INTRODUCTION
Bronchial asthma is one of the most common chronic diseases in childhood, ranking among the top 20 conditions worldwide for disability-adjusted life years in children (1). In Chile, a significant increase in the rate of hospitalization for asthma in children has been observed, reaching a figure of 7.8 per 10,000 in 2014 (2). On the other hand, hypovitaminosis D is a major health problem that affects more than 2 billion children and adults worldwide (3). Vitamin D (vitD) has multiple functions in the health of children and adolescents. In addition to its importance for the metabolism of calcium and phosphorus, it is an important immunomodulator and has effects on the development of autoimmune diseases, some cancers, insulin resistance, and cardiovascular health, respiratory tract infections and wheezings (4-6).
In recent years, numerous prospective and retrospective studies have been published that demonstrate an increased risk of exacerbations and hospitalizations for asthma in children with hypovitaminosis D (7,8). This is probably due to an immunomodulatory effect of vitD on T helper 1, 2 lymphocyte function and on regulatory T cells (9).
In a pilot study carried out 2 years ago at Hospital Clínico Universidad de Chile (HCUCH), we were able to verify that 62 % of asthmatic children who were hospitalized had hypovitaminosis D (deficit or insufficiency of vitD) and that this deficit was associated with poor control of the disease (10).
The objective of the present study was to evaluate the risk of hypovitaminosis (vitD < 30 ng/ml) and vitD deficiency (< 20 ng/ml) in a group of asthmatic children of similar socioeconomic status who were hospitalized at the HCUCH University Hospital and at the Roberto del Río Public Hospital (HRRIO), in relation to the same number of asthmatic schoolchildren who were controlled at the outpatient level in these hospitals, and who did not underwent hospitalization in the last 12 months prior to the study. Sociodemographic and clinical characteristics were analyzed and the association between hypovitaminosis D and nutritional status and severity of hospitalization was evaluated.
MATERIAL AND METHODS
A descriptive, analytical, case-control study was carried out between May 2017 and May 2018. The sample size of 54 patients was calculated for each group considering a power of 80 % with a significance level of 0.05, and a difference of 27 percentage points in the frequency of hypovitaminosis D in hospitalized asthmatics (H) versus those treated as outpatients (A). The project was approved by the ethics committee of both hospitals.
Patients between 5 and 15 years of age were recruited, who were treated consecutively either as inpatients or as outpatients at the bronchopulmonary clinic of HCUCH and HRRIO. After signing an assent or informed consent form, a sociodemographic data survey and asthma control questionnaire were applied using the Asthma Control Test (ACT) (11,12). A complete physical examination and calculation of BMI (body mass index) was performed to then make a diagnosis of nutritional status according to the WHO 2007 curve (13). A blood sample was taken from the patients to measure the serum concentrations of vitD. Aliquots were processed in the HCUCH Endocrinology laboratory using the electro-chemiluminescence technique (14). Patients with hypovitaminosis D (vitD < 30 ng/ml) were treated, administering vitamin D3 cholecalciferol 2,000 IU per day for 2 months, as indicated by expert recommendation (15). Calcium intake and supplementation was not evaluated in this study.
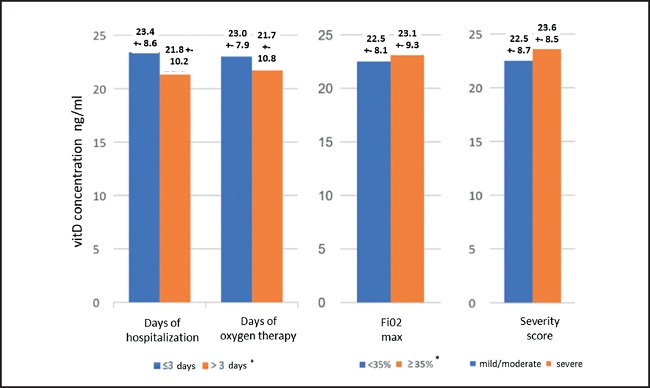
A severity score was recorded for those children who required hospitalization due to an asthmatic crisis. The score included: total number of days of hospitalization, total number of days with oxygen requirement, maximum inspiratory fraction of oxygen (FiO2max) reached, and need to transfer to the critical patient unit (mild score: 0-3, moderate: 4-6, severe: 7-14) (16).
