INTRODUCTION
Overweight and obesity in childhood, puberty and adolescence have become a public health problem, significantly affecting the poorest sectors of society. In the last 40 years, it has increased from 11 to 124 million worldwide (1,2) for the same age group. In Bolivia, the prevalence of overweight and obesity in children under five years of age and schoolchildren aged 12 to 16 years ranges between 10 % and 27 %, respectively (3). Body mass index (BMI) (4) is the most widely used indicator to diagnose overweight and obesity; however, it does not assess the distribution of body fat (5,6), an aspect strongly associated with the risk of chronic non-communicable diseases (7).
Waist circumference has a significant association with visceral fat and cardiometabolic risk (8,9). However, its measurement has considerable variability in obese subjects (10), and it requires removing part of the clothing and, according to gender, different space measurements.
It would be beneficial to have a more specific, more reliable and less complicated measuring parameter, such as neck circumference (NC), to assess the impact of interventions treating and preventing overweight and obesity.
NC was studied for the first time in the pediatric population in 2010. Since then, several countries have proposed it as a tool to identify overweight, obesity, and metabolic syndrome (11-15).
It is a parameter with good inter and intraobserver reliability (16). In addition, it is significantly correlated with waist circumference and BMI and has high sensitivity and specificity to identify overweight and obesity in childhood and adolescence.
Despite the advantages mentioned, it is not yet used in clinical practice because of the lack of internationally recognized cut-off points for the pediatric age.
The objective of this study was to explore the diagnostic validity of NC to detect overweight and obesity in a sample of schoolchildren between 10-12 years of age in the city of El Alto, Bolivia, at an altitude of 4,150 meters.
MATERIAL AND METHODS
A cross-sectional and analytical study was carried out between September 2016 and June 2017 in El Alto (La Paz, Bolivia), located at 4,150 meters above sea level. The target population was 17,319 students from fifth to seventh grade of public, private and mixed schools (17). The study started after the approval of the National Bioethics Committee and prior to taking body measures, we obtained an informed parental consent. A randomized sample size selected 399 subjects. It was calculated for a confidence level of 95 %, a type I error of 5 % and a power of 80 % for diagnostic test designs, with a sensitivity and specificity of 50 % given the absence of data in Bolivia. We excluded subjects with malformations which made the measurements difficult. We used BMI-z for age to identify overweight or obese subjects, calculated using the WHO Anthro Plus (4) software. The cut-off points proposed by the WHO ≤ -2 were classified as “low weight”; between -2 and +1 as “eutrophic”; between BMI-z ≥ +1 and < +2 as overweight; and BMI-z ≥ 2 as obesity. BMI was considered as the gold standard to validate neck circumference (4).
Two previously standardized researchers performed all the anthropometric measurements. An accuracy of 99 % was obtained in the standardization, as well as an average difference with the standard of 0.18 and 0.38, with an error of less than 1 % accuracy. Height and weight were assessed with a stadiometer and a previously calibrated electronic anthropometric scale (SECA 813® 0.1 kg).
The neck circumference was measured with an inextensible tape (SECA 20® 0.1 cm), below the laryngeal prominence and perpendicular to the long axis of the neck, in a standing position and with the head in the horizontal Frankfurt plane parallel to the floor (18). Waist circumference was measured standing and at the end of normal expiration, using the same tape, between the upper border of the iliac crest and the last rib, using a tape measure at just above the uppermost lateral border of the right ilium, at the end of a normal expiration. It was recorded at the nearest millimeter, as described by the National Center of Health Statistics (19).
The data was tabulated in Excel, and the statistical analysis was carried out in the STATA program version 13. Overweight and obese schoolchildren were grouped into a single category, “malnutrition by excess”. The normality of the data was evaluated through the Kolmogorov-Smirnov test. Means and standard deviations or median and interquartile range were calculated according to the distribution of the variable. To detect significant differences between the variables, Student’s t-test, ANOVA, Kruskal-Wallis or Wilcoxon tests were used according to the normality of the data. In addition, comparisons were made by sex and by age groups. Spearman’s correlation analysis was performed between neck and waist circumference and BMI-z. Neck circumference cut-off points were determined using ROC curves by age group and gender, and sensitivity, specificity, and positive and negative likelihood ratios were calculated. The cut-off points for the likelihood ratio considered were as follows: for the positive, > 10 as highly relevant and 5 to 10 as good; and for the negative, < 0.1 as highly relevant and 0.1 to 0.2 as good.
RESULTS
We studied 371 schoolchildren between 10 and 12 years of age. Eight children with undernutrition and 20 outside the age range were excluded. Table I shows that more than a third of schoolchildren had malnutrition by excess (24 % overweight and 10 % obesity).
Table I. Characteristics of sample in Bolivian schoolchildren aged 10-12 years (n = 371).
