INTRODUCTION
Dual-energy X-ray absorptiometry (DXA) is an accurate method for measuring total body and subregional bone mineral density (BMD), bone mineral content (BMC), fat mass (FM), and lean soft tissue (LST) (1-3). This method has the advantage of a short scan time (5-20 min) (4) and a low radiation dosage (± 10 μSv) (5). Moreover, it can be used with children and adolescents (6,7).
The three major commercial manufacturers of DXA are GE Medical Systems Inc. (formerly Lunar), Madison, WI, USA; Hologic Inc., Waltham, MA, USA; and Cooper-Surgical (formerly Norland Medical Systems, Inc.), Trumbull, CT, USA (8,9). One of the limitations of DXA is the size of the active scanning area. DXA machines have dimensions of approximately 60-67 cm in width and 193-198 cm in length (8,9).
The width of the scanning area can compromise the accuracy of the measurement when body dimensions exceed these limits. This is also true for people with a large trunk and skeletal muscle mass favorable for particular sports, such as bodybuilding, rowing, and rugby or obese patients (9), although currently new equipment can assess an area of 228 cm in length, 137 cm in width and a weight of 280 kg (7). However, these devices are not always available in laboratories, so in order to solve this methodological limitation, some researchers have studied the accuracy of half-body scans using DXA (HBS) for estimating the whole-body composition (10,11).
Indeed, some studies measured body composition by DXA in obese adults (4,12), obese children (7,13) and physically active young adults (11). Thus, analysis of the accuracy and homogeneity of half-body scans can improve the applicability of the technique in a clinical context (7), mainly when a person's body dimensions exceed these limits and even in patients with metallic implants in their extremities (14).
In general, to our knowledge, a study of this nature was not performed in the Chilean population, so this information could be relevant when evaluating heterogeneous adult populations.
Therefore, the aim of the study was, to verify the accuracy in body composition scanning through the half-body DXA scan compared to the standard total body scan, using GE Lunar Prodigy DXA
MATERIALS AND METHODS
SUBJECTS
A cross-sectional study was carried out on 145 volunteers (62 males and 83 females) between 18 and 70 years of age to compose the sample. Subjects fitting into the scanning area (197.5 x 66) of GE Lunar Prodigy were eligible to participate in the study. Those who did not complete the evaluations and those who presented some type of physical disability that prevented them from moving on their own were excluded. All volunteers were informed of the objective of the study and subsequently signed and authorized the informed consent form.
The data collection process was carried out in a laboratory of the Autonomous University between April and July 2019 from Monday to Friday from 8:30 am to 12:30 pm. The study was approved by the Research Ethics Committee of the local university.
INSTRUMENTATION
The anthropometric variables of weight and height were evaluated following the recommendations of Ross, Marfell-Jones (15). Body weight (kg) was assessed with a scale (SECA, Hamburg, Germany) accurate to 0.1 kg. Standing height was measured with a stadiometer (SECA, Hamburg, Germany) to the nearest 0.1 cm. BMI was calculated by means of the formula [BMI = weight (kg) / height (m)2].
Two DXA scans were performed the same day for analysis. First, WBS was performed and used as a reference. Second, HBS was performed to estimate the whole-body composition to compare it with the reference method. The same technician positioned the subjects, performed the three scans, and executed the analysis according to the operator's manual using the standard analysis protocol. Standardized positioning was maintained during HBS with volunteers in a supine position with the left sagittal line of scan window under the left upper limb. Right half-body composition was used to estimate the whole-body composition. Subjects were warned not to wear jewelry and to avoid and the presence of any type of metal on the body that could impede scanning.
DUAL ENERGY X-RAY ABSORPTIOMETRY (DXA)
DXA measurements were taken using a total-body scanner (Lunar Prodigy; GE Healthcare, Madison, WI, USA). The Lunar Prodigy DXA is an instrument with a weight limit of 160 kg and a relatively large space exploration of 197.5 x 66 cm. Scan analysis was performed using GE Encore 11.10 software (GE, Madison, WI, USA). The following variables were extracted from the DXA software: bone mineral content (BMC), fat mass (FM), Lean sof tissue (LST) and fat mass percentage %FM. The DXA was calibrated each day before measurement according to the manufacturer's guidelines. The coefficients of variation (CV) in our laboratory were 1.4 %, 1.6 %, and 1.0 % for BMC, FM, and LST, respectively.