Statistical calculations were performed using the Stata 14 package. The association between quantitative variables was assessed through the t-test and using the chi-squared test for categorical variables. Logistic regression was used to estimate the risk of deficiency and hypovitaminosis D, with a significance of p < 0.05.
This protocol was approved by the research ethics committee of HCUCH (Acceptance number, 874/17)
RESULTS
A total of 117 subjects entered the study, 64 % male and 9 years old on average; 67 % of the patients were hospitalized during the months with the lowest exposure to UVB radiation (May to November). More than half of the patients presented excess malnutrition without significant differences according to group (H/A) or sex. In all, 55 % had poor control of their disease (ACT ≤ 19), with no differences in average score according to group. The majority had a diagnosis of allergic rhinitis, the highest percentage in A patients (p < 0.05). The high frequency of underdiagnosis of the disease stands out, which was higher in group H (p < 0.05). Most of the patients had moderate asthma at the time of recruitment, this percentage being significantly higher in group H.
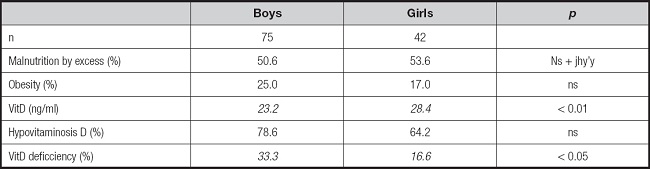
We found a high frequency of hypovitaminosis D in the patients studied (vitD < 30 ng/ml). Although we did not find any differences in the frequency of hypovitaminosis D (deficiency and insufficiency) between the groups, the deficit (vitD < 20 ng/ml) in H patients was significantly higher, and the average level of vitD was significantly lower in this group of children (Table I). When performing the analysis separately according to UVB exposure, there were no differences in the mean concentration of vitD, nor in the percentages of hypovitaminosis according to group; however, in months with lower UVB light levels, the deficit of vitD in hospitalized patients triples the deficit in patients A (p < 0.05) (Table II). We did not find any significant differences in the percentage of hypovitaminosis D according to sex; however, the mean concentration of vitD was lower and the percentage of deficit was higher in men (Table III).
Table I. Characterization of children with asthma treated at the Clinical University of Chile and Roberto del Río hospitals.
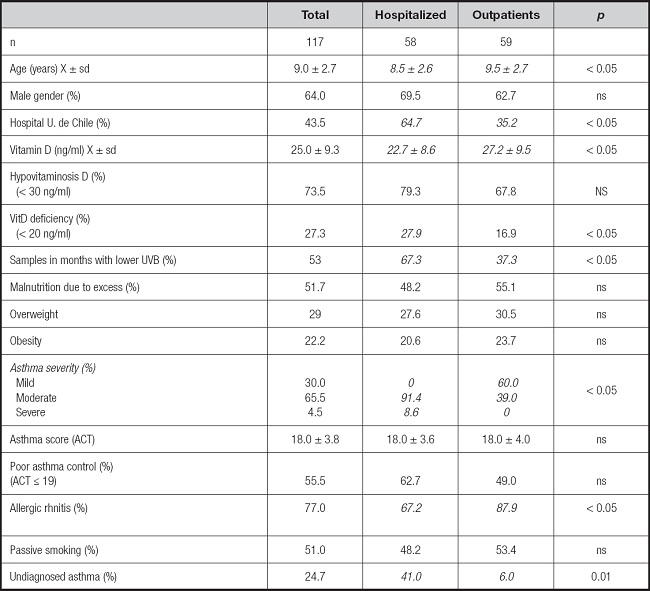
Table II. Serum concentration and percentage of deficit and hypovitaminosis D according to seasonality. Hypovitaminosis D < 30 ng/ml; deficiency < 20 ng/mL
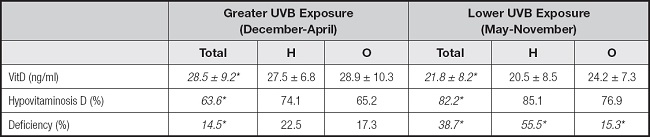
UVB: ultraviolet B radiation; H: hospitalized patients; O: outpatients.
