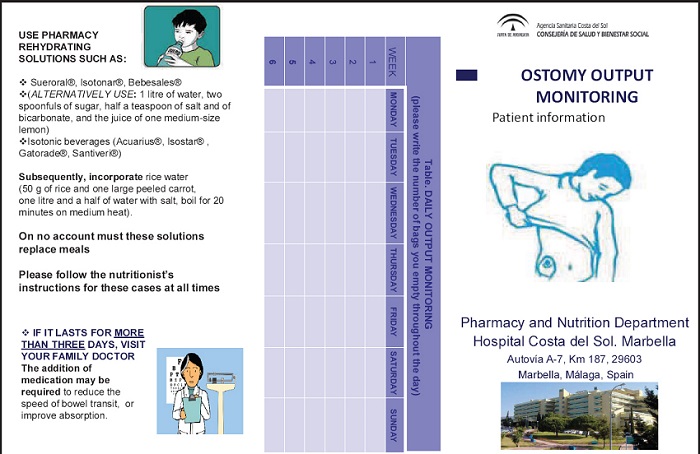
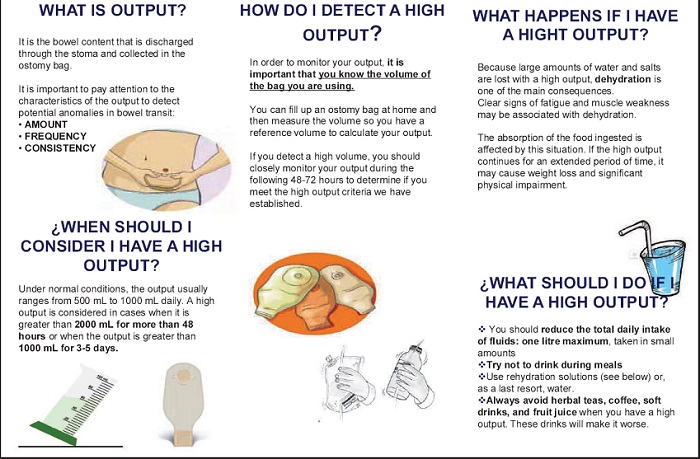
− In addition, patients were instructed in the detection and management of HOS. An information leaflet was provided (Annex I), its suitability assessed using the Suitability Assessment of Materials (SAM) scale, and its readability evaluated using the INFLESZ (Flesch- Szigriszt index) formula (12,13).
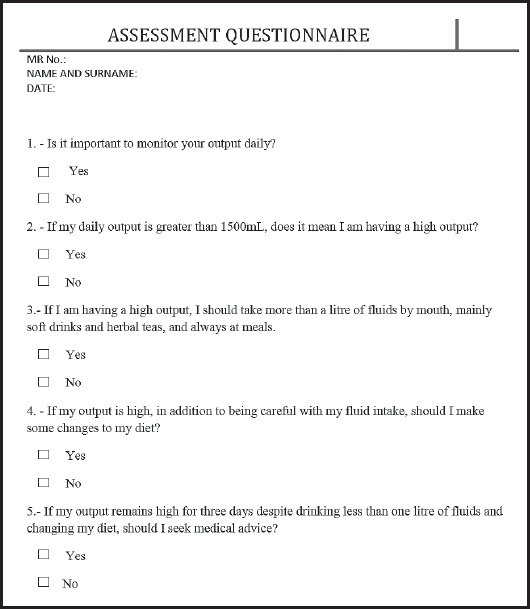
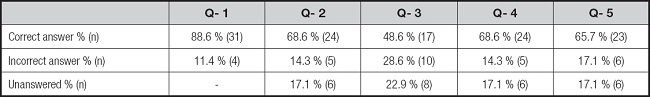
− The second visit took place one month later, with a further assessment of nutritional status and dietary progression, and the recording of any occurrences of HOS. The level of understanding of the training received during the first visit was also assessed using a five-question evaluation questionnaire with dichotomous (Yes/No) responses (Fig. 1).