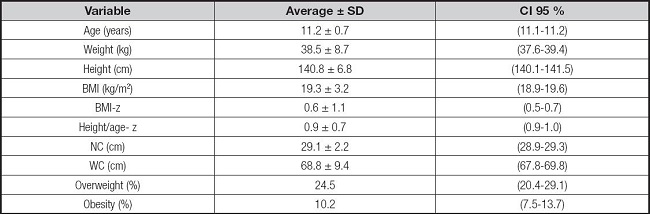
SD: standard deviation; CI: confidence interval; NC: neck circumference; WC: waist circimference; BMI-z: body mass index z; BMI-z ≥ 2: overweight; BMI-z ≥ 3: obesity.
Neck circumference increased with age and was higher in boys. In contrast, girls had higher height, weight, and BMI in all age groups (Table II).
Table II. Characteristics of the sample in Bolivian children aged 10-12 years in both genders.
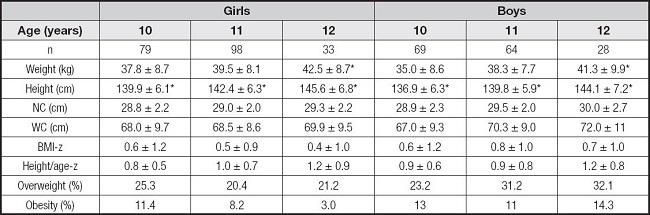
*ANOVA (Bonferroni) < p 0.05.
NC: neck circumference; WC: waist circimference; BMI-z: body mass index z; BMI-z ≥ +1 to < +2: overweight; BMI-z ≥ 2: obesity.
Overweight and obese boys and girls had a greater perimeter than their eutrophic peers (31.1 ± 1.8 cm vs 27.9 ± 1.3 cm, respectively; p < 0.0001) (Table III).
Table III. Neck circumference in Bolivian schoolchildren according to gender, age and nutritional status.
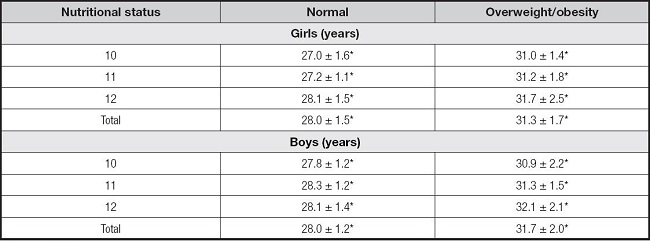
*t-test p < 0.0001.
The correlation analysis shows that NC has a high and significant correlation with waist circumference and the BMI-z in subjects of both sexes (r > 0.8; p < 0.001); furthermore, the correlation of the BMI-z with NC is similar to BMI-z with waist circumference (Table IV).
Table IV. Association of neck circumference, waist circumference and BMI-z (Spearman’s correlation) in Bolivian children aged 10-12 years in both genders.
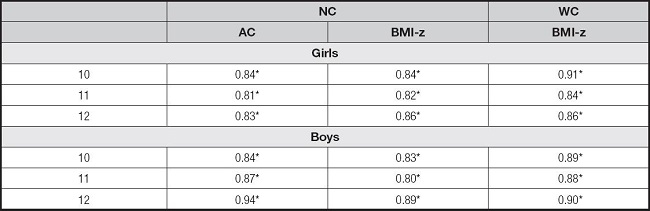
*p < 0.001. NC: neck circumference; WC: waist circimference; BMI-z: body mass index z.
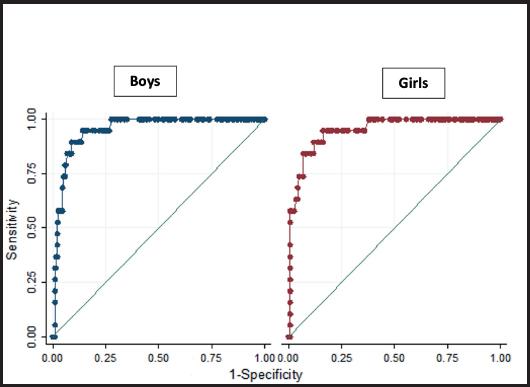
The sensitivity and specificity of the NC to diagnose overweight malnutrition ranged from 84.6 % to 92.3 % and 86.4 % to 92.0 %, respectively. In all age and sex groups, the area under the curve was greater than 0.90, and the positive likelihood ratio was > 5 (Table V).
Table V. Usefulness of neck circumference for the diagnosis of overweight and obesity in Bolivian schoolchildren aged 10-12 years in both genders.
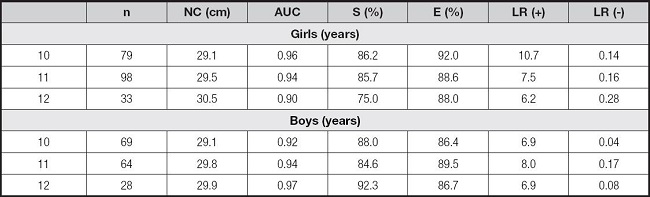
NC: neck circumference (cut points); AUC: area under the curve; S: sensitivity, E: specificity LR likelihood ratio positive (+) and negative (-).
