INTRODUCTION
Home parenteral nutrition (HPN) should be administered to patients unable to meet their nutritional requirements via oral and/or enteral route, and who can be safely managed outside of the hospital. HPN is the primary and life-saving therapy for chronic intestinal failure (CIF).
In Europe, the prevalence of HPN due to benign CIF has been estimated to range from 5 to 20 cases per million population (1). In Spain, according to the most recent voluntary registry of the Working Group on Home and Outpatient Artificial Nutrition of the Spanish Society for Clinical Nutrition and Metabolism (NADYA-SENPE), the prevalence of HPN in both adults and children has been increasing over the last few years reaching 6.01 patients per million in the year 2019 (2).
According to the ESPEN guidelines, monitoring HPN patients should be carried out by an expert multidisciplinary nutrition support team, home care specialists as well as by a home care agency with experience in HPN and should also involve the general practitioner (1).
Home care aims at satisfying people's health and social needs while in their home by providing appropriate and high-quality home-based health care and social services. It may involve formal and informal caregivers and use technology when appropriate, within a balanced and affordable continuum of care (3).
In Europe, countries such as Belgium, France, Italy, Portugal, United Kingdom, and Spain have an organizational model in which the “health” component of home care is part of the health care system, and the “social” component is part of the social system (3). Offering homecare helps avoid hospital admissions, allows early discharge to free up hospital beds, increases patient choice, and helps reduce waiting times (4). All these aspects are especially important during the current COVID-19 pandemic.
Nutrihome© is a homecare programme developed for patients with HPN (5). It is a programme unique in Spain, since here, unlike other European countries, there are no global homecare companies that provide home nutritional care for this type of patients. Its main objective is to facilitate the patient's transition from hospital to home, optimise patient training, and follow-up patients on their HPN treatment.
The objective of this study was to describe the results of the implementation of an HPN care programme (Nutrihome©) in a cohort of patients treated at a tertiary hospital.
METHODS
Retrospective study of the patients included in Nutrihome© at Hospital General Universitario Gregorio Marañón (HGUGM), Madrid, Spain. Prior to Nutrihome© implementation a series of scoping meetings were held. The meetings included a variety of healthcare professionals involved in HPN management at the hospital like physicians, nurses, and pharmacists, and also other professionals (members of the industry, statisticians, etc.). The overarching aim of the meetings was to brainstorms ideas to develop a ground-breaking HPN care programme.
Additionally, to have a better understanding of the type of patients treated at our hospital, a complete clinical and economic evaluation was conducted. The results were published in two different articles (6,7). The direct healthcare and non-healthcare costs accounted for 96.46 % of the overall costs, the personal costs for the patients receiving HPN amounted to 2.62 % and productivity costs to 0.92 % (6). Furthermore, the studies offered a helpful diagram showing all the categories of HPN costs based on the activity conducted at the hospital, which could be used in the designing of cost studies of other HPN programmes.
Based on the type of costs included in the first study, a cost simulator was developed. This is a useful tool designed to rapidly calculate the costs of HPN in a particular setting. The reason behind this is to obtain the direct costs of HPN without having to conduct an extensive cost analysis that is time consuming and requires numerous research personnel.
The implementation of Nutrihome© at HGUGM was performed in 2 phases: Nutrihome© pilot and Nutrihome© programme, which ran from 2017-2018 through December 2019-May 2021, respectively. The immediate results of the pilot prompted the team to develop a series of modifications in the activities initially thought to be part of Nutrihome©. This led activities such as home visits or patient training to suffer some type of adaptations before Nutrihome© programme started.
Nutrihome© consists of different modules. The transition module covers the first 30 days of HPN including: pre-discharge nursing hospital visits and nursing home visits, deliveries of the infusion pump, consumables and HPN bags, patient training (including a complete evaluation of competency level of the patients and/or their caretakers), weekly scheduled nursing home visits, scheduled nursing phone calls, stock control phone calls, and 24-hour on-call line manned by the nurses (5).
