INTRODUCTION
The effects of malnutrition on chronic diseases are significant, leading to prolonged hospital stays and higher healthcare costs because of increased morbidity and mortality (1). Enteral nutrition (EN), defined as the digestive administration of formulas or blenderized food through a feeding tube to the stomach or intestine, is an effective medical procedure to fulfil nutritional requirements for patients unable eat or to reach them orally (2). EN is effective in reducing malnutrition and restoring patients' nutritional status, improving their quality of life (QoL). According to the European Society for Clinical Nutrition and Metabolism (ESPEN) guideline, the main indications of EN include swallowing disorders because of neurological diseases and obstruction due to malignancies (3,4).
EN can be initiated during a hospital stay or, occasionally, in outpatients, and continued at home or another community setting. Home enteral nutrition (HEN) reduces hospitalization periods for patients requiring tube feeding support, reducing the probability of infections and healthcare costs (5-7). Moreover, HEN facilitates functional patients to live at home surrounded by their social environment and improves their QoL (8,9). HEN is also recommended when there is no effective treatment for the underlying condition, considering all related ethical aspects (3). Nevertheless, HEN should always meet the patients' nutritional requirements, and the access devices should be adapted to the patient's situation. Since their first introduction in the 1940s, ready-made formulas have provided all macro and micronutrients required, with different formulations available to adapt the treatment to the patient's needs (3,10).
Given the increase of HEN administration during the last decades, parallel to the increase in the incidence of chronic diseases, a registry of the treatment conditions would allow to analyze the differences between countries and the impact on their health systems. In the United States, the estimated prevalence of HEN administration increased from 597 patients per million in 1992 to 1,382 in 2013 (11), while in Europe, the prevalence was estimated to be lower (163 patients/million in 1998) (12), with substantial differences between countries.
In Spain, the HEN voluntary registry of NADYA-SENPE (13) has shown an increase in HEN prevalence since 1994, stabilizing over the last five years at around 100 patients/million inhabitants. However, some regional studies estimated HEN prevalence to be higher (14-17). The most common causes of HEN are neurological diseases, and the preferred administration method is gastrostomy (13).
Several studies were focused on the role of HEN in different clinical scenarios and its impact on QoL (18), but the evidence focused on the components of enteral formulas and patients' and specialists' preferences are limited (19,20). Detailed knowledge of the patient profile requiring each formula could improve adherence to treatment and patient satisfaction. The goal of the ECONES study was to describe the treatment of patients requiring HEN in routine clinical practice and the experience with the high-protein hypercaloric formula 2.0 with fiber IS50 (HP/HC 2.0) from the specialists' perspective.
METHODS
ECONES was a multicenter ecological study. The source of aggregated data was the knowledge and experience of specialists with experience treating patients with home enteral nutrition (HEN) and HP/HC 2.0 formula. The data were collected through an on-line survey. Given the ecological nature of the study, no data were extracted from clinical charts, and all treatments were prescribed following routine clinical practice and were not altered by the participation of the specialists in the study.
This study was conducted at hospitals in Spain and approved by the Ethics Committee of the Hospital Clínico San Carlos (Madrid, Spain).
SURVEY AND DATA COLLECTION
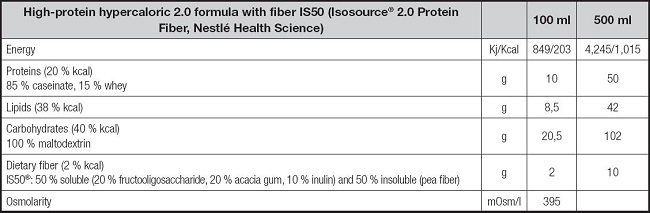
The survey was composed of 38 questions and answered by specialists between August 2021 and February 2022. Six questions were oriented to collect information about the specialists, 12 questions aimed to characterize the last six patients with HEN and 20 were about the percentage of patients treated with high-protein hypercaloric 2.0 with fiber IS50 (HP/HC 2.0) (Isosource® 2.0 Protein Fiber, Nestlé Health Science) enteral formula (Table I) at home.
STATISTICAL CONSIDERATIONS
A descriptive analysis of the responses was performed. Frequencies of qualitative variables were calculated and presented as percentages. For questions referring to the frequency of patients reported by the participants, mean and standard deviation (SD) were calculated. The statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) version 28.01.1 (SPSS Inc., Chicago, USA).
RESULTS
CHARACTERISTICS OF THE SPECIALISTS
The survey was answered by 82 specialists from different regions in Spain (Annex 1). Most specialists participating in the study had more than five years of experience (65.8 % had 6- 19 years of experience and 21.9 % had more than 20 years of experience). Fifty-eight were specialized in Endocrinology and Nutrition, eight in Internal Medicine and six in other specialties (n = 71). During the last month, the specialists (n = 81) treated a mean of 27.5 (25.9) patients with enteral tube feeding. Of those, a mean of 17.1 patients were hospitalized, while 9.9 were at home. The average duration of HEN was 9.6 (8.6) months.