*p < 0.05.
Table III. Distribution of nutritional status and VitD according to sex in schools with asthmatic children.
The characteristics of hospitalization can be seen in table IV. The average severity score achieved during hospitalization was 7 (moderate), with 48 % of the sample scoring severe. There were no differences in the mean concentration of vitD according to the severity score and according to each of its components (Fig. 1).
Table IV. Risk of hypovitaminosis D (< 30 ng/ml) and VitD deficit (< 20 ng/ml) in hospitalized asthmatic children.
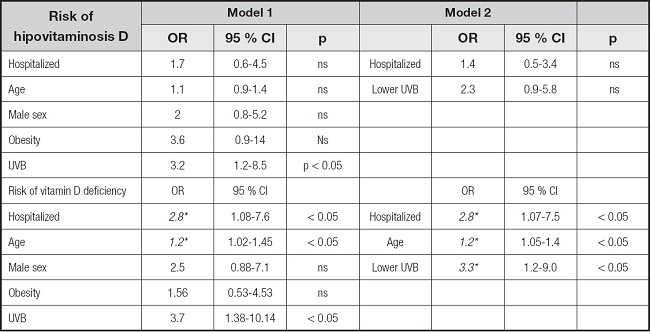
*p < 0.05. Hosmer-Lemeshow > 0.05 (appropriate goodness of fit).
OR: odds ratio; CI: confidence interval; UVB: ultraviolet B radiation.
The risk of hypovitaminosis and vitD deficiency in hospitalized asthmatic children was determined in comparison with those who were controlled and did not undergo hospitalization in the previous year through 2 logistic regression models (Table IV). In the first model, adjusted according to age, sex, presence of obesity and lower UVB; and in the second model, adjusted according to age and UVB (variables that were statistically significant). No risk of hypovitaminosis D was found in hospitalized children in either of the 2 models; however, the deficit of vitD was 2.8 times higher in patients who were hospitalized (OR, 2.8; 95 % CI, 1.08-7.6, p < 0.05) adjusted according to sex, obesity, UVB and age. In the second model, the risk of vitD deficiency is also higher in H subjects compared to A subjects (OR, 2.8; 95 % CI, 1.07-7.5, p < 0.05). The risk of vitD deficiency increases by 20 % for each year that the age of the subjects increases (OR, 1.2; 95 % CI, 1.02-1.45, p < 0.05).
In the second model, the odds of vitD deficiency persists, it being higher in H subjects compared to A subjects (OR, 2.8; 95 % CI, 1.07-7.5, p < 0.05). In both models, a lower UVB implies a 3.3 to 3.7 times greater risk of having vitD deficiency.
DISCUSSION
The main finding of our study was that hospitalized asthmatic subjects have a higher frequency of vitD deficiency, an association that disappears in the months of greater exposure to UVB radiation and increases in the months of less exposure. In inpatients the risk of having vitD deficiency is higher than that of outpatients, even after adjusting for seasonality and age. Few studies evaluate the frequency of deficiency and insufficiency of vitD in asthmatic patients who are hospitalized, and there are numerous studies that evaluate the concentration of vitD according to level of control, severity of asthma, and response to treatment. Bugadze, for example, found in a group of 50 Russian asthmatic schoolchildren a higher frequency of vitD deficiency in those with frequent and severe exacerbations compared to those with good control of the disease (p < 0.05) (17).
We found a high frequency of hypovitaminosis D (< 30 ng/ml) in the children studied (73.5 %). This result differs from that described in Costa Rica and Puerto Rico, where there is a much lower frequency than ours (28 % and 44 %, respectively), while the hypovitaminosis D rate found in Italian asthmatic children was 90.6 % (18,19). These differences could be explained by the different UVB exposures in these countries.
