INTRODUCTION
With the continued improvement of living standards, the incidence of chronic diseases such as hypertension and diabetes has drastically increased 1. In the last 30 years, the prevalence of diabetes has increased from less than 1 % in 1980 to 10.9 % in 2013. China is currently the country with most patients with diabetes 2. Additionally, the prevalence of hypertension increased from 7.73 % in 1980 to 25.2 % in 2012. In 2012, the prevalence of refractory hypertension was 14.8 % and accounted for 12.5 % of all patients with hypertension 3. Hypertension, diabetes and dyslipidemia are major factors in cardiovascular disease, sudden death, stroke, and congestive heart failure, and these factors often coexist in the same individuals (4,5).
Evidence has shown that the prevention of unhealthy dietary habits and sedentarism is crucial to hypertension and diabetes management (6,7). In a meta-analysis the DASH diet was found to result in significant decreases in systolic blood pressure (-5.2 mmHg, 95 % CI, -7.0, -3.4; p < 0.001) and diastolic blood pressure (-2.6 mmHg, 95 % CI, -3.5, -1.7; p < 0.001), and in the concentration of total cholesterol (-0.20 mmol/L, 95 % CI, -0.31, -0.10; p < 0.001) and low-density lipoproteins (-0.10 mmol/L, 95 % CI, -0.20, -0.01; p = 0.03). These changes predicted a reduction by approximately 13 % in the 10-year Framingham risk score for CVD 8. Studies have also shown that long-term adherence to the DASH diet was associated with a significantly lower incidence of cardiovascular disease as compared to regular diets 9. The DASH diet is an effective nutritional strategy to prevent CVD.
In addition, sodium surfeit and potassium deficiency are chief environmental factors in the pathogenesis of primary hypertension and the associated cardiovascular risk 10. Therefore, reducing sodium intake, increasing potassium intake, and using potassium-containing salt substitutes may be protective factors for cardiovascular disease (11,12).
Thus, the aim of this study was to evaluate the effects of low-sodium salt applied to the Chinese modified DASH (CM-DASH) diet on atherosclerotic cardiovascular disease (ASCVD) risk in patients with diabetes and hypertension.
METHODS
PARTICIPANTS
Targeted telephone number lists and face-to-face interviews were used to recruit participants from community centers in the Nan'an District of Chongqing. Inclusion criteria required that participants be: 1) aged ≥ 50 and ≤ 75 years; 2) residents near the hospital with no plans to withdraw or go out during July-October 2020, who can be regularly followed up; 3) hypertensive patients with type-2 diabetes (the diagnostic criteria for hypertension are based on the Chinese Guidelines for the Prevention and Treatment of Hypertension (2018 Revised Edition) (13), and the diagnostic criteria for diabetes are based on the Chinese Guidelines for the Prevention and Treatment of Type-2 diabetes (2017 Edition) [14]) who currently are regularly taking antihypertensive drugs/hypoglycemic drugs; 4) to strictly abide by the two daily meals provided by us in the course of the study; and 5) all the subjects and their family members living together signed an informed consent. Exclusion criteria were: 1) patients with a malignant tumor, acute myocardial infarction, stroke within 3 months, or other serious diseases, and expected survival time less than 1 year; 2) patients with hypercortisolism or hyperaldosteronism; 3) acute diseases such as upper respiratory tract infection, fever, severe diarrhea; 4) deaf-mute people, patients with dementia, and those with serious depression or other mental disorders who cannot communicate normally; 5) mobility issues and inability to follow up on time; 6) stage 3 or above chronic renal failure or renal replacement therapy; 7) abnormal liver function; 8) abnormal blood potassium or is taking potassium diuretic drugs; 9) women who are pregnant or may become pregnant; 10) attending to participate in other clinical studies; 11) other ineligible conditions as adjudicated by investigators.
