INTRODUCTION
Providing the nutritional needs of hospitalized patients is considered to be a fundamental approach to facilitate recovery from illness (1). Malnutrition, which can be considered as undernutrition in hospitalized patients (2), occurs at a frequency of about 37 % to 82 % in hospitals worldwide, varies according to the investigated population and the definitions for malnutrition used (3). Most studies conducted in Iran reported that the nutritional status of hospitalized patients is not favorable (4,5). Malnutrition is a costly disorder because of delayed recovery, increased length of hospital stay (LOS), and increased readmission rate (6). Poor food intake during hospitalization can lead to increased infections, poor wound healing, cardiac complications, and a higher mortality rate (3).
The most common nutritional risk factors in the hospitalized patients include lack of early detection and treatment of malnutrition, inadequate nutritional screening, prolonged nil by mouth status, missed meals due to medical procedures, poor appetite, food wasting, limited dietary options, and nutritional inadequacy of hospital meals (7). High quality nutritional practices in the hospital such as early nutritional screening, early diet therapy, and monitoring of nutritional status may improve the care processes and health outcomes (8). Assessment of the nutritional status of patients who are hospitalized should be considered as an integral part of the health assessment as soon as the patients are admitted to the hospital and should continue to be monitored throughout their hospitalization (1). Dietary practices need a multidisciplinary team to address a patients' nutritional needs and improve their health status and minimize hospital acquired risks associated with poor nutrition (9).
Dietitians are a professional group who are educated to provide individualized nutritional assessment and treatment in hospital settings. A physician referral is commonly required to involve nutrition services in the care of a patient. However, the dietitian's clinical roles are sometimes underestimated by physicians in different situations, resulting in potentially inappropriate referrals and inadequate nutritional support (10). Many studies reported that early involvement of a dietitian can reduce LOS, decrease infection, and promote healing (11). For example, a recent study indicated that enteral nutrition, which is frequently used in critically ill patients, was more effective when the formula was prescribed by a dietitian compared by a physician. The result showed that dietitian-supervised patients received 10 % more energy and protein, and had an increased body weight and a shorter LOS (12). Another study reported that parenteral nutrition prescription provided by a dietitian compared with a surgeon resulted in a higher intake of vitamin B complex and lipids, and better patient clinical parameters such as fewer secondary infections, less weakness, rapid recovery, and reduced patient mortality (11). Therefore, considering the views of dietitians on the nutritional status of patients and clinical nutrition services provided in the hospital may promote the proper re-orientation of treatment policies. However, few studies have been conducted on the status of clinical nutrition services in hospitals (6). So, this study aimed to assess the status of nutrition care services and diet therapy in public hospitals of Guilan province, Iran.
METHODS
STUDY DESIGN AND DATA COLLECTION
This cross-sectional study was carried out from 1th October 2019 to 1th December 2020 in public hospitals of Guilan province, Iran (n = 26). The public hospitals of five cities including Siahkal, Astara, Talesh, Rudsar, and Fouman were excluded from the study due to lack of data, and three hospitals -Manjil, Rezvanshahr, and Rostamabad- were excluded from the study due to lack of a resident dietitian. Finally, eighteen hospitals including eight hospitals of Rasht city (Razi, Velayat, Poursina, Heshmat, Alzahra, Shafa, Amiralmomenin, and Hefdah shahrivar), two hospitals of Lahijan city (22-Aban and seyedalshohada), and the hospitals of Amlash, Roudbar, Sowmesara, Bandare Anzali, Astaneh, Langeroud, Masaal, and Shaft cities were included in the study. Data was collected using a validated hospital nutrition assessment questionnaire (HNAQ) with 21 items, which was completed by visiting the hospitals and an -depth interview with the hospitals' dietitians. The HNAQ has four domains including referral system, involvement of hospital staffs in clinical nutrition, the status of clinical nutrition staff, and enteral and parenteral nutrition. The referral system subscale means to refer to a dietitian for nutrition counseling any patient who has one or more of 18 special clinical conditions including the need for enteral and parenteral nutrition, diabetes, hypertension, cardiovascular disease, cancers, burns, stroke, renal failure, hemodialysis, cirrhosis, organ transplants, bed sores, malnutrition, neurologic diseases, abdomen surgery, chronic obstructive pulmonary disease, and head trauma: referral of a patient with malnutrition, and referral of new case patients to the ICU after 24 hours of hospitalization.
The involvement of the hospital staff in clinical nutrition was defined as compliance with the dietary plan, approval of a clinician to implement the diet provided by a dietitian, proper implementation of the diet by the ward nurse, filling specialized nutrition assessment forms, and record nutrition-related information in the hospital information systems (HIS).
