INTRODUCTION
Docosahexaenoic acid (DHA or 22:6n-3) is an omega n-3 polyunsaturated fatty acid (PUFA). Chemically, it is a carboxylic acid like all fatty acids (FAs). DHA is considered as the most important long-chain PUFA of the n-3 family. Physiologically, the human body is able to metabolize DHA through conversion in the organism of alpha linolenic acid (ALA), another n-3 PUFA. This conversion takes place principally in the liver and it is transported as a phospholipid by plasma albumin, almost exclusively, to the brain and retina. In cases of pregnancy, adipose tissue also acts as a temporary reserve, but the degree of conversion is reduced, making it difficult to meet recommended levels of DHA, considered to be an essential prenatal nutrient (1). For this reason, the European Food Safety Authority (EFSA) (2) recommendation ranges from 100 to 200 mg/day.
Factors that can influence low DHA intake in pregnant females include level of education, older age, smoking and insufficient fish and seafood consumption, especially in the second and third trimesters (3). DHA is found in fish oil and some algae. In turn, most DHA in fish and other complex organisms comes from their access to photosynthetic heterotrophic microalgae. Foods that contain it include cold-water fish (like salmon, herring or anchovy), tuna and codfish oil (1). As it can be difficult to reach the recommended amounts through dietary intake, the consumption of DHA supplements with or without other FAs is advised. It should also be noted that omega-3 fatty acid supplements are well tolerated by pregnant and lactating women (4).
In this group of women, this n-3 PUFA participates in different functions (5,6). In terms of mental health, significantly lower levels of DHA, EPA and total n-3 PUFAs have been found in adult patients with depression, suggesting that n-3 PUFAs play a role in the pathogenesis of this illness (7), participating in neurobiological processes including control of serotonergic and dopaminergic function, modulation of brain-derived neurotrophic factor in the hippocampus, regulation of the hypothalamic-pituitary-adrenal axis, and with effects on neuroinflammation (8). In this regard, Lin et al. (7) argued the need for studies examining the specific functions of DHA in different population groups with depressive symptoms. In this context, the present study focuses on maternal mental health.
One possible solution to mental health issues in such situations is the application of prescription drugs. However, because of their potential toxic, teratogenic or even lethal effects on the fetus, the use of many of them is not recommended during pregnancy. In addition, the physiological changes inherent to pregnancy and lactation condition the absorption, transfer, excretion and metabolism of antipsychotics (9). For this reason, nutrition-based treatments have been proposed as an aid to alleviate and/or prevent prenatal anxiety and depression (10). There is therefore an evident need to know the real effect of DHA on mental health during pregnancy and the postpartum period.
Nonetheless, despite the findings of the referenced studies, the relationship between DHA and its effect on mental health in the prenatal stage is not fully clear (7). It can be speculated that different actions can occur simultaneously. On one hand, by maintaining and increasing the brain structures and preserving their function by interacting with phospholipid metabolism and, hence, the modulation of signal transduction. On the other hand, preventing or decreasing the inflammatory status occurring during depression (11). The aim of this scoping review is therefore to evaluate the effect of DHA during pregnancy and the postpartum period on maternal mental health in terms of depressive symptoms and anxiety.
MATERIAL AND METHODS
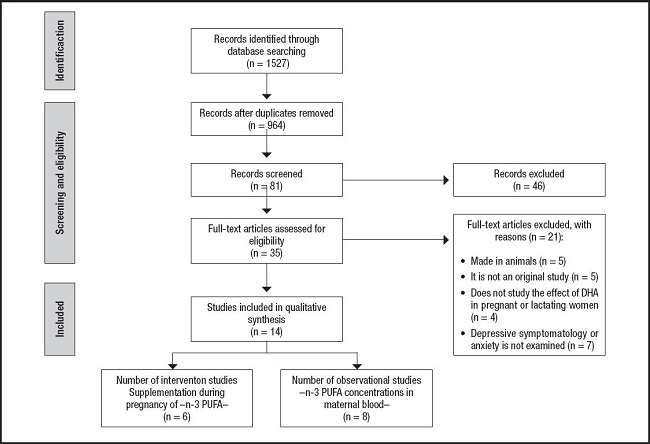
The scoping review framework adopted was based on the methodological model of Arksey and O’Malley (12), with contributions from the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (13). Following the model, the methodological process was divided into five stages.