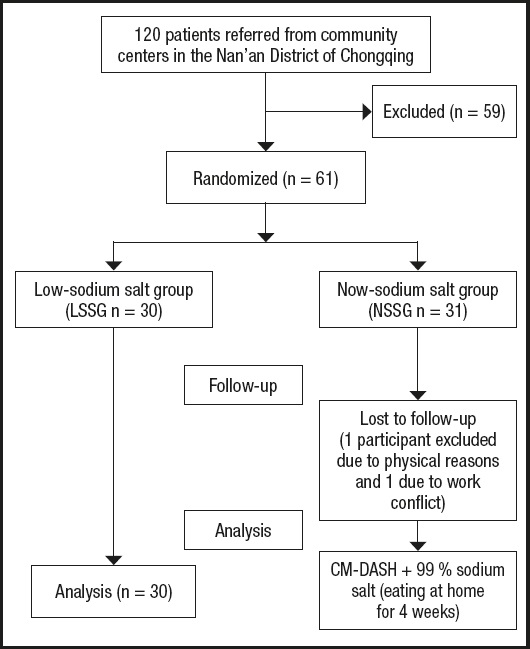
A total of 61 patients met the inclusion criteria and were randomly assigned to the low-sodium salt group (LSSG) or the normal-sodium salt group (NSSG). All participants and their families signed a written informed consent before enrollment in the trial. The study details are better shown in figure 1.
STUDY DESIGN
This was a randomized, single-blind trial. Participants were randomly assigned to either the LSSG (n = 31) or NSSG (n = 30). Randomization was performed using a random numbered table. The study protocol was approved by the Ethics Committee of Chongqing Medical University (approval date: 2020.07.28), which means that all procedures reported in this submitted paper were conducted in an ethical and responsible manner, and in full compliance with all relevant codes of experimentation and legislation. Trial registration: ChiCTR2000029017. Registered on January 11, 2020; prospective registration, http://www.chictr.org.cn/. All participants and their families signed a written informed consent before enrollment in the trial.
PROCEDURE
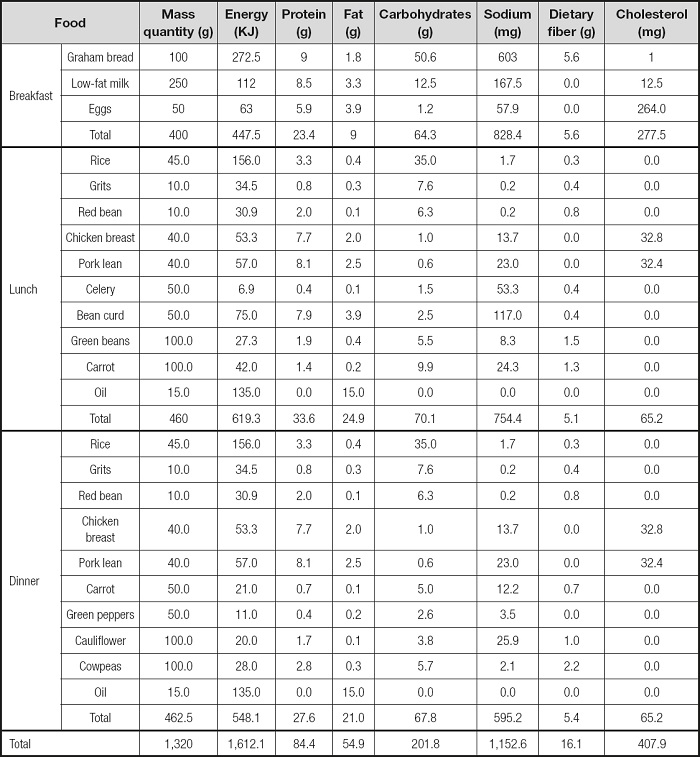
Participants were allocated to the LSSG or NSSG. Patients in the LSSG were given the Chinese Modified DASH (CM-DASH) diet plus low-sodium salt (52 % sodium chloride) whereas in the NSSG they were given the CM-DASH diet plus normal-sodium salt (99 % sodium chloride). The doses of salt used for both groups consisted of 5 g daily for 8 weeks, based on the WHO recommendation 15. The low-sodium salt “Mushroom Chef” was developed by the Shanghai Institute of Ecological Health Sciences. Name: solid compound seasoning; executive standard: Q/BAAM0009S; food production license number: SC10334042205441; main ingredients: potassium chloride (31 %), sodium chloride (52 %), carbohydrates (9.2 %), and protein (4.4 %). The normal-sodium salt “Jingxin” was developed by the Chongqing Salt Industry Group Co., Ltd. Name: pure salt; product standard: NY/T1040; sodium chloride content: 99 %. Diet instructions and recipes were the same for the two groups. Food selection recommendations were as follows: 1) staple food: coarse grain: fine grain = 1:1:1; 2) lean meat with a preference for white meat (chicken or fish); 3) choosing low-fat milk; 4) moderate consumption of nuts; 5) 25 to 30 g of oil; and 6) 5 g of salt. One of the CM-DASH recipes is included in table I.