Status of clinical nutrition staff describes an adequate number of dietitians as compared to the number of active hospital beds, the effect of regular and principled referral of patients for nutrition counseling in improving a patient's condition and reducing LOS, and improving the position of dietitian in the hospital. Furthermore, the status of parenteral and enteral nutrition was defined according to the items included separated gavage room, providing gavage feeding with a commercial formula, providing gavage feeding with a manual formula, providing supplements needed in enteral nutrition and vitamin and mineral vials in parenteral nutrition. The questionnaire is on a five-point Likert scale from never (0) to always (4). Generally, “never” and “few” were considered as unfavorable situation, and “always” and “high” were considered as desirable situation.
INTERVIEW GUIDE
A semi-structured interview was used to direct the interviews toward the dietitians' experiences about the nutritional status of their hospital by asking open-ended questions to clarify aspects that came up in the interviews. The interview contains two main topic areas included the participants' experience of problems and their helpful suggestions improving for nutritional services of the hospitals. The interview will be transcribed verbatim, deidentified, and integrated with written field notes following each interview.
STATISTICAL ANALYSIS
Descriptive statistics were used to describe the characteristics of the status of nutrition care services and diet therapy in the hospitals. The frequency of nutritional care service problems in four different domains was calculated. All statistical analyses of descriptive statistics were performed with IBM SPSS version 22.
Regarding qualitative data, we transcribed all the interviews, reviewed the transcriptions for accuracy, and anonymized them. We enacted the criterion for credibility through open-ended questioning, spending a prolonged amount of time with the material, and giving a detailed description of the methods. To meet the criterion for transferability, we present detailed and in-depth descriptive data and quote the participants in the text. To meet the criterion for dependability, each transcription was independently read, checked, and coded by two of the authors.
RESULTS
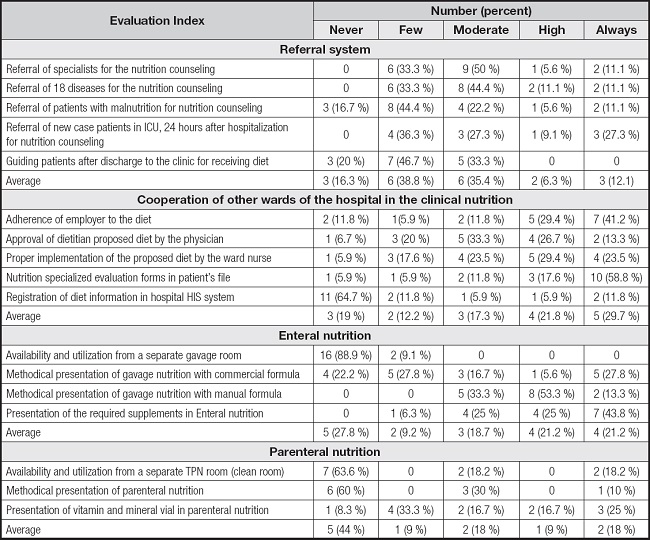
The situation of clinical nutrition in hospitals was assessed in four different domains (Table I). Regarding the referral of patients for receiving nutritional counseling, patients were not referred or were rarely referred to the nutrition specialist in more than 33 % of the hospitals. The average referral of specialists for nutri- tion counseling, referral of 18 special clinical conditions for nutrition counseling, and referral of patients with malnutrition for nutrition counseling were in a desirable situation only in 18.4 % of hospitals (Fig. 1).
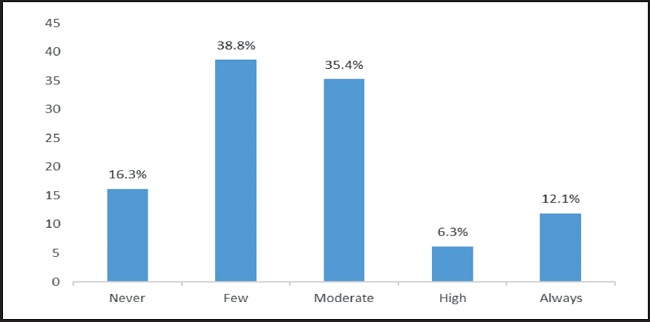
Figure 1. The status of the referral of patients for nutrition counseling in the hospitals of Guilan, Iran.