IDENTIFYING THE RESEARCH QUESTION
The research question that was formulated was as follows: what are the effects of DHA during pregnancy and the postpartum period on maternal mental health in terms of depression and anxiety?
IDENTIFYING RELEVANT STUDIES
Relevant studies were identified by searching recent literature published between February and March 2021 in the PubMed, Scopus, PsycINFO and Medline databases. The following keywords were used: “Docosahexaenoic Acid”; “Fish Oil”; “Dietary Supplements”; “Pregnancy”; “Maternal-Fetal Exchange”; “Breast Feeding”; “Depression; “Depression, Postpartum”; “Mental Health”; “Behavioral Symptoms”; “Stress, Psychological”; “Affective Symptoms”; “Anxiety”; “Postnatal depression”; and “Antenatal depression”.
Articles included in this scoping review met the following specified inclusion criteria: a) analytical studies (i.e., randomised controlled trials [RCT], or mainly observational studies [cross-sectional, cohort and case-control]); b) evaluating the effect of DHA on mental health (depression and anxiety) in pregnant and/or lactating women; c) published in English or Spanish; and d) published between January 2010 and March 2021. The healthcare level at which the study was carried out was not considered as relevant. Studies which were carried out on animals or which focused only on other n-3 PIFAs were excluded.
STUDY SELECTION
Study selection was carried out as described above and following PRISMA (14). First, the search results were imported into Mendeley (https://www.mendeley.com) to perform the duplication check, thus eliminating 563 articles. Of the remaining 964 studies which were subsequently analyzed according to title and abstract, 883 were discarded based on the inclusion and exclusion criteria, while 81 were found to be potentially eligible articles. Subsequently, the relevance of each of the abstracts was analyzed, eliminating 46 in this process. Finally, the full text of the remaining 35 articles was examined and 14 were chosen for final analysis (Fig. 1). The entire process was recorded using an Excel Information Manager spreadsheet (15).
CHARTING THE DATA
Four specific components were extracted using a standardised form: a) general data (author[s], year of publication and country); b) methodological elements (study design and population); c) data of the intervention/observation carried out (i.e., dose of DHA, measurement of the presence of depression and/or anxiety, etc.); and d) data evaluating the effect of DHA on the mental health of pregnant and/or lactating women.
RESULTS
The results are set out in three different sections: characteristics of the included studies, studies which show the effectiveness of DHA in terms of maternal mental health, and studies which show no such effectiveness.
CHARACTERISTICS OF INCLUDED STUDIES
The 14 papers came from a total of 11 countries: two from Brazil, United States and Japan; and one each from Australia, The Netherlands, Iran, Kenya, Mexico, Norway, United Kingdom and Taiwan. Exactly half of the papers were published between 2016 and 2018 (n = 7). As for the type of study, six were RCT, four were prospective cohorts, three were cross-sectional studies and one, a longitudinal case-control study. These and other characteristics of the studies are shown in table I.
Table I. Overview of included studies.

DSM-IV: Diagnostic and Statistical Manual, 4th edition; IG: intervention group; CG: control group; WG: gestation week; DHA: docosahexaenoic acid; EPA: eicosapentaenoic acid; STAI: State-Trait Anxiety Inventory (Spanish version); EPDS: Edinburgh Postpartum Depression Scale; FA: fatty acids; ALA: alpha-linolenic acid; BDHQ: self-administered diet history questionnaire; CES-D: Center for Epidemiologic Studies Depression Scale; PDSS: Postpartum Depression Screening Scale; HIV: human immunodeficiency virus; n-3: omega-3; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; sFFQ: semi-quantitative food frequency questionnaire; n-3 PUFA: omega-3 polyunsaturated fatty acids.