DATA COLLECTION
Outcome variables were assessed at baseline and after the intervention. Ten-year ASCVD risks were measured using a tool for risk assessment and health guidance on cardiovascular and cerebrovascular diseases in Chinese people developed by the Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) project. This tool is suitable for people over 20 years old with no history of cardiovascular or cerebrovascular diseases (16,17). To calculate the 10-year-ASCVD risk, we logged into https://www.cvdrisk.com.cn/ASCVD/Eval and provided data on age, gender, place of residence, waist circumference, TC, HDL-C, SBP, DBP, whether the patient used antihypertensive drugs, whether the patient was diagnosed as having diabetes, whether the patient smoked, and whether the patient had a family history of cardiovascular disease.
STATISTICAL ANALYSIS
All statistical analyses were performed using the SPSS Advanced Statistics version 24.0 (IBM, Armonk, NY, USA). The Shapiro-Wilk test and Levene's test were used to test the normal distribution and homogeneity of variance, respectively. The measurement data of the normal distribution were expressed as mean and standard deviation. Within-group changes after the intervention were estimated using a paired t-test. One-way ANOVA was used to compare the difference between the two interventions. The level of significance was set at p < 0.05.
RESULTS
A total of 61 participants were enrolled in this study whereas 59 participants (26 men and 33 women) completed the study; 1 patient left the study at week 1 due to a work conflict and 1 patient left the study at week 2 due to physical reasons. A flowchart of participant enrollment and follow-up procedures is provided in figure 1. The characteristics of participants are summarized in table II. The mean age of the population was 69.03 (4.12) years, with 42.4 % of male and 100 % of elderly people. All patients suffered from hypertension and type-2 diabetes.
Table II. Baseline characteristics of patients*.
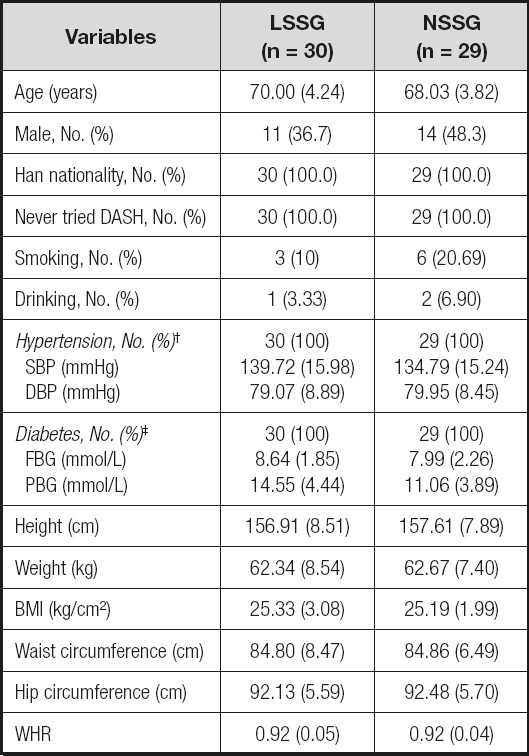
SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood glucose; BMI: body mass index; WHR: waist-to-hip rate.
*Values are expressed as mean (SD) or frequency (%).
†Hypertension was defined as an average systolic blood pressure > 140 mmHg or an average diastolic blood pressure > 90 mmHg.
‡Diabetes was defined as fasting blood-glucose ≥ 7.0 mmol/L or postprandial blood-glucose ≥ 11.1 mmol/L.