Module 1 starts on day 31 and module 2 on day 90, and both include the same activities as the transition module, with the exception of the scheduled nursing home visits, which are weekly in Module 1 and monthly in Module 2. Module 3 is recommended starting month 7 and includes the delivery service, and the 24-hour on-call line. However, in exceptional cases, some of the patients can skip Module 1 and go directly to Module 2 if their clinical status and type of follow-up they require allow it (5).
Both during the pilot and the programme, the homecare nurses conducted a complete evaluation of the patients' prior to discharge. The data gathered included vital signs, nutritional status and bowel habit, oral diet, sleep, socio-economic status, and drugs, among others. On top of that, the suitability of the home care environment was also assessed and approved before starting HPN.
Since the beginning, Nutrihome© worked in close collaboration with the hospital staff both from the Nutrition Unit and the Pharmacy Service keeping constant communication with the coordinators. Table I details the process involved in the implementation of Nutrihome© at the Hospital General Universitario Gregorio Marañón.
Table I. Steps in the implementation of Nutrihome© at Hospital General Universitario Gregorio Marañón.
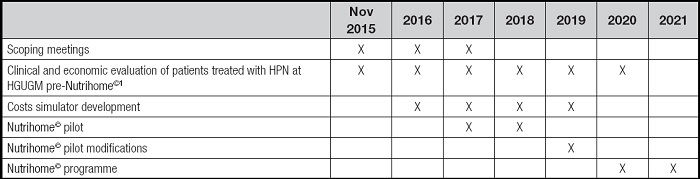
1The results have already been published by our group (6,7).
HPN: home parenteral nutrition; HGUGM: Hospital General Universitario Gregorio Marañón.
COST ANALYSIS
The direct costs associated with the management of patients' complications were calculated. The total costs were obtained by multiplying the number of emergency room days, the number of days of hospitalization, and the number of catheter replacements by the unit cost.
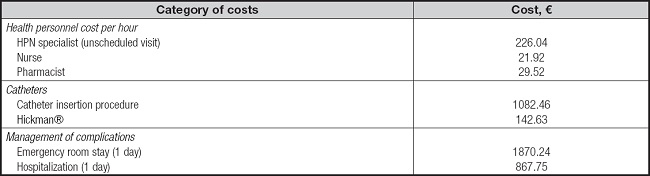
Additionally, an estimate of the costs saved through the adverse events reported by Nutrihome© was also conducted. The estimates were done on the assumption that these adverse events (clinical, technical, catheter-related, and other) would need to be solved by different healthcare professionals (HPN specialist through unscheduled visits, nurse and/or pharmacist, respectively) if these patients were not included in Nutrihome©. A total of 30 min was estimated for each healthcare professional to solve these adverse events. Afterwards, the cost per patient and cost per patient per day was estimated. The unit costs were taken from the study conducted by Arhip et al. (6) and updated to Euros (€) for the year 2022 using the CCEMG-EPPI-Centre Cost Converter (v.1.6 last update: 29 April 2019) (8) (Table II). All costs are expressed in Euros (€) for the year 2022.
QUALITY OF LIFE AND PATIENTS' SATISFACTION
Data on quality of life were recorded using the EQ5D-3L© and EQ5D-5L© instrument for the patients included in the Nutrihome© pilot and programme, respectively and the HPN-QOL©9, which is a self-assessment tool for the measurement of quality of life in patients on HPN. According to the scoring procedure, the HPN-QOL© is built with both multi-item scales and single-item measures. These include 8 functional scales, 9 symptom scales, 3 global health status/quality of life scales and 2 single items. As it is customary with quality-of-life instruments, all scales are linearly transformed to scores between 0 and 100. Regarding the functional and health status/quality of life scales and the two HPN items, a high score indicates high functional or good health status. Regarding the symptom scales/items a high score represents a high (“bad”) level of symptoms (10).