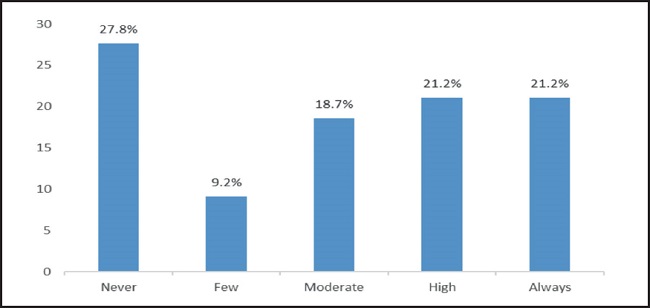
The cooperation of personnel from other parts of the hospital with the hospital dietitian was insufficient in 48.5 % of hospitals. The adherence of employers to a diet was reported as desirable just in 5 percent of the hospitals (Fig. 2).
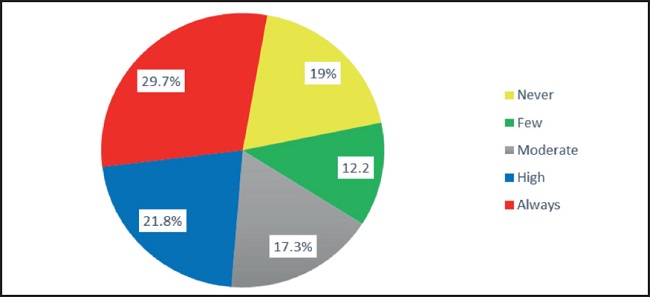
Figure 2. The status of cooperation of other hospital sections with dietitians in the hospitals of Guilan, Iran.
Regarding artificial nutrition, enteral nutrition was properly provided in about 40 % of hospitals with ICU ward (Fig. 3). Only about 17.7 % of hospitals in Guilan provided proper parenteral nutrition for patients.
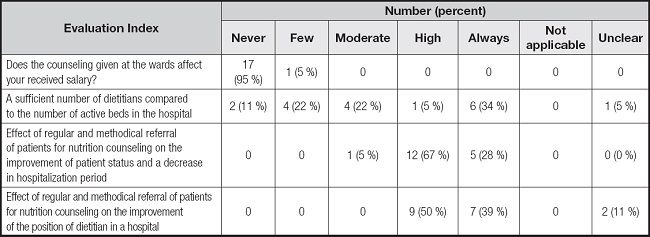
In terms of the situation of the nutrition staff at the hospital, the number of dietitians in about one third of hospitals was less than the desirable number (at least one person per 100 active beds) (13).
According to the qualitative interview and scoring of the collected comments, approximately all dietitians confirmed the effect of regular and methodical referral of patients for nutrition counseling in the improvement of patient health status. In none of the studied hospitals, the dietitians were paid with per case payment methods for their counseling sessions (Table II).
The most common problems reported by the dietitian in the hospitals were included non-adherence of the employer of the food services from the dietary plan as lack of payment of counseling fees as per case payment to dietitians (Table III).
Table III. Hospital dietitians' perceptions of the problems existing in the clinical nutrition department of public hospitals in Guilan province, Iran.
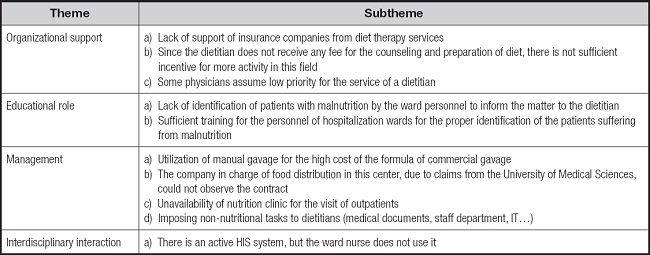
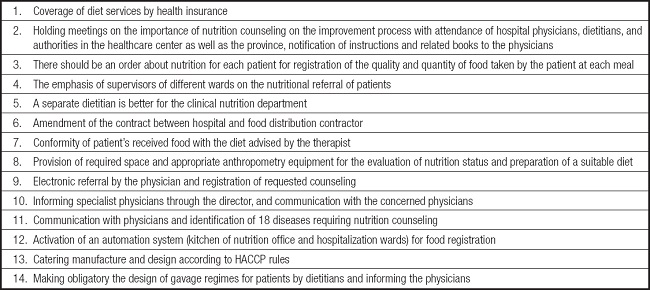
On the other hand, suggestions by dietitians for the improvement of the existing situation are presented in table IV. Some major points were related to lack of clearly defined responsibilities, lack of co-operation among all staff groups, and lack of involvement of hospital management.
DISCUSSION
The main aim of the present study was to explore the status of nutrition care services and diet therapy in public hospitals of Guilan province, Iran. The results of this study indicated that almost 50 % of patients were not referred for further assessment by dietitians in public hospitals in Guilan, Iran. Some studies reported that hospitalized patients in developing countries are at a high risk of malnutrition (14), and this situation can be associated with higher rates of some complications such as increased nosocomial infection and mortality (15).