Tables III and IV show the effects of LSSG and NSSG on the observation index. The within-group analysis showed that, compared to baseline, the LSSG significantly decreased their 10-year ASCVD risk (-1.78 %; p = 0.000), BMI (-0.25; p = 0.040), SBP (-14.32 mmHg; p = 0.000), DBP (-6.32 mmHg; p = 0.000), FBG (-0.75 mmol/L; p = 0.013), PBG (-4.50 mmol/L; p = 0.000), urinary sodium (-23.41 mmol/day; p = 0.015) and sodium/potassium (-1.28; p = 0.000); the NSSG significantly decreased their 10-year ASCVD risk (-1.17 %; p = 0.000), SBP (-10.98 mmHg; p = 0.000), DBP (-5.24 mmHg; p = 0.000), FBG (-0.69 mmol/L; p = 0.030), PBG (-2.42 mmol/L; p = 0.000), TC (-0.38 mmol/L; p = 0.042) and NHDL-C (-0.37 mmol/L; p = 0.038). Besides, the LSSG significantly increased their HC (4.10 cm; p = 0.000) and urinary potassium (11.51 mmol/day; p = 0.028), while the NSSG significantly increased their HC (4.10 cm; p = 0.002) and WC (1.51 cm; p = 0.007).
Table III. Effects of 8 weeks of low-sodium salt and normal-sodium salt: within-group analysis*.
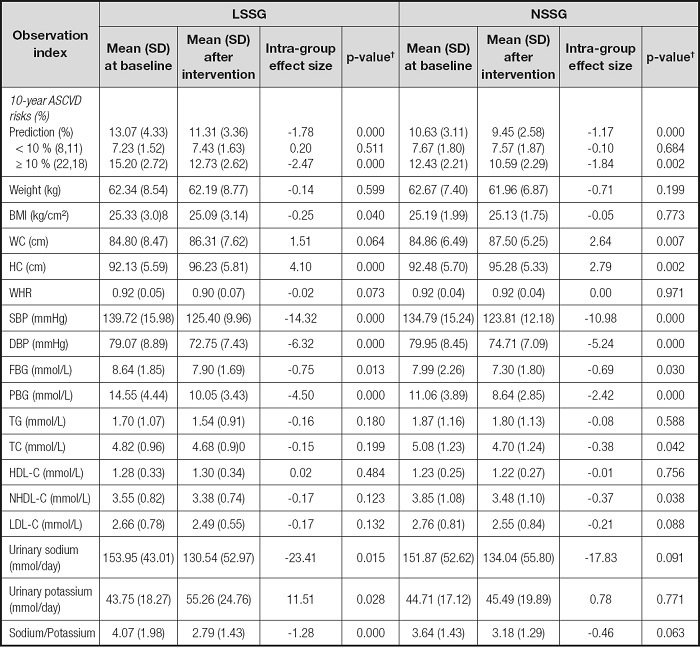
*Values are expressed as mean ± SD;
†p-value from paired t-test; LSSG: low-sodium salt group; NSSG: normal-sodium salt group; ASCVD: arteriosclerotic cardiovascular disease; BMI: body mass index; WC: waist circumference; HC: hip circumference; WHR: waist-to-hip rate; SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood glucose; TG: triglycerides; TC: total cholesterol; HDL-C: high-density lipoprotein cholesterol; NHDL-C: non-high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol.
Table IV. Effects of 8 weeks of low-sodium salt and normal-sodium salt: between-group analysis*.
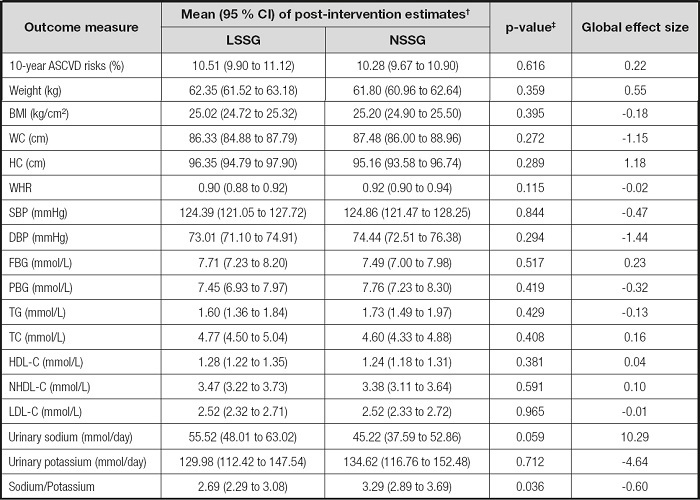
*Values are expressed as mean (95 % CI);
†Mean (95 % CI) from one-way ANOVA;
‡p-value from one-way ANOVA; LSSG: low-sodium salt group; NSSG: normalsodium salt group; ASCVD: arteriosclerotic cardiovascular disease; BMI: body mass index; WC: waist circumference; HC: hip circumference; WHR: waist/hip rate; SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood glucose; TG: triglycerides; TC: total cholesterol; HDL-C: high-density lipoprotein cholesterol; NHDL-C: non-high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol.