PATIENTS TREATED WITH HOME ENTERAL NUTRITION
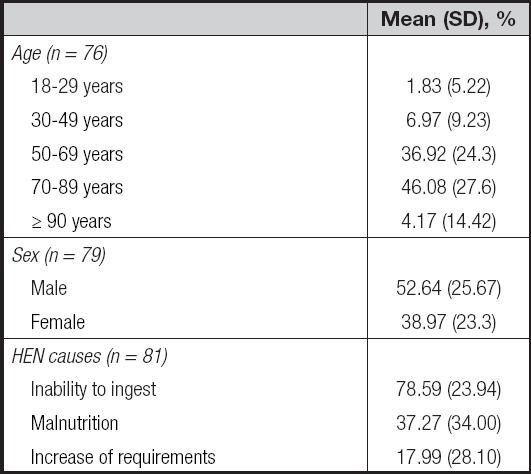
Most patients treated with HEN were older than 50 years, and a mean of 52.6 % (25.7) were male (Table II). A mean of 63.4 % (30.6) of patients required caregiver help. According to the specialists, the main reason for starting HEN was the inability to ingest orally, for a mean of 78.6 % (23.9) of patients (Table II).
The inability to ingest orally in patients treated with HEN was primarily caused by mechanical swallowing disorders produced by injuries, neoplasms, surgeries, or radiation therapy or by neuromotor swallowing disorders produced by neurological diseases for all patients treated with HEN, including those treated with HP/HC 2.0 formula (Table III).
Table III. Indication and administration of HEN.

*n = 80;
†n = 78;
‡n = 79.
HEN: home enteral nutrition.
When asked about the HEN administration method, the specialists claimed that it was mainly delivered by bolus, mostly through a syringe, and through gastrostomy (Table III). Moreover, in those patients treated with HP/HC 2.0 formula, the mean daily volume of EN was 935 (366.5) ml. On average, specialists recommended a mean daily volume of 1,033.8 (363.3) ml of water.
In addition, the specialists chose different formulas based on the patients' requirements, administering a high-protein hypercaloric polymeric < 2.0 kcal/ml formula to a mean of 44.1 % of patients and HP/HC 2.0 to 31.5 % (Table IV). These were supplemented with different volumes of water, being 1,094.4 ml recommended for hypercaloric 2.0 formulas (Table IV).
EXPERIENCE WITH HIGH-PROTEIN HYPERCALORIC FORMULA WITH FIBRE IS50 (HP/HC 2.0)
Specialists highlighted that the administration of HP/HC 2.0 was prescribed since the beginning of treatment for 42.2 % of patients. This formula was chosen because of the nutritional requirements increase (for a mean of 49.1 % [40.3] of patients), volume restriction (36.2 % [36.2]), fewer bolus administration (28.8 % [34.6]) or because of bronchial aspiration risk, reducing the nutrition volume in the stomach and gastric residual volume (12.2 % [28.2]). According to the specialists, most patients (89.8 % [23.4]) reached at least 75 % of the prescribed intake, and most patients (81.4 % [29.0]) improved their nutritional status.
The HP/HC 2.0 was also considered to be adequate based on the caloric and protein requirements according to 92.4 % of specialists, while 6.3 % considered it partially adequate and 1.2 % did not have the opportunity to prescribe it. Moreover, 93.7 % of specialists claimed that the HP/HC 2.0 formula was adaptable to patients' comorbidities.
According to the specialists, a mean of 48 % of patients treated with the HP/HC 2.0 formula was in good health status, and improvements were observed in social relationships (31.2 %), mood (41.2 %), and physical status (66.3 %).
SATISFACTION AND SAFETY
Specialists claimed that most caregivers (90.6 %) said that the HP/HC 2.0 was well tolerated by patients and that patients (or their caregivers) felt comfortable with the administration frequency (82.9 %) and administration time (75.3 %), feeling 78.7 % comfortable with the formula packaging characteristics.
The most common adverse events, according to the specialists, were diarrhea, bloating and constipation, being present in a median of 13.2 %, 11.2 % and 9.6 % of patients with any HEN and 6.6 %, 8.75 % and 6.3 % of patients treated with HP/HC 2.0, respectively. All reported adverse events are recorded in figure 1.
DISCUSSION
The ECONES study presents the perspective of Spanish specialists on using HEN in different situations and their experience with different available formulas, with 82 specialists providing aggregated information about their last six patients, which provides a perspective of the current routine clinical practice in Spain. Moreover, given its novelty, this is the first description of the experience with the HP/HC 2.0 with fiber IS50 formula tube feeding in Spain, yielding useful insights on how this formula is being used in real-world clinical practice.
