INTRODUCTION
Cleft lip and/or palate (CL/P) are a type of congenital anomalies that affect one per 700-750 newborns and are caused by embryological defects in the formation of the upper lip and palate during the early stages of pregnancy (1). In addition to the stigmatizing aesthetic defect, CL/P associate feeding and breathing problems, ear infections and hearing loss, speech pathology, and dental and developmental problems of the jaws (2,3). Therefore, these patients require, on the one hand, a multidisciplinary approach (surgical, orthopaedic, orthodontic, otorhinolaryngological, phoniatric and psychologic) that must be done early in life and, on the other hand, a prolonged follow-up both to avoid functional impairment and to allow normal development of the child (4). There are several classifications but, overall, the cleft may affect the lip, the palate or both, and they can be unilateral or bilateral (5).
In children with CL/P, nutritional status can be affected because of feeding difficulties, mainly due to their anatomy and the surgical interventions themselves, as well as airway and middle ear infections (6,7). Consequently, these patients may have impaired growth and development during their first months of life, more or less marked depending on the type of cleft, and they may need nutritional support and aid with feeding practices (8,9). However, after two years of age, the nutritional prognosis and growth trajectories in most of them are similar to those of their peers (10,11).
The available studies on long-term growth and nutritional outcome of children with CL/P are scarce in the literature but, despite the fact that the nutritional prognosis seems to improve from two years of age (12-14), there is not enough conclusive evidence about their growth and body composition patterns during childhood (15). Furthermore, CL/P populations are from very different geographical origins and only a few of the existing studies, about long term growth prognosis of CL/P patients, have compared anthropometric measurements of CL/P children with their counterpart healthy controls (15-17). Thereby, more studies are needed to assess longitudinal growth, from birth to childhood, of those children with higher nutritional risk and the long-term consequences on their nutritional status and body composition. This article aims to analyse the growth trajectories of a cohort of Spanish children with isolated cleft lip and/or palate (without pathology or associated syndrome) who required surgical intervention and to compare them with international standards and with a healthy representative cohort of children from Aragón.
MATERIAL AND METHODS
STUDY DESIGN AND SAMPLE SIZE
This is a study with a retrospective longitudinal design in which the medical records of the patients seen in the Children’s Oral and Maxillofacial Surgery consultation of a reference hospital born between 2009-2014 were reviewed. The selection criteria were: patients with a diagnosis of cleft lip, cleft palate or cleft lip and palate born in that period. In each of the selected patients, data collected were sex, date of birth, type of cleft, date and type of intervention, surgical technique and sequelae, as well as weight, length (height) and body mass index (BMI) (weight/size2) at different ages (0-6 years). Sixty patients born between 2009 and 2014 were initially reviewed with a diagnosis of CL/P, from which 41 patients (21 male and 20 female) were finally selected because they had full longitudinal registration of anthropometric measurements in their medical records and they did not associate any pathology or syndrome.
A cohort of Spanish children participating in the Growth and Feeding during Infancy and Early Childhood in Aragon (CALINA) study (18,19), born in the same year (2009), were used as control group. CALINA is an ongoing birth cohort study whose sample is a representative cohort of our population. CALINA’s study main objective was to assess growth patterns, body composition and feeding aspects in infants and children and to examine prenatal, postnatal and sociocultural factors which may influence them. The cohort was randomly drawn from births occurring from March 2009 to February 2010 in different localities in the region of Aragon (Spain), recruited from Primary Care centres by trained paediatric staff and with compliance and attendance over 80 % of the population living in this area.
One thousand six hundred and thirty families were contacted to participate in the CALINA study and 1,602 families accepted to participate. After eliminating children with any malformation, diseases or physical disabilities and without information on sex, birth weight, length at birth, and date and place of birth, a total of 1,540 new-born infants were examined at birth and periodically re-examined at two weeks, monthly and yearly. After the six-year follow-up, 323 children no longer participated in the study (retention rate 79 %). Children with missing values in exposures, covariates or outcomes at baseline or follow-up were excluded. Asians were not included because models could not run satisfactorily due to the small size of the sample that led to unstable results. Finally, the analysis included 1,031 children (19).
Research project in CL/P patients and CALINA study were both approved by the Aragón Clinical Research Ethics Committee.