The between-group analysis results did not show any statistically significant differences for any observation index except for urinary sodium/potassium (0.10; p = 0.042).
DISCUSSION
Numerous studies have shown that the DASH diet and avoidance of high salt intake are protective factors for cardiovascular disease risk and hypertension (8,18), which may be related to the DASH diet's high levels of fruits, vegetables and potassium, and low levels of sodium, saturated fatty acids and sugars. Saturated fat is associated with high levels of inflammation, which may be a cause of CVD risk and insulin resistance 19. A diet high in free sugars contributes to fat regeneration and liver fat, and the conversion of free sugars and refined starches to fat produces saturated fat, which is a known risk factor for cardiovascular disease (20-22). Fruits and vegetables are beneficial because they are sources of dietary fiber, vitamins, minerals, and antioxidants (23,24). Research has emphasized that dietary fiber benefits cardiovascular health by improving blood lipids and lowering blood pressure; low dietary fiber intake is associated with a higher risk of cardiovascular disease (25-28). Studies have proven that potassium intake significantly reduced blood pressure in various populations without changing sodium intake (29,30). A meta-analysis of 12 studies indicated that an increased potassium intake and decreased sodium potassium ratio were associated with reduced risk of hypertension, cardiovascular disease, and especially stroke 30.
However, current studies on the relationship between sodium intake and cardiovascular disease are still controversial, mainly whether there is a J-shaped curve. Multiple studies have confirmed that excessive sodium intake is closely related to hypertension and increased risk of CVD, but some studies have shown that long-term low sodium intake may result in activation of the renin-angiotensin-aldosterone system (RAAS), which may lead to an increased risk of CVD 31. In this study, after 8 weeks of the CM-DASH diet formula and low sodium salt intervention, the blood pressure, blood glucose, and cardiovascular disease risk of subjects showed a trend of decline. This may be due to the fact that the urinary sodium excretion of subjects was 3.5 g/day and 3 g/day before and after the intervention, respectively, which are higher than the J-type curve low sodium intake. Besides, this study lasted only for 8 weeks, and long-term effects need further research.
In addition, the within-group comparison showed that the waist circumference of subjects in the LSSG, and the waist circumference and hip circumference of subjects in the NSSG increased, while the BMI of subjects in the LSSG decreased. Considering that the weight of subjects in both groups decreased after the intervention (although not significantly), we believe that the measurement error might be caused by a thicker clothing of subjects.
Although urine sodium and urine sodium/potassium ratio decreased in the LSSG after the intervention, there was no significant difference in urine sodium between the LSSG and NSSG, which may indicate that the low-sodium formula salt with a sodium chloride content of 52 % has limited effects on reducing sodium intake, which is consistent with our expectation. However, for this study we chose to use this salt to avoid potential adverse effects that could result from excessive intake of potassium or inadequate sodium intake, also considering subject compliance. In addition, the urinary sodium of subjects in both groups was still higher than we suggested. Although subjects were advised to avoid other salty seasonings, a follow-up survey found that some subjects still used soy sauce and fermented black beans.
In any case, our study is important because it may benefit people at high risk of cardiovascular disease such as hypertension and diabetes. In addition, the economically feasible dietary therapy provided by this study may help reduce the burden of chronic disease.
This current study has several limitations. First of all, its small sample size may hide some relevant findings. Second, 52 % low-sodium formula salt has limited effects on reducing sodium intake. Third, 8 weeks of intervention were not enough to detect changes in certain indicators.
CONCLUSION
Salt limits and DASH diets reduce the risk of cardiovascular disease while low-sodium salt containing 52 % sodium chloride did not significantly lower the risk of cardiovascular disease when compared to regular salt. Due to the limitations of the research, additional studies will be necessary to confirm our findings.