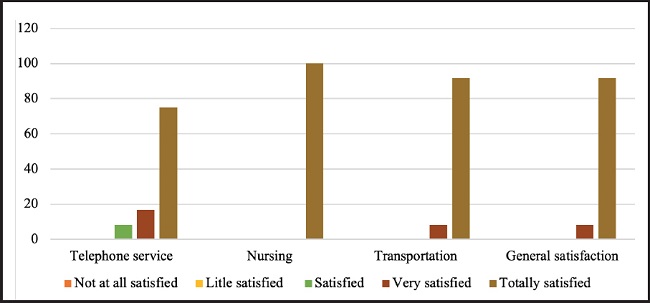
Patients' satisfaction was recorded using a questionnaire including 4 items regarding the telephone service, nurses, transportation, and global evaluation and 5 answers: not at all satisfied, little satisfied, satisfied, very satisfied, and totally satisfied.
DATA COLLECTION
The variables were collected from medical records, the dispensary, and the Nutrihome© database. Data collection was compliant with the Law on Protection of Personal Data (Spanish Organic Law 15/1999). All patients gave their informed consent. Data are expressed as median and interquartile range and frequencies. The programmes used were Microsoft Excel (Microsoft Office 365 ProPlus), and IBM SPSS Statistics 23.
RESULTS
STUDY POPULATION AND CLINICAL VARIABLES
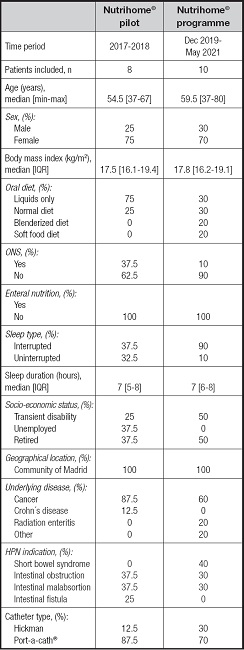
The study included 8 (75 % women) and 10 (70 % women) patients in the Nutrihome© pilot and Nutrihome© programme, respectively. Table III shows the characteristics of the study population in both phases of its implementation.
NUTRIHOME© PILOT
The median duration was 31.5 days [14-68.5]. Nutrihome© pilot included new HPN patients and relapsed patients in rates of 87.5 % and 12.5 %, respectively. All the patients included were hospitalised when HPN was initiated.
All the patients started the 30 days transition module and continued to Module 1. The module categories and the differences between them was later developed for the Nutrihome© programme.
The median number of HPN bags per week was 7 [7-7]. A total of 100 % of the patients used custom-made HPN bags. Nutrition infusion was 16 hours [14-18], 100 % of the patients had a night-time cycle. The median HPN volume was 1500 mL [1425-1950], and 50 % of HPN were supplemental.
The median visit service time (time spent at the patients' home for conducting the initial nursing visit) was 105 min [93.7-120].
Nutrihome© pilot registered a total of 78 home nursing visits, 96 scheduled nursing phone calls, 33 stock control phone calls, 20 patient phone calls, 328 HPN bags, and 142 deliveries.
Additionally, 37 adverse events were reported, 26 of which were technical, 9 were clinical, 1 was catheter-related and 1 was a different event. A total of 99 % of these events were solved by Nutrihome, phone calls or home visits with the exception of catheter-related bloodstream infections (CRBSIs), which required hospitalization.
Nutrihome pilot also included psychologist home visits and phone calls (chosen by 50 % of the patients).
NUTRIHOME© PROGRAMME
The median duration was 140 days [47.2-355.5]. The patients included were mostly new HPN patients (80 %). Compared to the pilot programme, only 60 % of the patients included in the programme were hospitalised. The remaining ones were able to start HPN at home.
Since the start of the COVID-19 pandemic, 7 patients were started on HPN and included in Nutrihome© programme while 3 of them started HPN directly at home without ever being hospitalised. In particular one of the patients started on HPN at home during the complete lockdown (March 2020).