ANTHROPOMETRIC MEASUREMENTS
Anthropometric measurements in CL/P patients were obtained through the data collected in their electronic medical records. Length/height, weight and BMI were registered at the ages of one, three and six months and at one, two, four and six years old. Normalized age- and sex-specific anthropometric Z-score values were calculated in both studies (CL/P children and CALINA) by using child growth standards tables of the World Health Organization (WHO) (20,21).
STATISTICAL ANALYSIS
The data were entered into a database and analyses were conducted using the statistical software package IBM SPSS Statistics Version 26. A descriptive analysis was carried out using mean and standard deviation (SD) for continuous variables and frequencies and percentages for categorical variables. Differences in continuous and categorical anthropometric variables between CL/P and CALINA groups were compared using Student’s t tests and Chi-squared analyses, respectively. The criterion for statistical significance was set at p < 0.05.
RESULTS
Forty-one patients were finally included, 21 male and 20 female. Different types of clefts were intervened: 9.75 % cleft lip (n = 4/41), 41.46 % cleft palate (n = 17/41) and 48.78 % cleft lip and palate (n = 20/41). In addition, 59.8 % (n = 25/41) were operated from the first surgical time, 6.9 % (n = 3/41) from the second surgical time, 16.1 % (n = 6/41) were operated on sequelae and 17.2 % (n = 7/41) had several interventions. The average age at the time of the first intervention was seven months (SD = 1.58) in the cleft lip and 12 months (SD = 2) in the cleft palate. In reference to sequelae, in cleft palate and cleft lip palate patients (n = 37), pharyngoplasty was performed due to velopharyngeal incompetence in 18.91 % (n = 7) at an average age of 5.9 years (SD = 1.89), and 21.62 % (n = 8) presented palatal fistula. In cleft lip and cleft lip palate patients (n = 24), 20.83 % (n = 5) were reoperated for labial sequelae.
Anthropometry (weight, length/height and BMI) mean Z-scores at each age and gender in CL/P patients and gender differences are shown in table I. There are no statistically significant differences between boys and girls at any age and in any of the variables. Mean anthropometric Z-scores were low in both sexes during the first year of age but all measurements seem to progressively reach normality later (Table I and Fig. 1). In fact, when trajectories of growth Z-scores parameters of CL/P infants are compared with those from the CALINA study, mean weight and BMI Z-scores are both significantly lower at one, three and six months of age but not at one year or later (Fig. 1A and C). The highest differences in terms of weight and BMI Z-scores are at the age of three months when CL/P subjects showed lower values, recovering from that moment until the age of one year. Although the length is also low during the first months, it does not show statistically significant differences compared to the control group at any time (Fig. 1B). Thus, it can be seen that length is slightly affected in infants with CL/P.
Table I. Anthropometry at each age and gender in CL/P patients.
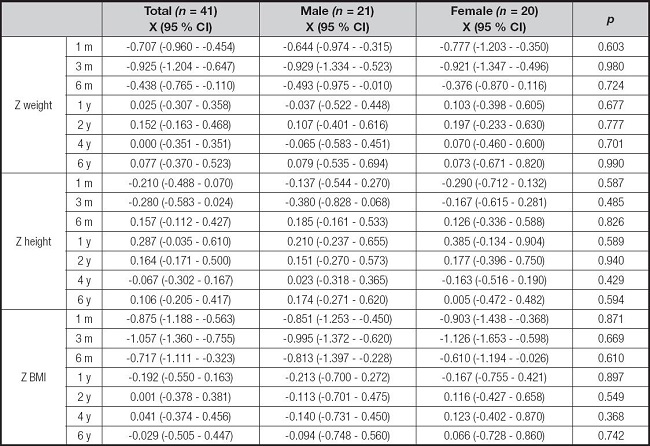
Z: Z-score; BMI: body mass index; CI: confidence interval; y: year; m: month.
Statistical significance was set at p < 0.0.