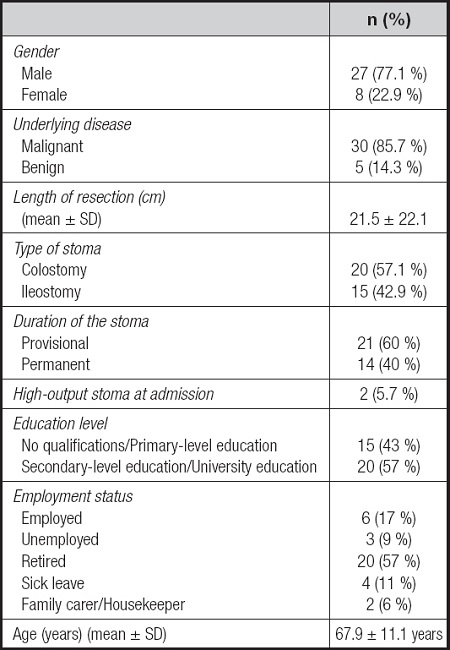
Demographic characteristics (age, sex, education level, employment status), underlying disease leading to the surgical intervention, length of resection, type of stoma, and presence of HOS after surgery were collected from electronic medical records.
The answers to each of the questionnaire's items were collected and analysed.
STATISTICAL ANALYSIS
A descriptive analysis was performed using measures of central tendency, dispersion, and position for quantitative variables, and frequency distribution for qualitative variables. To evaluate differences in the level of understanding recorded with the questionnaire, the Mann-Whitney U-test was used for quantitative variables, and Fisher's exact test for qualitative variables. Statistical significance level was set at p < 0.05.
RESULTS
The study population consisted of 35 consecutively recruited patients. Demographics are shown in table I.
EDUCATIONAL MATERIAL EVALUATION
The evaluation of the information leaflet using the 22 factors contained in the SAM scale provided a 75 % score, and therefore the quality of the material was considered superior (70-100 %). Text readability was assessed with the INFLESZ formula, and the level of difficulty was considered normal.
HIGH OUTPUT MANAGEMENT: LEVEL OF UNDERSTANDING
Of all the patients, 71.4 % (n = 25) did not provide correct answers to all the questions. Table II shows the answers to the different items of the questionnaire.
Correctness of the answers to the questionnaire showed no significant differences between the group of patients with secondary/university edcation and the group without formal education or with primary education (p = 1.00).
DISCUSSION AND CONCLUSION
Seventy percent of patients provided incorrect answers to some of the items of the questionnaire. These results evidence a lack of understanding of the information provided during the nutritional consultation and are consistent with the findings of other studies on treatment adherence, which have shown that the limitations of certain patients to understand the characteristics of their disease and the information received determines their degree of treatment compliance (1,4).
In line with this, some authors have suggested that the level of education may be a risk factor associated with non-adherence (2-13,14). However, our analysis did not identify patient level of education as a determinant of the results obtained in the questionnaire. Other studies have associated the lack of understanding not so much with education level but with a lack of commitment of the patient (6). Distrust in treatment efficacy, low motivation to recover health, and/or lack of knowledge on the consequences are all factors that may have an impact on adherence (1,15).
In addition to the patient-related factors, certain characteristics of the healthcare professionals and settings such as lack of written instructions or difficulty of the language used may compromise adherence to the instructions provided. Several tools are available to assess educational material or health information for adults (12,13). In our case, the analysis of the material prepared did not reveal a high level of complexity. However, in light of the results obtained and in line with other studies (16), our objectives regarding understanding and patient commitment with the information provided were not met. Thus, it would be beneficial to simplify the material provided to lower the level of complexity.
Furthermore, although a large number of studies on medication adherence and associated factors are readily available (1,16), evidence on adherence in the field of clinical nutrition and lifestyle and dietary recommendations is scarce (3).
The occurrence of ostomy-related complications, in particular dehydration and malnutrition secondary to HOS, can be largely prevented through patient self-care education and training (9).
Several authors have described educational programmes based on multidisciplinary teams and aimed at reducing HOS-related hospital readmission rates (9,10,18,19).
Although our study has several limitations such as the use of a non-validated measuring tool and a small sample size for subgroup comparisons, our findings reveal that new validated tools assessing the quality of clinical interventions performed to improve patient understanding and commitment with the recommendations provided are required.