After the 30 days transition module, 60 % of the patients continued to Module 1 whereas 40 % continued to Module 2. The patients spent 160 days [25-230.5] in Module 1 and 110 days [21-314.2] in Module 2, respectively. Three patients moved from Module 1 to Module 2 later on.
The median number of HPN bags per week was 5 [4-7]. Custom-made HPN bags were used by 90 % of the patients. Nutrition infusion time was 12 hours [12-13.5], 90 % of the patients havd a nigh-time cycle. The median HPN volume was 1100 mL [1000-1500]. All HPN were supplements.
The median visit service time was 90 min [67.5-120].
Nutrihome programme registered a total of 176 home nursing visits, 209 (includes year 2020 only) scheduled nursing phone calls, 96 stock control phone calls, 61 (includes year 2020 only) patient phone calls, 1368 HPN bags, and 608 consumable deliveries.
A total of 107 adverse events were reported, 57 of which were technical, 21 clinical, 16 catheter-related and 13 were other events. A total of 99 % of these events were solved by Nutrihome, phone calls or home visit with the exception of CRBSIs.
PATIENT TRAINING
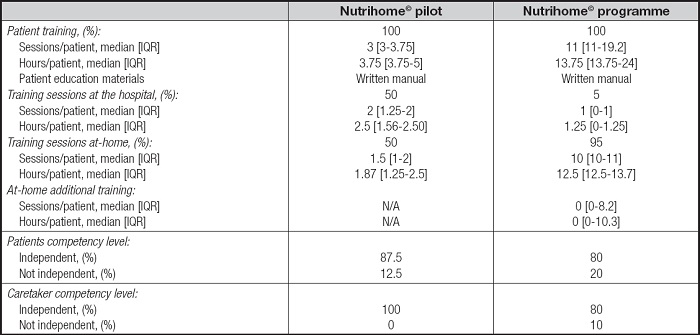
During the Nutrihome© pilot, most patient training was conducted at the hospital, before discharge. However, this was one of the changes made later in the Nutrihome© programme where patient training was conducted almost exclusively at home.
Patient training included in the pilot and the programme was always in addition to the usual training given by the hospital's healthcare personnel. What is more, Nutrihome© programme included extra training sessions, which were required by 3 patients. Most patients and/or their caregivers reached the level of independence needed for HPN management. The Nutrihome© team together with the hospital healthcare personnel in charge of these patients developed a patient training manual that was used in both phases. The patients and their caregivers were trained on catheter care, pump use, preventing, recognizing, and managing complications and so on (Table IV).
HOSPITALIZATIONS, EMERGENCY ROOM VISITS, AND RATE OF INFECTION
The patients included in the pilot and the programme went to the emergency room 1 single time, respectively. Each of those visits were due to CRBSIs and resulted in 2 hospitalizations. This led Nutrihome© pilot to present an infection rate per 1000 catheter days of 2.35 while the Nutrihome programme had an infection rate of 0.52 per 1000 catheter days. Three of the patients included in the Nutrihome© programme used taurolidine lock.
COST ANALYSIS
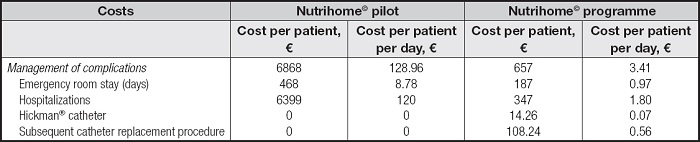
The direct costs associated with the management of complications were €6867 per patient (€128.96 per patient per day) and €657 per patient (€3.41 per patient per day) in the Nutrihome© pilot and programme, respectively (Table V). The patients were hospitalized for 63 days.
During the pilot programme, the costs saved through the adverse events reported by Nutrihome© were €160.41 per patient (€3.01 per patient per day) divided into the following categories: technical [€44.65 per patient (€0.83 per patient per day)], clinical [€113 per patient (€2.12 per patient per day)], catheter-related [€1.37 per patient (€0.02 per patient per day)], and other [€1.37 per patient (€0.02 per patient per day)].