The high frequency of hypovitaminosis D found in our patients could be due to a low exposure to UVB light and/or a low intake of milk and fortified cereals, frequent conditions in the age group to which they belong (20,21). Numerous publications describe the relationship between vitD deficiency and increased risk of hospitalization for asthma. Brehm in Costa Rica finds that, as the concentration of vitD increases, a decrease in the risk of hospitalization is observed, after adjusting for age, sex, BMI-z and parental education (OR, 0.05; 95 % CI, 0.004-0.71; p = 0.03). This study also detected a decrease in the need for anti-inflammatory medication and bronchial hyperresponsiveness, variables that were not evaluated in our study (4). Other prospective cohort publications carried out in North American asthmatic children show that 35 % of them had hypovitaminosis D. After adjusting for age, sex, BMI, income, treatment received, and seasonality, it was observed that both deficit and insufficiency of vitD were associated with a higher risk of hospitalization or emergency service consultation (OR, 1.5; 95 % CI, 1.2-2.1; p = 0.004) (22).
In our study, the high prevalence of allergic rhinitis in H and A subjects stands out, a figure higher than that found in a study carried out in Japan (23) and in a multicenter study recently carried out in our country (24). Proper management of allergic rhinitis is very important, observing that this improves asthma control and exacerbations decrease (25).
Most of the asthmatic children in our study presented excess malnutrition, without differences between the group of hospitalized patients and that of outpatients, and without differences according to sex. We did not find any association between obesity and a higher frequency of hospitalization; however, it is described that excess malnutrition is a factor that may worsen the clinical management of asthma. Tashiro observed that obesity was associated with an increase in the incidence and prevalence of asthma, and that the more overweight, the more severity increased (26). This association could be due to the fact that asthmatic children with malnutrition due to excess have a lower response to corticosteroids, have a higher degree of airway inflammation, alteration of the intestinal and pulmonary microbiome and often vitD deficiency.
In our work, we did not find any association between nutritional status and vitD concentration. This could be explained by poor asthma control in these patients, which could be associated with a short time spent in outdoor activities, with the consequent low sunlight exposure.
In contrast to these results, in a study carried out in Costa Rica it was verified that as BMI increases, the average concentration of vitD decreases (5).
The average days of hospitalization and the concentration of O2 administered in our patients agrees with that described in the literature (27,8). Lastly, we found that serum VitD concentration was not associated with in-hospital evolution or with severity score in hospitalized subjects. In agreement with our findings, Iqbal found that in pediatric patients hospitalized for respiratory causes (66.7 % asthmatics) the concentration of vitD was not associated with severity of the disease (28). On the contrary, a study carried out in Concepción shows that vitD deficiency is frequent in children hospitalized in the Pediatric Critical Patient Unit (UPCP), and that this is associated with a greater probability of requiring mechanical ventilation, fluids and inotropic drugs (29).
Regarding the limitations of our work, it seems important to highlight that the power (72 %) to detect differences between the subjects with vitD deficiency was lower than expected. Furthermore, most of the hospitalized patients were recruited during the months of lower UVB exposure, which may have influenced the concentration of vitD. On the other hand, one of the centers participating in this study does not have a UPCP, which could have limited the admission of patients with greater severity. An element to be highlighted is that this study is the first in Chile to compare the serum concentration of vitD with associated factors in pediatric, hospitalized and outpatient asthmatic patients. Given the results obtained, it seems important to consider the systematic measurement of vitD in all asthmatic patients, especially in those who are hospitalized. We recommended the systematic supervision of intake and measurements of vitD blood levels before supplementing it. More clinical trials and cohort studies in asthmatic children are still needed to determine the optimal dose to be supplemented, the cut-off point to define the deficiency of vitD, as well as the clinical role it produces in asthmatic patients with hypovitaminosis when supplemented with this vitamin. On the other hand, it seems important to us to insist that asthmatic children perform physical activity outdoors to allow greater exposure to UVB light.
CONCLUSIONS
In all, 73.5 % of asthmatic children who are controlled in HCUCH and HRRio have vitD deficiency or insufficiency. VitD deficiency is 2.8 times higher in hospitalized patients than in outpatients. This risk increases with age and in the months with less UVB exposure. Clinical trials and cohort studies are needed to evaluate the optimal doses required by asthmatic children to achieve vitD concentrations and determine the clinical changes associated with vitamin supplementation.