STATISTICAL ANALYSIS
A descriptive analysis (mean ± standard deviation [SD], minimum and maximum), and the Kolmogorov-Smirnov test for normality were performed. We used Student's paired t-test to compare Pearson's correlation coefficient (r) to verify the relationship between the variables and linear regression analysis (adjusted coefficient of determination [R2]. Additionally, the standard error of estimate [SEE]) was used to verify explanation power of HBS in estimating the whole-body composition with WBC. The concordance correlation coefficient (CCC) proposed by Lawrence, Lin (16) was also calculated to verify precision and accuracy. The significance level was set at α ≤ 0.05. The SPSS version 16.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis, as wellas MedCalc 11.1.0.
Results
The anthropometric variables characterizing the sample studied can be seen in table I. There were no significant differences in age (p = 0.23) and BMI (p = 0.74) between both sexes. However, as expected, men presented higher weight and height in relation to women p < 0.000).
Table I. Characteristics of the sample studied.
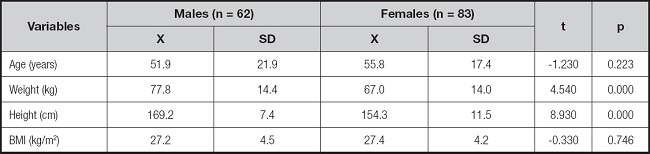
X: mean; SD: standard deviation; BMI: body mass index.
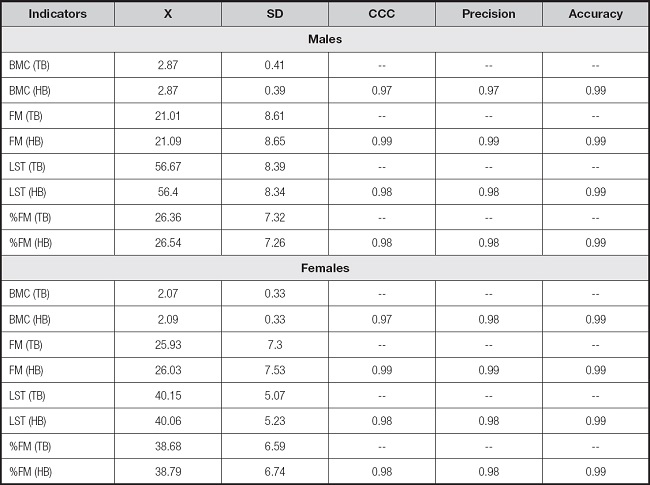
Comparisons of BMC, FM, LST and %FM values between total body and half body by sex are shown in table II. There were no significant differences between both scans (p = 0.81 to 0.99) in both men and women.
Table II. Comparison of total-body and half-body composition indicators in both sexes.
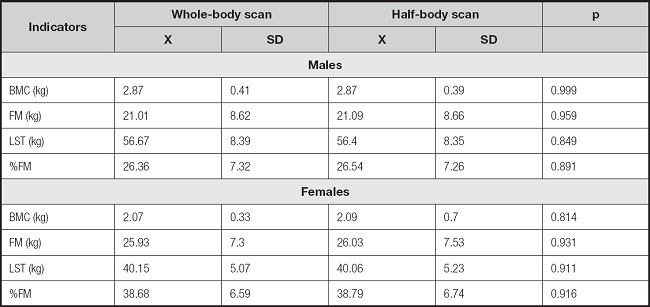
X: mean; SD: standard deviation; BMC: bone mineral content; FM: fat mass; LST: lean soft tissue; %FM: percentage of fat mass.