STUDIES THAT REPORT EFFECTIVENESS OF DHA WITH RESPECT TO MATERNAL MENTAL HEALTH
Of the 14 analyzed papers, nine found that the consumption of either DHA alone or in combination with other FAs during pregnancy was beneficial for maternal mental health. Of these, six (16-21) measured plasma levels in the mother while only three (22-24) studied dietary supplements during the pregnancy.
With respect to the consumption of DHA alone, without other FAs, this was only performed by Judge et al. (23). Significantly lower scores (p = 0.016) were recorded on the Postpartum Depression Screening Scale in the IG (46.03 ± 2.17) compared to the control group (CG) (52.11 ± 2.4).
The effect of the combination of DHA with other FAs has also been studied. Daily intake of DHA varied between 70 mg/day and 325 mg/day and the prevalence of depressive symptoms between 5.8 % and 33.7 % (16-18,21). Pinto et al. (17) reported a 5 % decrease in the probability of having depressive symptoms for each one-week increase in the pregnancy. In all (16-18,21), it was found that pregnant women with lower dietary intake and blood concentrations of DHA had higher scores on the Edinburgh Postpartum Depression Scale (EPDS) (p < 0.05). Likewise, lower plasma concentrations of other FAs, such as EPA (16-18,21), docosapentaenoic acid (DPA) (17,21), total n-3 (17,21), the n-3/n-6 ratio and highly unsaturated fat (21) were correlated with higher scores on the EPDS. Finally, it should be noted that no statistically significant results were obtained for the postpartum period (20,21). As for anxiety, Álvarez-Ramírez et al. (16) reported a prevalence of 44.4 % (STAI > 40 points) and an increase in the STAI score for pregnant women with a lower intake of DHA and EPA (p = 0.03).
Two observational studies carried out a follow-up of a group of pregnant females diagnosed with perinatal depression (IG) and another with no prior pathology (CG). In the first of these, Chang et al. (19) found that the IG had significantly lower levels of DHA (p = 0.020), total n-3 (p = 0.026), and EPA (p = 0.019). In the second study (20), an 11.5 % prevalence of perinatal depression was found, along with a positive association between DHA and EPA, and perinatal depression. However, as in the previous cases, no statistically significant correlations were found between DHA and EPA plasma concentrations and postnatal depression.
The final two papers that reported a beneficial effect of DHA were RCTs. In the first of these (22), after the follow-up it was found that fish oil supplements significantly reduced the mean EPDS score during pregnancy (p < 0.05). In the second study, Mozurkewich et al. (24) used two IGs and a CG (with soybean oil). EPA-rich fish oil was administered to the first IG and DHA-rich fish oil to the second. At the third of four visits (at 24-36 weeks’ gestation), the Beck Depression Inventory (BDI) score was significantly predicted by serum DHA (p < 0.05), BDI at enrollment (p < 0.001) and admission to having stopped taking the capsules (p < 0.01). None of the three dietary supplements significantly predicted the BDI scores at 6-8 weeks postpartum.
STUDIES THAT REPORTED NO EFFECTIVENESS OF DHA WITH RESPECT TO MATERNAL MENTAL HEALTH
In this section, a description is offered of the five studies which reported no beneficial effect of DHA on maternal mental health. In the observational studies, an analysis was undertaken of the concentration of n-3 PUFAs in blood samples. In the most recent of the studies, carried out by Urech et al. (26), a longitudinal follow-up was made of four groups of pregnant women. Mean scores increased more in the groups with a mental disorder than in the healthy group (CG). Moreover, women with a major depression disorder did present lower levels of n-3 (p = 0.018) and EPA (p = 0.006), and those diagnosed with a mixed anxiety-depression disorder had lower levels of EPA (p = 0.015) and higher levels of DPA (p = 0.001). No statistically significant association was found between the anxiety disorder group and any FA. In addition, no FA was significantly associated with postpartum depression. In the other observational study (27), a total of 967 women were screened for postpartum depression. Depression was recorded in 19.8 % of the women one month after delivery, a value which fell to 12.8 % at six months. No significant associations were observed between postpartum depression and intakes of DHA, EPA and n-3 PUFA.