Table VI shows the direct association between the probability of being obese and the NC value through a logistic regression model; this association is independent of the age and sex of the subject.
Table VI. Association of neck circumference with obesity in a logistic regression model.

Model I: without adjustment.
Model II: adjusted by age and sex.
*Significant values p < 0.01.
BMI: body mass index; CI: confidence interval; OR: odds ratio.
Finally, the area values under the ROC curve show a high discriminative capacity of the NC cut-off points to separate schoolchildren with and without excess malnutrition at all ages (Fig. 1).
DISCUSSION
This study supports the validity of NC for the identification of overweight and obesity in schoolchildren aged 10-12 years of both sexes who live at high altitudes.
The prevalence of malnutrition due to excess in our study is similar to UNICEF’s in 2020, which indicated that 22 % of the school population in Bolivia was overweight and 11 % was obese (20).
Similar to other studies, we found a positive correlation (≥ 0.60) between NC, BMI and WC (21,22). A cross-sectional study conducted in India in 360 subjects (13-16 years old) found a good and significant (< 0.001) correlation between NC and WC in both men (0.72) and women (0.67) (14). Another Mexican study, which included schoolchildren aged 6-11 years of both sexes with normal weight, detected a correlation between NC and BMI (between 0.51 and 0.67) and waist circumference (between 0.59 and 0.72) (17).
In the present study, NC values for obese children ranged between 30.9 and 31.7 cm. For subjects of the same age, the study by Kym et al. presented values between 30.5 and 32.5 cm (21), and Valencia Sosa et al., between 28.5 and 30.3 cm (n = 1,800) (17). Kelishadi et al. reported a higher average NC in overweight and obese schoolchildren compared to eutrophic counterparts (n = 23,000) (23).
Our study’s sensitivity (84.6-92.3 %) and specificity (86.4-92.0 %) values using NC to diagnose malnutrition due to excess were high and comparable to other studies, like that of Taheri M. et al., with a sensitivity of 75-83 and specificity of 71-85 using NC in schoolchildren to diagnose malnutrition due to excess (16). The lowest sensitivity value in our study was in 12-year-old girls, probably due to the low prevalence of obesity at that age in our study (3 %). The best sensitivity and specificity values in the different groups were obtained with NC cut-off points between 29 cm and 29.9 cm. When comparing our results with those of Castro Piñero J et al., we observed that our NC cut-off points were lower (24).
Iñarritu-Pérez M et al., with NC cut-offs of 30.0 and 29.3 cm for 12-year-olds, 31.9 and 30.4 cm for 13-year-olds, and 33.5 and 30.7 cm for 14-year-old in male and female Mexican adolescents, respectively, have the highest sensitivity and specificity. The NC cut-offs identified overweight/obesity in 80 % of males and 86 % of females, and indicated significant correlations (p < 0.01) in males and females with weight (r = 0.821 and r = 0.840, respectively), BMI (r = 0.649 and r = 0.819, respectively), WC (r = 0.710 and r = 0.813, respectively) and mid-upper arm circumference (r = 0.736 and r = 0.815, respectively) (25).
Our results should be analyzed considering the altitude at which the study was carried out. Different investigations show that body composition can be modified by the altitude at which the subjects live. Lowland and highland children differ in their patterns of stunting, BMI, WC and WCH index (26). Santos C et al. observed that schoolchildren who lived at higher altitudes had a lower prevalence of obesity than those who lived at sea level (6.3 % vs 41 %, respectively). Tibetan children living permanently above 4,000 m show a phenotypic adaptation in chest growth and a moderate reduction in linear growth. The differences could be explained by the environment, stress exposure to cold climate, and hypoxia, discarding the influence of food patterns and economic conditions. Although we did not find studies of NC done at high altitudes, the data above suggest considering altitude as a variable to consider when defining references (27).
Our study has certain limitations that must be considered when interpreting the results. As we diagnose overweight and obesity through the BMI, we cannot distinguish between the percentage of lean mass and body fat mass. Another aspect to consider is the small sample size in some of our groups.
In summary, we found that NC identified correctly a large proportion of overweight and obese schoolchildren. NC measurement is a simple technique that does not require undressing the individual, has good inter- and intra-rater reliability, and could be used to screen for excess malnutrition. Despite all these advantages, it is essential to bear in mind that there are still no established NC percentiles for each age and sex, nor do we have defined cut-off points to diagnose overweight/obesity.
This study is carried out in children living at high altitudes, where NC is used as a screening tool to identify malnutrition by excess in school age children; we did not find other studies for the same age population living at high altitude.
We hope to encourage the development of new studies in these particular settings which include a large population and, in the future, analyze its association with metabolic syndrome and other chronic pathologies.