During the programme, the costs saved through the adverse events intercepted by Nutrihome© were €331.70 per patient (€1.72 per patient per day) divided into the following categories: technical [€73.87 per patient (€0.38 per patient per day)], clinical [€226 per patient (€1.17 per patient per day)], catheter-related [€17.53 per patient (€0.09 per patient per day)], and other [€14.24 per patient (€0.07 per patient per day)].
QUALITY OF LIFE AND PATIENTS' SATISFACTION
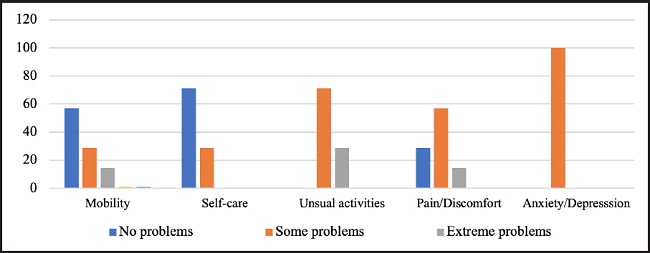
Nutrihome© pilot patients' quality of life was 50 [30-60] according to the visual analogue scale (VAS). The main problems of the 3 dimensions, from most to least significant, were anxiety/depression (100 %), usual activities (100 %), pain/discomfort (71.4 %), mobility (42.9 %), self-care (28.6 %). Figure 1 shows the EQ-5D-3L descriptive system.
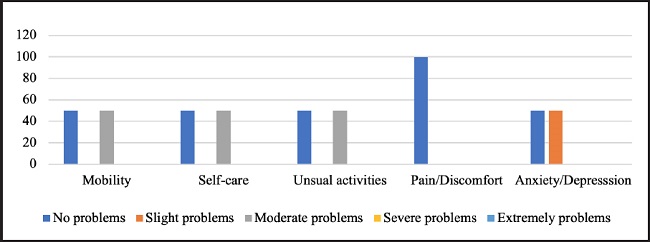
Nutrihome© programme patients' quality of life was 72.5 [70-.] according to the visual analogue scale (VAS). The main problems of the 5 dimensions, from most to least significant, were anxiety/depression (50 %), usual activities (50 %), mobility (50 %), self-care (50 %), pain/discomfort (0 %). Figure 2 shows the EQ-5D-5L descriptive system. Additionally, table VI shows the data obtained using the HPN-QoL© questionnaire.
Table VI. Patients' quality of life according to HPN-QoL© questionnaire.
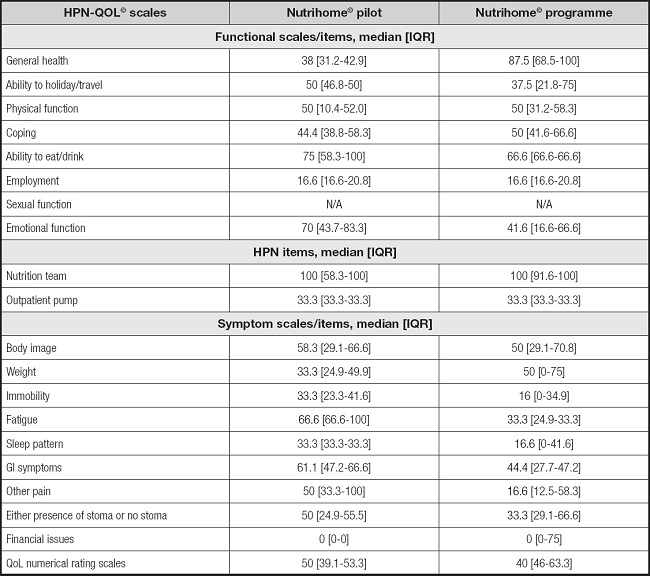
IQR: interquartile range; N/A: not available
Regarding patient's satisfaction, we collected data from 12 patients (5 patients from the pilot and 7 from the programme). A total of 91.7 % of the patients were totally satisfied with either the Nutrihome© pilot or the programme (Fig. 3).