The patients at risk of malnutrition are supposed to be referred to specialists for nutritional assessment and intervention. Nutritional assessment usually includes anthropometric, dietary, and biochemical measurements and medical history (16). A cross-sectional description showed that nutrition counseling and diet therapy in patients reduced the prevalence of malnutrition and improved weight gain (17). So, comprehensive nutritional assessment by a dietitian should be performed in those patients identified as at risk of malnutrition or who are malnourished using many items for assessing clinical status such as clinical history, physical examination, body composition measurements, and functional and laboratory assessments. The most common reasons given for lack of dietary practices were reported to be insufficient knowledge, low priority, unclear assignment of responsibility, and lack of procedures or guidelines (11).
The results of the present study showed that the shortage of facilities for managing food service operations, such as parenteral nutrition and enteral nutrition (PN/EN) preparation, is a common problem in hospitals of Guilan province, Iran. One of the main roles of the nutrition department in hospitals is involving in PN/EN preparation (18). PN/EN assessments should involve medical, nutritional, and pharmacological considerations as well as physical examination, anthropometric measurement, and laboratory data (11), which are mainly dependent on the specialized skills associated with dietitians (18).
According the results of this study, in 31.2 % of the hospitals, the cooperation of other departments in the field of clinical nutrition was insufficient. Clinical dietitians help hospital patients to determine their nutritional needs in interaction with another healthcare worker such as physicians and nurses (19). This interaction helps to develop appropriate nutritional programming for patients and track their progress (20). Clinical dietitians may also review laboratory tests ordered by physicians (11). Therefore, inter-departmental cooperation is crucial for the optimal performance of the duties of a dietician.
In this study, the number of dietitians in the hospitals was below international standards. Pan et al. investigated the status of the clinical department in Jiangsu, China (21) and reported that the nutrition departments of Jiangsu had some problems in different aspects. Nutrition departments did not have a clear department definition and the management and development of nutrition departments were confusing. Also, the ratio of dietitians per hospital bed was far from the standard levels of the hospitals in Jiangsu, China (18). The departments of nutrition in hospitals need enough human resources to improve the provision of nutrition services in hospitals. This study indicated that, compared to a similar study in 2018, the number of total human resources in clinical nutrition departments was increased. However, the most growth of human recourses was related to an increased number of clinicians and nurses instead of dietitians (22). Um et al. indicated that the hospitals of Korea had a low performance rate regarding nutritional care and there were large variations in the quality of nutritional service between hospitals (23). Rasmussen et al. found that nutrition departments in Danish hospitals did not follow the standards for nutrition support according to the established criteria (24).
In the present study, lack of organizational support was considered as the most important problem of nutritional services by hospital dietitians.
In Iran, the hospital dietitian is responsible for several duties, such as monitoring the process of receiving and buying foods, monitoring storage, preparing and transporting raw or processed foods, monitoring the preparation of gavage solution, monitoring food cooking, nutritional assessment of the patients and designing the food plan of the patients and staff, and follow up of nutritional status of hospitalized patients. Due to lack of sufficient staff for the number of active beds in the hospital, the multiplicity of responsibilities of dietitians, and the lack of per case payment method (dietitians have a fixed salary), providing a specialized diet for the patients may not be done properly in many hospitals.
Overall, the results of the present study showed that the nutritional status of public hospitals in Guilan province of Iran was not favorable. However, the present study had some limitations. First, this study was conducted only in public hospitals and cannot be generalized to private hospitals. Secondly, some hospitals in different cities of Guilan province were excluded from the study for various reasons, such as lack of access to information and lack of a resident dietitian in the hospital, and this may affect the accuracy and generalizability of the results.
Also, this study focused on the status of providing clinical nutrition services in hospitals, and the nutritional status of the patients has not been studied. Future more comprehensive studies may be effective for better policy-making and order to improve clinical nutrition in hospitals.
CONCLUSION
The status of clinical nutrition in the Guilan public hospitals of Guilan, Iran was inadequate in terms of most of the evaluated indicators. Providing appropriate training to hospital staff, specialists, and nurses, as well as providing a sufficient number of dietitians to hospital, per case payment method for nutrition counseling, of the hospital catering department may improve the situation of clinical nutrition in hospitals.
Ethics approval and consent to participate.
The research was performed in accordance with institutional regulations after protocol review and approval by the Medical Ethics Committee of the Shahid-Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.NNFTRI.REC.1400.033).