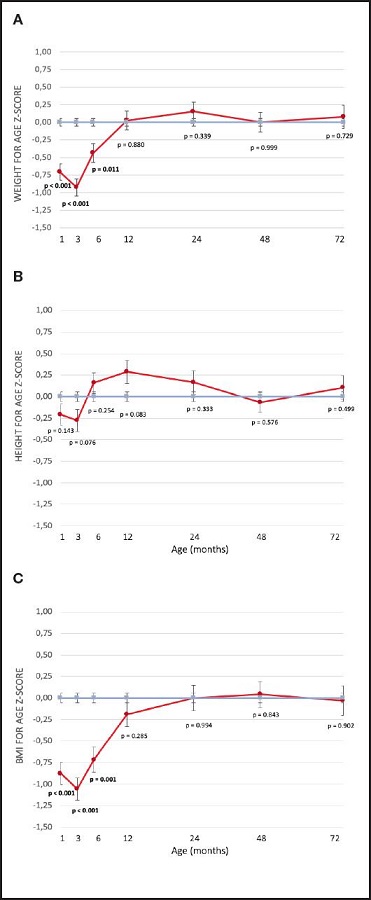
Figure 1. Anthropometry charts for weight, height and body mass index (BMI) Z-scores of cleft lip and/or palate (CL/P) patients compared with CALINA study children. A. Anthropometry chart for weight Z-scores of CL/P patients compared with CALINA study children. Statistical significance was set at p < 0.05. B. Anthropometry chart for height Z-scores of CL/P patients compared with CALINA study children. Statistical significance was set at p < 0.05. C. Anthropometry chart for BMI Z-scores of CL/P patients compared with CALINA study children. Statistical significance was set at p < 0.05.
The percentage of CL/P patients with a Z-score lower than -1 for weight, length/height and BMI has been compared at each age with controls in figure 2. The proportion of CL/P patients that could be at nutritional risk is significantly higher during the first months of age based on weight (Fig. 2A) and BMI (Fig. 2C). At three months of age, when the differences are greater, 44.44 % and 50 % of CL/P patients had respectively a weight and BMI lower than -1 Z-score, compared with 15.54 % (p < 0.001) and 12.79 % (p < 0.001) in controls. Although these differences become smaller, the percentage of CL/P patients with low BMI remains higher than that of controls at 2-6 years of age (7-10 % higher) with statistical differences at six years of age (p < 0.05) (Fig. 2C). Regarding length, no statistically significant differences were found at any age in comparison with controls (Fig. 2B).
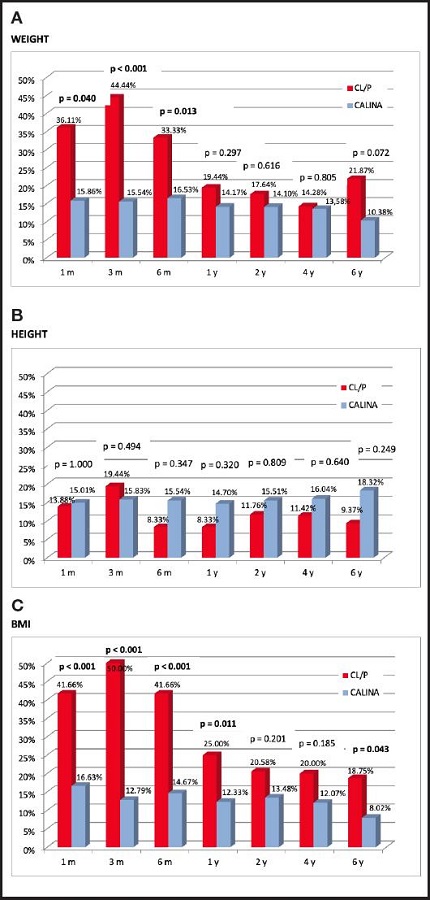
Figure 2. Percentage of children with weight, height and BMI less than -1 Z-score in CL/P and CALINA samples. A. Percentage of children with weight less than -1 Z-score in CL/P and CALINA samples. Statistical significance was set at p < 0.05. B. Percentage of children with height less than -1 Z-score in CL/P and CALINA samples. Statistical significance was set at p < 0.05. C. Percentage of children with BMI less than -1 Z-score in CL/P and CALINA samples. Statistical significance was set at p < 0.05. BMI: body mass index; y: year; m: month; CL/P: cleft lip and/or palate.
DISCUSSION
This study, with a retrospective longitudinal design, aims to analyse the growth trajectories of children, from birth to six years of age, with isolated CL/P (without associated pathology or syndrome) born between 2009-2014, and to compare them to their counterparts. The highest nutritional risk in CL/P patients takes place at 3-6 months of age but nutritional status and growth trajectories get recovered from one year of age compared to their counterparts. Nevertheless, the rate of thin subjects among CL/P patients is higher during childhood. The presence of these congenital orofacial malformations may influence negatively the nutritional prognosis of CL/P patients and, consequently, alter growth and development mainly during infancy (6,7).