PATIENT OUTCOMES
Out of all the patients included in the Nutrihome© pilot, 87.5 % died and 12.5 % were weaned off. Whereas, of those included in the programme, 80 % are still included, 10 % of the patients have been weaned off and 10 % have already died. None of the patients died due to HPN related complications.
DISCUSSION
The objective of this study was to describe the results of the implementation of Nutrihome© in a cohort of patients treated with HPN at a tertiary hospital. Compared to the previous activity at our hospital, the implementation of Nutrihome© brought some changes into how HPN patients are currently managed (Table VII).
Table VII. Differences between HPN with and without Nutrihome© at Hospital General Universitario Gregorio Marañón.
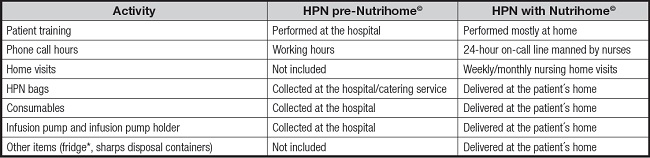
*Only included in Nutrihome© pilot.
The activity performed during Nutrihome© implementation followed the ESPEN guideline on HPN, which recommends, with a grade of Recommendation GPP, strong consensus (91.3 % agreement) that home care environment should be assessed and approved by the HPN nursing team before starting HPN, wherever possible.
The implementation of Nutrihome© programme has led to an increased and intense level of training of patients with HPN at our hospital. Most of this training was performed at the patient's home which follows the ESPEN guidelines on HPN.
Different publications regarding the management of patients at a national UK intestinal failure unit demonstrated that patients can be educated at home, which reduces the length of stay and may be preferable for some patients (11-13).
According to the study conducted by Arhip et al. at our hospital, the infection rate pre- Nutrihome© was 2.03 per 1000 catheter days, similar to the rate of 2.35 per 1000 catheter days obtained in Nutrihome© pilot. Conversely, after the implementation of the Nutrihome© programme the infection rate dropped down to 0.52 per 1000 catheter days. This data being lower than that published in the literature (14). This infection rate can be explained by the consistent patient training, the number of sessions and hours per patient and the stable environment, most of the training being performed at the patient's home. These data support the involvement of home care nurses that adhere to a strict predefined catheter care protocol. It is worth noting that the infection episode presented by the patient included in the Nutrihome© programme appeared during a temporary leave from the programme during the holidays, which led the patient care to be managed by third parties. This makes necessary to raise awareness on HPN patients and their care in all settings.
The cost analysis showed that the management of patients included in both the Nutrihome© pilot and programme, respectively (€14.9 per patient per day and €0.26 per patient per day) is lower compared to the data obtained in the cost analysis of patients managed at our hospital without Nutrihome© (€27.10 per patient per day) (6). This can be explained by the lower infection rate that led to less emergency room visits and hospitalizations.
Regarding quality of life and the degree of satisfaction of the patients included in Nutrihome©, data should be interpreted in the light and context of the recent hospitalization, the data being collected days after discharge. Given the number of patients and the limited time they spent in Nutrihome©, the study of the data on quality of life was cross-sectionally analysed and only reflects the image of the recent discharge.
CONCLUSIONS
The implementation of Nutrihome© first as a pilot was key to improve the programme in terms of patient training, catheter care and follow-up. Nutrihome© programme has been extremely useful during this pandemic facilitating both the start of HPN and training at the patient home without the need of hospitalisation. Additionally, the adverse events reported and solved by Nutrihome© not only reduced the physicians' burden during those tough times and the patients' stress of being hospitalised during a pandemic but supported the entire healthcare system.