The HEN increase in prevalence during the last decades (13) has probably been related to the development of new formulas and the improvement in administration devices, the awareness of the importance of malnutrition, and the new legislation (16,21). The NADYA-SENPE voluntary registry provides a picture of the HEN situation in Spain (13). According to their last report, the median age of HEN patients was 77.5 years in 2018 and 71 in 2019, in line with our results, as almost half of the ECONES patients were 70-89 years old. Similarly, in 2018-2019 around half of the NADYA-SENPE patients were male, as in our study. The specialists of the ECONES study claimed that more than half (63.4 %) of patients required a caregiver, as in the NADYA-SENPE registry (54 %). These results suggest that the answers collected in our study are aligned with previously published studies.
EN is indicated for those patients unable to fulfil nutrition requirements orally, or for those having difficulties in the proper transit of food from the mouth to the intestine. Patients with neurological diseases often require enteral nutrition, given the impairment of the neural pathways underlying swallowing activity. Similarly, some malignancies are usually related to swallowing problems. In these situations, enteral nutrition reduces infections, hospital stays and costs (22). Neurological diseases were the primary underlying condition according to the last NADYA-SENPE report (13), but according to the specialists in our study, the main indications for HEN were mechanical swallowing disorders produced by injuries, neoplasms, surgeries or radiation. These differences could be related to the selection of specialists with experience using the HP/HC 2.0 formula.
There are different options to administer HEN. Nowadays, nasogastric administration is recommended only for short periods (less than four weeks), whereas gastrostomy has become the preferred long-term administration system, as it limits several adverse events usually recorded with nasogastric tubes (2,10). Our results align with these recommendations, as gastrostomy was the administration system for most patients. Similarly, the recommendations on the mode of administration also changed during the last decades. Although according to a previous European survey (12), the preferred mode of administration was cyclic at that time, and bolus administration was rarely recommended as it usually led to gastroesophageal reflux, in our study, most specialists chose bolus for their patients, independently of the formula used. This trend could be related to the improvement in the devices during the last two decades, as fewer adverse events (AEs) have been registered with intermittent administration, and the QoL would improve, allowing the patient to resume normal activities.
The parameters considered before prescribing HEN also changed over time. Classic parameters such as weight loss, body mass index and biochemical parameters (albumin, lymphocyte count or cholesterol) were recently complemented by bioelectrical impedance analysis, dynamometry, muscular ultrasound, functional tests, and other parameters. These new considerations give a new perspective on the patient's nutritional status and facilitate the selection of the most suitable formula in each particular case (23), as shown in our results, where different formulas were chosen based on the patient's needs.
Our study focused on a high-protein hypercaloric 2.0 formula with fiber IS50 (HP/HC 2.0) (Isosource® 2.0 Protein Fiber, Nestlé Health Science). High-protein formulas with fiber have shown few gastrointestinal AEs, facilitating adherence (24). Moreover, high-protein hypercaloric formulas reduce the volume administered, which in the case of bolus administration involves reducing the amount of boluses throughout the day, and in the case of cyclic infusion administration, reducing the number of hours connected to the pump and this improving the patient's QoL (25). It is also useful in situations with significant fluid overload, such as heart failure, where the volume administered is an important factor in the course of the disease (26). Another group of patients that could benefit from this formula are those with high nutritional requirements such as acute pancreatitis, some neoplasms, cystic fibrosis, polytrauma or major burns (27-31). Accordingly, the main reasons for specialists' choice of this formula in the present study were the increased nutritional requirements and the volume restriction.
Although adverse events are relatively frequent, they are usually mild and can be resolved adjusting the treatment. Based on the answers of the specialists, the most common AEs were gastrointestinal (diarrhea, bloating and constipation), being less common in patients treated with the HP/HC 2.0 formula.
Our study presents limitations. We missed patients' and caregivers' opinions, as we based our analysis on aggregated data based on the specialists' experiences. As medical records were not reviewed, our results are also subjected to certain subjectivity given the potential recall bias. Although the results of our study are in line with those presented in the last NADYA-SENPE report (13), we cannot rule out a possible bias when selecting specialists from different regions and specialties to participate in the study. Moreover, these results may not represent the current situation in other countries, especially in those where formulas are not fully reimbursed by their health systems or where different ethical aspects on extending life for terminal diseases may apply.
The continuous improvement in formula components and packaging and new administration devices offer new solutions to patients requiring HEN. We presented a snapshot from the specialists' perspective, but more studies should follow to keep an updated view on the optimal treatment in each case and to create guidelines oriented to fulfilling nutrition requirements while minimizing the effect on patients' QoL.
In conclusion, according to the specialists, the formulas and the administration systems chosen constantly adapt to new options available and are selected based on patients' characteristics. The HP/HC 2.0 formula is used in patients with high nutritional requirements, allowing volume restriction, presenting few AEs and improving patients' QoL.