Just one study, that of Makrides et al. (28), administered only DHA supplements (800 mg/day) to an IG. No significant differences were found between the percentage of women who reported depressive symptoms during the first six months postpartum in the IG and CG (9.67 % against 11.19 %; adjusted OR 0.85; 95 % CI: 0.70-1.02; p = 0.09). Depressive symptoms were commoner among women with a prior or current diagnosis of depression at enrolment.
The two RCTs in which DHA was studied in combination with other FAs were published by Opiyo et al. (29) and Dos Santos Vaz et al. (30). In the first of these (29), all participants were HIV-positive pregnant women. At the end of the follow-up, most of the participants had mild depressive symptoms (95.3 % in the IG and 97.9 % in the CG), with the difference not being statistically significant. Finally, in the study by Dos Santos Vaz et al. (30), depression was detected using the EPDS (≥ 11 points) in different gestation weeks. At weeks 30-32 of gestation, the IG had higher serum concentrations of EPA, DHA and lower n-6/n-3 ratio compared to the CG. However, there were no differences between the IG and CG in the prevalence of EPDS scores over time. Only women in the IG with a previous history of depression had a higher reduction in the EPDS score between the second and third trimester compared to the CG (p = 0.038). In their conclusions, the authors argued that a daily dietary supplement of 1.8 g of n-3 PUFAs during 16 weeks had no effect in terms of preventing maternal depressive symptoms.
DISCUSSION
The results were classified according to whether the studies showed beneficial effects or otherwise of the intake of DHA during pregnancy on maternal mental health in terms of depressive symptoms and anxiety. The observational ones almost all show that the DHA has an important effect in relation to maternal mental health (6 yes, 2 no). On the other hand, the experimental ones do not show that effect so clear (3 yes, 3 no). This lower effect in the experimental ones may be due to various causes (i.e., the different doses, the sample size and even the different countries in which the studies have been performed, since it is known that there are clear differences in diets [31].
According to the analysis of the papers that has been undertaken, dose is one of the conditioning factors that may affect the effectiveness of DHA. Different doses were administered in the RCTs (22-24) (Table I). These doses meet the recommended daily DHA intake of the EFSA (2) (a range from 100 to 200 mg/day). It should also be noted that the effectiveness of DHA reported in these studies may be affected by the exclusion criteria of a prior history of depression, anxiety or certain other illnesses.
In other RCTs with higher doses of DHA, no beneficial effect on mental health was reported, though this may be due to how the studies were developed. In the case of Dos Santos Vaz et al. (30), the inclusion criteria were a prior history or risk of depression. Likewise, in the study of HIV-positive pregnant women (29), the illness itself could imply a bias in the results given the different physiological and psychological conditioning factors of this group of women. Finally, it should be noted that in the study by Makrides et al. (28), a dietary DHA supplement of 800 mg/day was found to be ineffective in the prevention or reduction of depressive symptoms. However, as limitations to their study, the authors reported that they did not verify the clinical diagnosis of depression before the start of the RCT. In addition, they associated the lower than expected rate of depressive symptoms in the CG to the so-called Hawthorne effect (33), according to which the mere fact of participation in a trial with a high degree of contact with researchers helps to prevent such symptoms. Finally, in relation to the non-effectiveness of DHA in pregnant women with an established diagnosis of prenatal depression, a recent study by Mezquida et al. (34) reported the association of a specific pattern of obstetric complications with a more severe clinical symptomology like depression. All of this may be influential in terms of the results of the non-effectiveness of DHA in this population with a history of mental illness.