The correlations between both scans according to body composition indicators are shown in figure 1. In men and in the four indicators (BMC, FM, LST and %FM) the predictive power ranged from R2 = 0.94 to 0.98. For women the values explained from R2= 0.96 to 0.98, respectively.
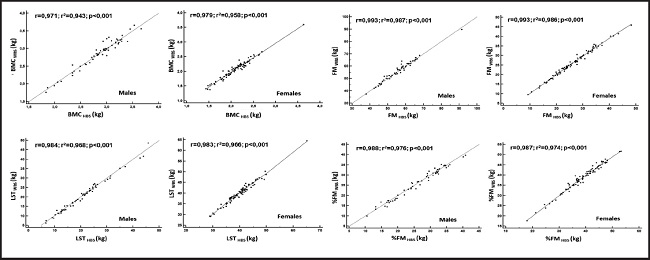
Figure 1. Relationship between both scans (total body and half body) according to body composition indicators in both sexes.
The DRI values that define the degree of agreement between both scans are shown in table III. In general, it is observed that the half-body scan shows a CCC with the reference method (total body) from 0.97 to 0.99. In addition, the values of precision (0.97 to 0.99) and accuracy (0.99) in both sexes are high.
Discussion
The aim of the study was to verify the accuracy of body composition scanning through HBS DXA scanning compared to standard WBS scanning, using GE Lunar Prodigy DXA.
The results of the study have shown that the half-body scan reflects similar results as the total body scan in the indicators of BMC, FM, LST and %FM. These findings are consistent with some studies that compared both methods (4,7,10,12).
In fact, no bias was observed in the results, even the correlations between both methods were high and almost perfect, ranging from 0.93 to 0.99 as reported by other studies (7,17).
Evidently, HBS scanning has reflected wide concordance and precise and accurate values versus WBS scanning, as this information allows highlighting that the HBS scanning technique supports the use of DXA to scan a larger number of subjects and in less time. It also allows the inclusion of those sub- jects that are outside the scanning area (7) due to their extreme body dimensions (9).
In fact, DXA has become a popular tool for measuring body composition due to its ease of operation, completeness of analysis and gold standard (18,19). For nowadays WBS and HBS scanning, can be considered as precise and accurate scanning techniques, moreover, some studies have used HBS scanning to predict body composition in weight reduction programs in obese patients who barely fit in the scanning area (20) and even, to verify body composition changes after bariatric surgery in morbidly obese individuals (21).
In that sense, it is important that studies develop a satisfactory technique to scan individuals of all physical types (11), these include patients who present metallic implants in their extremities, as they are often excluded from studies covering body composition analysis (15).
Also, it is widely known that most manufacturers' manuals do not verify the use of DXA for body composition analysis in subjects with a metallic implant (22).
Consequently, having the HBS scanning technique in clinical and epidemiological contexts may avoid excluding some patients who are likely to have extreme physical characteristics, as well as amputations and/or metallic implants in some of their extremities. On the contrary, HBS scanning opens new perspectives and possibilities to be implemented in clinics and laboratories to cover not only conventional but also non-conventional populations.
In general, DXA is a non-invasive, fast, safe and low radiation method equivalent to a day sunbathing (23), in addition, in recent years, DXA equipment have been improving over time in their designs and manufacturing models, for example, they have been reducing scanning times, as well as have ostensibly improved the quality in their images in terms of pixels (24).
This research presents some strengths, given that it is the first study that verified the applicability of the use of HBS scanning in a sample of Chilean adults. In addition, the results obtained in this study can serve for future comparisons, as well as a baseline to verify trends among the adults studied.
Notwithstanding the above, the study has some limitations, for example, the type of sample selection and the number of participants considered were not large enough. These aspects could limit the generalizability of the results to other contexts, so they should be analyzed with caution. Future studies should consider the use of more sophisticated equipment to corroborate our findings.
In conclusion, this study demonstrated that HBS scanning through DXA evidenced concordance and high values of precision and accuracy to assess body composition indicators (BMC, FM, LST and %FM.) in adult patients. The results suggest the use and application in research, clinical and epidemiological contexts.