In a recently published systematic review about long term growth patterns in CL/P patients, there were only six studies which analysed their nutritional prognosis during childhood and growth patterns from two years of age (15). The selected studies in this systematic review showed very varied results: three of them found some growth differences between cleft children and their counterparts (16,17,22) but the other three did not (13,23,24). Moreover, different groups of clefts were considered in each of these studies, diverse outcome measures were assessed and patients came from varied origins (three from Latin America, one from the United States, one from Asia and one from Europe) (15). In all of the previously reported studies about growth trajectories from two years of age in CL/P patients, anthropometric Z-scores were calculated (15); however, only in two of them and with a cross-sectional design, one in Colombia and the other one in Sweden, CL/P measurements were compared with controls (16,17). Thus, to our knowledge, ours is the second study that assesses growth trajectories in CL/P patients in Europe from two years of age, comparing them with controls, and the only one that does so worldwide in a population-based cohort study.
Our results are in agreement with what was previously published in children under two years of life (8,12,25,26). Below this age, there is a risk of malnutrition due to feeding difficulties, due to their anatomy and the surgical procedures themselves, as well as airway and middle ear infections (26-29). In our study, that happens especially during the first half year of age and the recovery, in terms of mean anthropometric trajectories, seems to be reached at one year of age. In fact, when the percentage of children with weight, length and BMI less than -1 Z-score (risk of malnutrition) has been analysed in our study, about half of children with CL/P are at risk of undernutrition at six months of age but later, from the first year of life, there are no statistical differences comparing with controls. However, the percentage of children with BMI less than -1 Z-score during childhood tends to be higher than in their peers (7-10 % higher), indicating that there are proportionally more thin children in the CL/P group than in the reference population.
On the other hand, it would seem reasonable to hypothesize that in these patients, in which growth restriction is evident during the first months of life due to early undernutrition followed by a later rapid weight gain, overweight and/or obesity risk could be increased in the long term as a compensatory response, either due to the effects of “metabolic programming” and/or by an excess of family insistence that they eat beyond their needs. However, no data supporting this hypothesis have been found in our sample (19,30,31).
In terms of growth recovery, our results after one year of age may reflect that nowadays in our healthcare environment, with the appropriate multidisciplinary management of these children, they get comparable to their healthy counterparts. This satisfactory outcome happens earlier than in other studies from Uganda or Syria (14,32,33). However, there is still much to improve in the first year of age in CL/P patients, especially during the first six months, when feeding difficulties are more relevant and it is just the time before the first surgeries are usually done. It is in this period when our sample had the highest rate of undernutrition, indicating a poor health outcome and a disadvantage to face the surgery.
Looking into growth trajectory differences between the types of clefts, the sample was not big enough to analyse them in this study because there were only four patients with isolated cleft lip. In this regard, it has been reported that the more extensive the cleft, the more functional impairment there will be. Patients with cleft that affect only the lip should not have difficulty with breastfeeding (34). However, children with unilateral or bilateral complete cleft lips, as well as those with cleft palate, may have difficulties in feeding more frequently, mainly because the cleft lip can compromise sucking during breastfeeding while the cleft palate can cause milk to pass into the nasal cavity (6,7,27,35).
The main limitation of this study might be its sample size. However, this sample offers a current representative population of CL/P patients, followed up longitudinally in our health area, and controlled by the same specialized staff. This sample included all patients attended at the third-level reference hospital of our region for the management and treatment of patients with CL/P. The final number of patients is not so high as to perform more complex statistical analyses, but it does represent the global universe of the sample and it gives a real view of our results about this topic.
As strength of this study, it should be highlighted the fact that age- and sex-specific anthropometric Z-scores were calculated for each patient and, besides, that these data were compared with our own control sample of healthy counterparts (18). These aspects have allowed us to normalize the anthropometric measurements throughout the study period (from birth to six years old) in both sexes, to have a longitudinal view of each variable with respect to an international standard (WHO) and, at the same time, to compare them with real and current measurements of a control group.
From the results of this study, we can conclude that in Spanish children with CL/P there were no differences in growth between sexes. Their nutritional status and growth trajectories get recovered from one year of age compared to their healthy counterparts. The highest nutritional risk in these patients takes place at 3-6 months of age, when more efforts have to be done to improve feeding aspects and nutritional prognosis, in order to get the patient ready for surgery in the best conditions. During childhood, growth trajectories of CL/P patients are appropriate and similar to those of their counterparts. The rate of thin subjects among CL/P patients is higher during childhood but further larger studies are needed to confirm the long term consequences of these malformations on final growth and body composition later in life.