On the other hand, Makrides et al. (28) only analyzed the effect of DHA in the postpartum period, while the effectiveness of DHA was only found to be statistically significant in other studies during pregnancy (16-24). In this regard, a total of five studies (24,26-29) found, after analyzing the effect of DHA in the postpartum period, no positive effect in terms of the prevention or reduction of depressive or anxiety symptoms. This may be because the dietary supplements were administered during pregnancy and, therefore, the concentrations of DHA would have lowered considerably in the postpartum period. However, the importance of DHA for maternal mental health in the third trimester has been shown. This appears to be a critical period to ensure adequate levels of maternal DHA to facilitate optimal cognitive development at the end of infancy (35). In this regard, the potential effects of DHA during infancy and adulthood are becoming more widely recognized, suggesting at the same time that DHA levels can play a role in cognitive decline and in relation to the main psychiatric disorders (36). The effect may be related to the intake of DHA supplements increasing the concentrations of 17-hydroxy-docosahexaenoic acid in maternal and umbilical cord blood (p = 0.02) (37).
Finally, another conditioning factor that may have affected the results is the way depressive symptoms were measured. One of the scales used, in the study by Judge et al. (23), was the Center for Epidemiologic Studies Depression scale (CES-D) (38). In the study, a Cronbach's α coefficient of 0.89 in the IG and 0.90 in the CG was reported. A noteworthy result if compared with the original coefficients of 0.85 and 0.9, respectively (38). For this reason, Judge et al. (23) concluded that the maternal CES-D score during pregnancy was a significant predictor of postpartum depressive symptoms. This finding also supports previous research that identified psychological disturbance during the prenatal period as a significant predictor of postpartum depression (39,40). However, this scale was not used in the other studies, where the most commonly used scale was the EPDS (25) (n = 11). This scale measures depression and the emotional feelings of mothers in the last weeks of gestation. The prevalence of depression ranged between 5.9 % and 50 % (16-22,24,26-28,30). The EPDS has been used with different cut-off values (≥ 12 points, ≥ 11, ≥ 10, ≥ 9 and > 8) or simply the mean values. Although a high EPDS score (25) cannot confirm a diagnosis of depression, it is considered that a score higher than 12 may indicate a probable depressive disorder (28). A score of 10 to 12 represents a crossover point and a score of 0 to 9, the absence of postpartum depression (41). In contrast, Markhus et al. (21) argue that the cut-off value should be ≥ 10, as this is the value commonly used in Primary Care settings.
LIMITATIONS
The selected studies were carried out in different countries with large sociocultural and dietary differences, making generalizations difficult. In addition, there are important gaps in the body of knowledge with respect to the influence of other nutrient deficiencies (i.e., genetic polymorphisms that affect the synthesis of n-3 FAs and the total intake of FAs) or the real influence of other n-3 FAs (i.e., EPA) in maternal mental health. Data on dietary intake of fats and measures of fatty acid status in blood are not collected or, at least, not specified in most papers.
The studies are also limited in many instances by a small sample number or the inclusion/exclusion criteria that were used in relation to mental health issues prior to pregnancy. For the above reasons, the results of these studies cannot be considered to be conclusive.
CONCLUSIONS
This scoping review focuses on identifying the effectiveness of DHA with respect to maternal mental health. In most of the studies analyzed (n = 9), higher serum concentrations of this n-3 PUFA, whether due to a high natural intake or dietary supplements, were shown to influence reducing the prevalence of depressive and anxiety symptoms. Although more research is needed, these exploratory results therefore seem to indicate that DHA plays an important role in the prevention of the pathogenesis of these two mental illnesses during the gestation period. However, it appears to lose effectiveness in the postpartum period, since no studies analyzed in this review had shown an effect of DHA on depressive or anxiety symptoms. The findings lend support to the hypothesis of the implication of phospholipids in depression. However, further research in this area is required. Future investigations should aim to replicate findings in larger data sets and clarify possible pathophysiological mechanisms. Another research line would be to investigate what happens with multiple pregnancies given that all the studies made to date have concentrated on singleton pregnancies. It should also be noted that very few of the papers have considered only the use of DHA, with most studying DHA in combination with other PUFAs like EPA. Further research is therefore required to know the individual effect of DHA on maternal mental health.
Finally, different scales were used to detect depressive symptoms, with the EPDS being the most frequently employed. However, there appears to be no consensus on the cut-off value. Clarifying this question is key in terms of the healthcare implications for the systematic detection of depression during pregnancy and the postnatal period and, in this way, ensuring early intervention and the correct tackling of the disorder.